Copy link
Sentinel Events
Last updated: 06/27/2025
Key Points
- Sentinel events are unexpected occurrences involving death or serious physical or psychological injury, or the risk thereof.1,2
- Events are termed “sentinel” as they signal the need for immediate investigation and response.1
- Accredited hospitals are mandated to report sentinel events to national reporting systems, analyze root causes, and develop improvements in reliability, consistency, and performance.1,2
Introduction
- The Joint Commission (JC) adopted a sentinel event policy in 1996 to enhance safety and learn from these events.1
- The JC defines a sentinel event as a patient safety event that reaches a patient and results in:
- death;
- permanent harm (regardless of the severity of the harm); or
- severe harm (regardless of duration of harm).1
- The goals of the JC sentinel event policy are to positively impact care, focus on identifying underlying causes and developing risk reduction strategies, increase knowledge and awareness of sentinel events and their prevention, and promote public confidence in the accreditation process.1
- Sentinel events that must be reported to the JC are listed in Table 1, and events that do not require reporting are listed in Table 2.
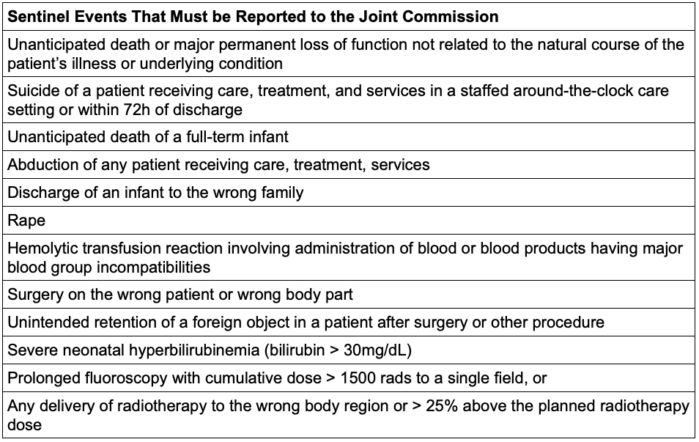
Table 1. Sentinel events that must be reported to the Joint Commission2
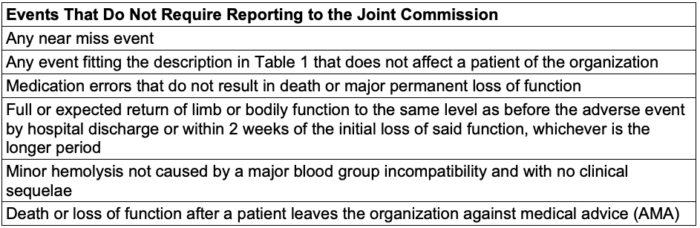
Table 2. Events that do not require reporting and review to the Joint Commission2
- Nearly all health systems worldwide run national reporting systems (Table 3), and most definitions incorporate two explicit elements: that the event be unexpected (or unintended) and that it has either caused harm or has the potential to do so.2
- Anesthesia-related sentinel events are relatively rare and are associated with significant consequences for patient safety and institutional accountability.2,3,4,5
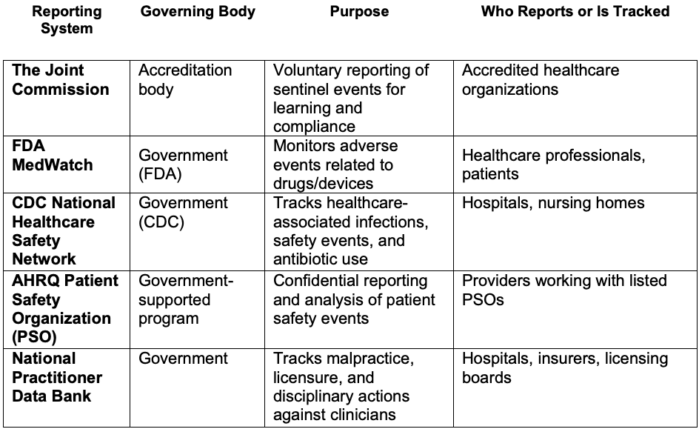
Table 3. National reporting systems for sentinel events. Abbreviations: FDA, Food and Drug Administration; CDC, Center for Disease Control and Prevention; AHRQ, Agency for Healthcare Research and Quality
Types of Sentinel Events in Anesthesia
- Advancements in monitoring, protocols, and training have reduced the incidence of anesthesia-related sentinel events.6
- Reducing sentinel events requires emphasizing communication, shared mental thinking, and vigilance.7
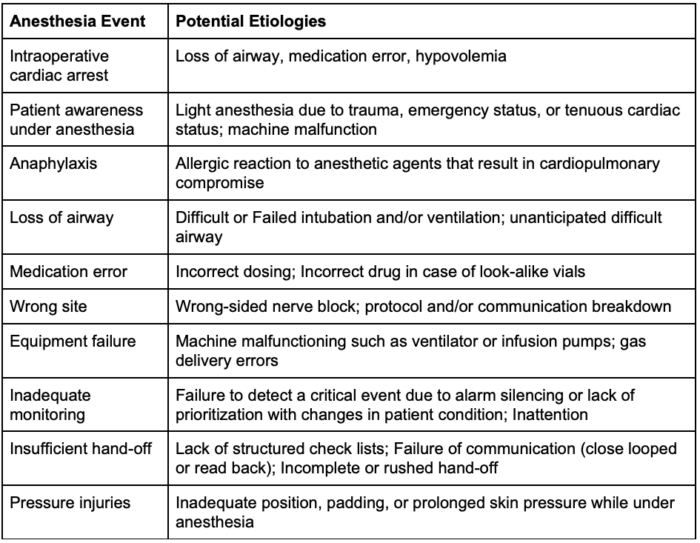
Table 4. Sentinel events and potential etiologies within anesthesia
Disclosure of Sentinel Events
- The JC maintains a sentinel events database. The aggregate information, including the causes and outcomes of sentinel events, is analyzed annually to gain insight into the causes of sentinel events and develop strategies to prevent harm to individuals under their care.1
- The JC received 1,411 reports of sentinel events in 2023. Link
- The majority of these events were self-reported (96%) by an accredited or certified entity.
- Most reported sentinel events occurred in the hospital setting (88%).
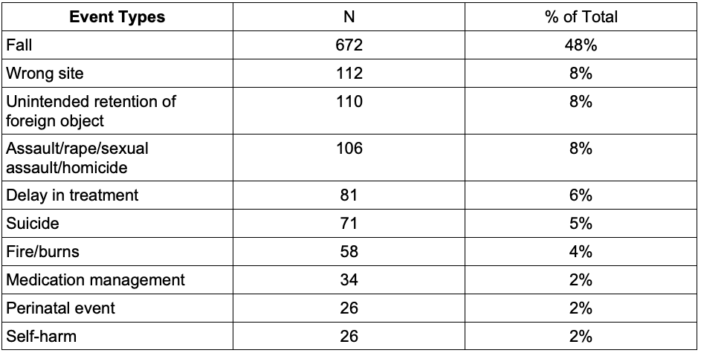
Table 5. Top ten reviewed sentinel event types. Adapted from the JC Sentinel Event Data 2023 Annual Review. Link
Sentinel Event Management and Root Cause Analysis
- When an event occurs, immediate stabilization and care of the patient are first priority.1,2
- There is institutional variability in the reporting of events. A root cause analysis (RCA) is typically employed to investigate sentinel events.1
- The JC specifically requires that the institution prepare and submit a credible RCA and action plan within 45 calendar days of the event.1,2
- This process examines human factors, system issues, communication breakdowns, and environmental conditions that contributed to or led to the event.1,8
- The RCA aim is to identify system issues that can be addressed sustainably, rather than focusing on individual factors.
- Please see the OA summary on RCA for more details. Link
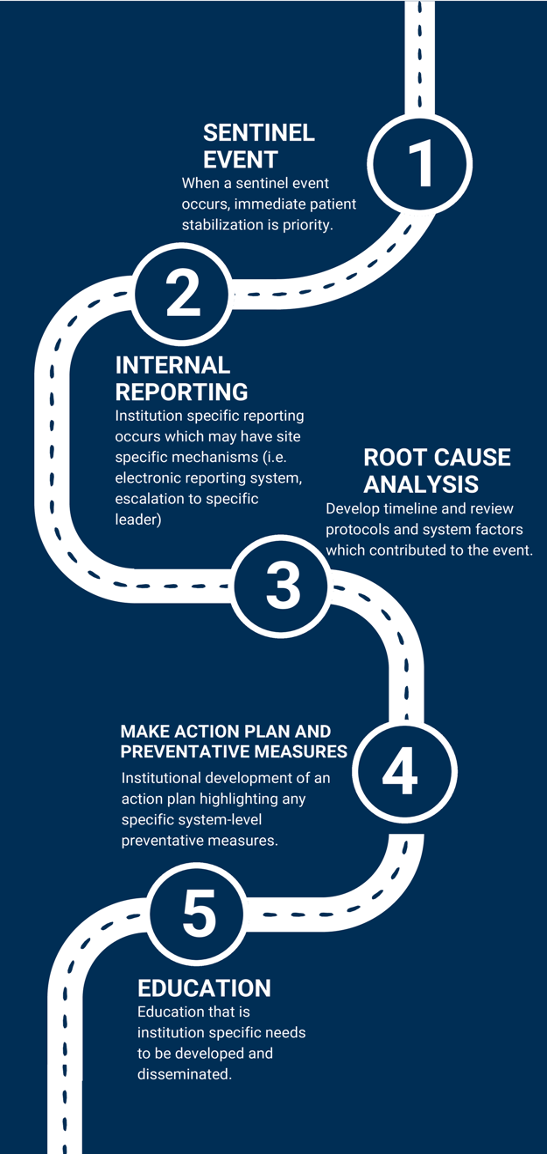
Figure 1. Timeline of reporting a sentinel event and development of an action plan
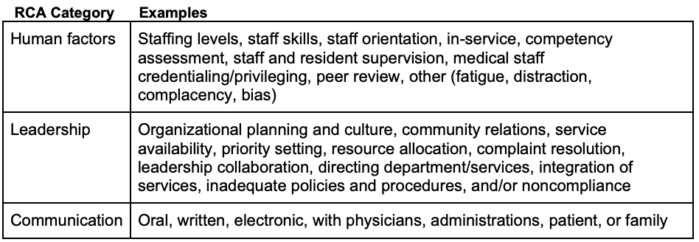
Table 6. Examples of root causes identified by the JC2
- Institutions should focus on building and fostering a safety-oriented culture that encourages the development of enhanced communication and a shared mental model.1,2
- Nonpunitive communities are recommended and ideal for patients where team members have psychological safety to report sentinel events.2
- Having team engagement will improve system-wide education and improvement, and ultimately lead to enhanced patient care and safety.1,2
Prevention Strategies
- Crisis resource management enhances preparedness and prevention of sentinel events. It is a skill derived from aviation that emphasizes skills while under stress.7
Crisis Resource Management Skills
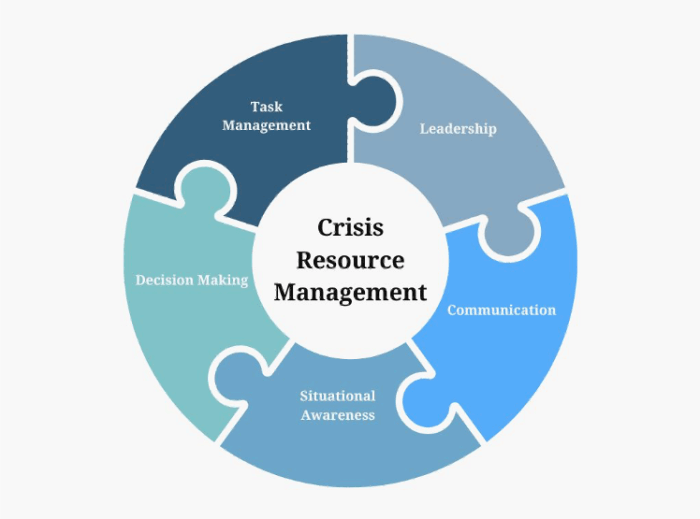
Figure 2. Different skills needed for crisis resource management
- These skills are relevant and critical in perioperative environments where events can unfold quickly and unpredictably.
- Simulation-based training is another tool for preventing and managing sentinel events. It enables the management of critical events in a controlled environment, reinforcing crisis resource management skills and facilitating debriefing.7
- Lastly, the development and implementation of perioperative risk reduction strategies, such as checklists, standardized protocols, equipment checks, and effective handoffs, play an essential role in preventing sentinel events.6,8
- These approaches are institution-dependent and must be tailored to individual sites to improve reliability and consistency.
References
- The Joint Commission. (2023). Sentinel Event Policy and Procedures. Link
- Tung A. Sentinel events and how to learn from them. Int Anesthesiol Clin. 2014;52(1):53-68. PubMed
- Cramer JD, Balakrishnan K, Roy S, et al. Intraoperative sentinel events in the era of surgical safety checklists: Results of a national survey. OTO Open. 2020;4(4):2473974X20975731. PubMed
- Cheney FW. The American Society of Anesthesiologists closed claims project: What have we learned, how has it affected practice, and how will it affect practice in the future? Anesthesiology. 1999;91(2):552-6. PubMed
- Staender S, Mahajan RP. Anesthesia-related complications: what can we learn from claims data? Curr Opin Anaesthesiol. 2011;24(3):325-32. PubMed
- Kent CD, Metzner JI, Domino KB. Anesthesia hazards: lessons from the anesthesia closed claims project. Int Anesthesiol Clin. 2020;58(1):7-12. PubMed
- Arriaga AF, Gawande AA. Improving patient safety through simulation training in anesthesiology. Anesthesiol Clin. 2012;30(1):1-19. PubMed
Other References
- Toimil B. Process improvement. OA summary. 2024. Link
- Amici LD, et al. Perioperative medication errors. OA summary. 2024. Link
- Li J, et al. Legal implications of medication errors. OA summary. 2024. Link
- Jian T, et al. Perioperative handovers. OA summary. 2024. Link
- Kanjia MK. Quality improvement methodology. OA summary. 2024. Link
- Kanjia MK. Barriers to quality improvement. OA summary. 2024. Link
- Kanjia MK. Lean Six Sigma. OA summary 2024. Link
- Kanjia MK. Safety II. OA summary. 2024. Link
- Kanjia MK. Root cause analysis. OA summary. 2024. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.