Copy link
Adult Liver Transplantation: Surgical Considerations
Last updated: 10/05/2023
Key Points
- Liver transplantation (LT) is the only proven treatment for end-stage liver disease (ESLD).
- Orthotopic liver transplantation (OLT) involves the removal of the diseased liver and its replacement, in the same anatomical space, with a donor organ.
- Two different surgical techniques are employed – the classic (cLT) and piggy-back techniques (pbLT) – which differ by their alternate approaches to the reanastomosis of the donor organ during the anhepatic stage.
Introduction
- The first OLT was undertaken in 1963 by Dr. Starzl at the University of Colorado.
- Mortality rates have steadily improved since then due to advances in patient selection, surgical technique, immunosuppressive therapy, anesthesia management, and intensive care provision.1
- Organs are obtained following donation after cardiac death, donation after brain death, or from the donation of a graft by a living donor.
- The most common indication for LT is cirrhosis or ESLD.
- Patient selection is a complex undertaking with input from many subspecialties.2
- Most patients undergoing LT have decompensated ESLD or are expected to deteriorate within a short period of time.
- The Model for End-Stage Liver Disease-Na (MELD-Na) Scoring system is currently used to quantify and compare patients’ disease burden and to facilitate a process for organ allocation to the sickest patients.
- Patients with acute liver failure are given the highest priority for a donated organ.
Donor Organ Selection and Allocation
- Organs are retrieved from donors in a variety of ways:
- Donation after brain death (DBD)
- Donation after cardiac death (DCD)
- Living donation
- In Western societies, the most common form of donation is DBD. The donor is brought to the operating room, where the organ can be retrieved with the heart still beating. However, in Eastern societies living donation, where a partial hepatectomy is performed to provide a donor graft, is the more popular technique. For DCD, the donor is taken to an operating room where life support is withdrawn, the heart allowed to cease beating, and death certified before organ retrieval. Organs retrieved from DCD donors usually have more ischemic damage compared to those from DBD donors.
- Please see the OA Summary on organ donation for more details. Link
- Donor organs are allocated to potential recipients based on need using the Model for End-Stage Liver Disease (MELD) scoring system.
- The MELD system was originally developed to predict the three-month mortality in patients with ESLD who underwent a transjugular intrahepatic portosystemic shunt procedure.
- In 2016, the MELD system was updated to the MELD-Na score to account for the hyponatremia that accompanies renal damage due to liver disease.
- The MELD-Na score is calculated using the most recent results for serum sodium, serum bilirubin, creatinine, and the International Normalized Ratio.
- A calculator can be accessed at Link
- There are two tiers for organ allocation:
- Tier 1 comprises patients without pre-existing liver disease needing rapid access to a donor graft for acute liver failure.
- Tier 2 covers those patients with ESLD whose condition is deteriorating over time, and their allocation of MELD points is based on recent laboratory test results.
Surgical Phases of Liver Transplantation
Traditionally, LT surgery can be divided into three stages: recipient hepatectomy (or dissection), graft implantation, and hemostasis and biliary reconstruction.1
Recipient Hepatectomy
- This stage starts at skin incision and continues until the explant of the native liver.
- In both cLT and pbLT, the surgeons must obtain control of the blood supply into and out of the liver.
- In the cLT approach, this is achieved by total vascular exclusion (TVE) of the liver, which drastically reduces any venous return to the heart via the inferior vena cava (IVC).
- The inflow to the liver is clamped/ligated: hepatic artery (HA) and portal vein (PV).
- The outflow is also clamped: suprahepatic and infrahepatic IVC.
- The liver is removed (with the intrahepatic IVC) as a block dissection (Figure 1).
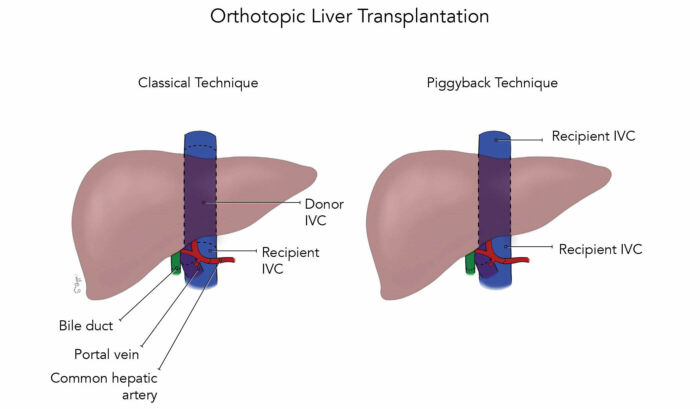
Figure 1. The classic and piggyback surgical techniques;
Abbreviation: IVC, inferior vena cava
- In the pbLT approach, the recipient intrathepatic IVC is preserved, and the hepatic veins are clamped at their attachment to the IVC to allow some venous return to the heart to be maintained, even if somewhat reduced (Figure 2).
- In both techniques, should the recipient be unable to tolerate the loss of preload, then venovenous bypass should be considered.3 Please see the OA summary “Venovenous Bypass During Liver Transplanation” for more details. Link
- The common bile duct is ligated and divided.
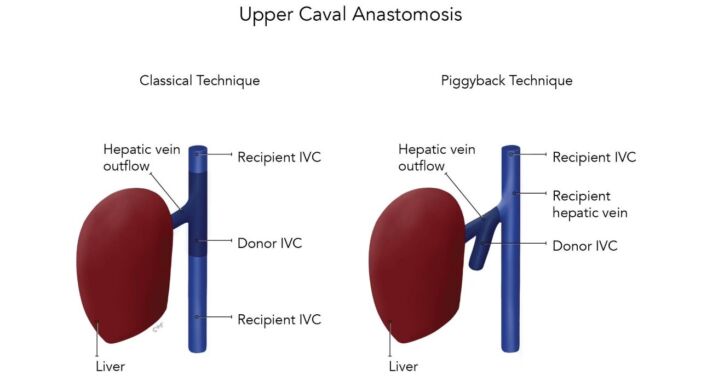
Figure 2. Classic and piggyback techniques showing different surgical approaches to the caval and hepatic vein anastomoses;
Abbreviation: IVC, inferior vena cava
Back-Table Preparation of the Donor Graft
- During the process of retrieval, the graft is usually flushed with a cold preservative solution, [e.g., University of Wisconsin Solution (UW) or histidine-tryptophan-ketoglutarate solution (HTK)] prior to being stored on ice and delivered to the recipient’s operating room.
- While the hepatectomy team is removing the native liver, a second team, usually in the same operating room, may be working to prepare the donor graft by (a) removing any excess tissue from around the organ, (b) preparing the vascular structures and biliary duct for future anastomoses and (c) remediating any injuries, lesions and anatomical abnormalities where possible (Figure 3).
- On the back table, the surgeons will secure a cannula into the donor’s portal vein through which the graft is flushed with a cold crystalloid or colloid solution to remove as much of the preservative solution as possible.
- After flushing, the graft is ready for implantation.
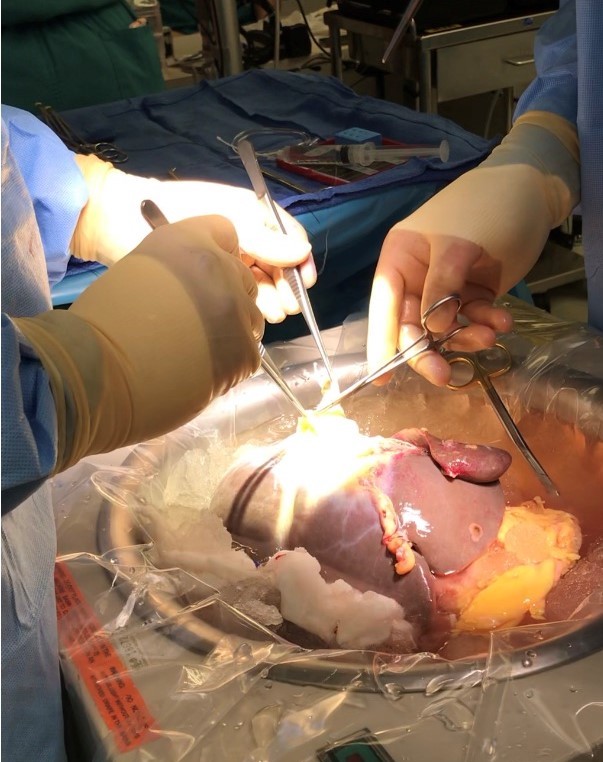
Figure 3. Back-table preparation of the donor organ; Image courtesy: Jennifer Cutler, MD
Graft Implantation
- In the cLT technique, the IVC anastomoses are performed first. Because of TVE, this part of the procedure is performed quickly because of hemodynamic instability, as venous return from the lower half of the body is totally occluded. Some centers prefer to use venovenous bypass to circumvent this issue.
- In the pbLT technique, the outflow from the donor organ is anastomosed to the recipient’s hepatic vein cuff or directly to the side of the suprahepatic IVC (Figure 2).
- The PV is then anastomosed in both the cLT and pbLT techniques, and the donor organ is reperfused. Venous return through the donor organ often leads to a period of profound hemodynamic instability due to the return to the circulation of cold, acidemic, cytokine-rich fluid from both the washout of the donor organ and return from the splanchnic bed. Some centers flush the donor organ prior to full reperfusion with warm saline and/or blood from the portal vein before allowing full venous return into the circulation.
- The hepatic artery is then reconstructed as an end-to-end anastomosis. This allows the return of oxygenated blood to the donor organ (Figure 4).

Figure 4. Full reperfusion of the donor organ; Image courtesy: Jennifer Cutler, MD
Hemostasis and Biliary Reconstruction
- With the donor organ fully reperfused, hemostasis is the next priority. Pre-existing coagulopathy, previous abdominal surgeries, etiology and severity of liver disease, surgical technique, and experience of the surgical team are all predictors of intraoperative blood loss and transfusion requirements.4
- The biliary system is reconstructed, either with an end-to-end anastomosis of the biliary duct or with a Roux-en-Y using small bowel.
- Bile production after HA reperfusion is a good surgical indicator of immediate graft function.
References
- Makowka L, Stieber AC, Sher L, et al. Surgical technique of orthotopic liver transplantation. Gastroenterol Clin North Am. 1988;17(1): 33–51. PubMed
- Dove LM, Brown RS. Liver transplantation in adults: Patient selection and pretransplantation evaluation. In: UpToDate, Robson KM (Ed), Waltham MA (accessed September 15, 2022). Link
- Lapisatepun, W, Lapisatepun W, Agopian V, et al. Venovenous bypass during liver transplantation: A New Look at an Old Technique. Transplantation Proceedings. 2020; 52: 905-9. PubMed
- Pandey CK, Singh A, Kajal K, et al. Intraoperative blood loss in orthotopic liver transplantation: The predictive factors. World J Gastrointest Surg. 2015;7(6):86-93. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.