Copy link
Postcesarean Delivery Analgesia
Last updated: 11/30/2023
Key Points
- Postcesarean delivery (CD) analgesia should ideally balance adequate pain relief with the risk of adverse side effects.
- Current recommendations include multimodal opioid-sparing analgesics, including neuraxial morphine with scheduled nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen, with the addition of supplemental opioids, only if needed.1
- Truncal nerve blocks are integral to enhanced recovery after cesarean (ERAC) protocols and should be implemented early in both CD performed under general anesthesia and rescue analgesia scenarios.
Introduction
- The overall rate of CDs, both primary and repeat, has substantially increased over the last 30 years. It is now becoming one of the most commonly performed surgeries in the world.2
- Patients have long reported pain, both during and after surgery, as their number one concern in the course of their personal health plan.3
- Greater pain duration and overall pain intensity increase the likelihood of future opioid use and postpartum depression and act as a barrier to maternal and fetal bonding.
- Multimodal pain management and perioperative planning are the backbones of modern ERAC protocols aimed at improving clinical outcomes.
Goals for Post-CD Analgesia
The goals for effective post-CD analgesia are interrelated and include the following.4
- Allow maternal-newborn bonding
- Allow safe breastfeeding, with minimal transfer of analgesics to the neonate
- Preserve the ability for the mother to care for her infant
- Minimize opioid use
- Facilitate postoperative mobilization to reduce the risk of thromboembolism
- Facilitate early discharge
Multimodal Analgesia Approach to Pain Management
- Post-CD analgesic plans should be personalized to the patient’s medical history and preferences while delineating the risks and benefits.
- Multimodal analgesia includes the administration of a long-acting neuraxial opioid while limiting systemic opioid consumption and is based on the additive or synergistic effects of different drugs or analgesic techniques in order to limit potential negative side effects. A multimodal approach to pain management post-CD has been shown to decrease opioid use and side effects by 30%.5
Patients Who Receive Neuraxial Opioids
- Neuraxial opioids provide analgesia for approximately 24 hours postoperatively when used as part of multimodal analgesia.
- Compared to systemic opioids, neuraxial opioids are associated with improved patient satisfaction, better pain scores, and increased time to first rescue analgesic.4
- Potential side effects include pruritus, nausea, vomiting, and respiratory depression. Notably, neuraxial opioids do not increase the risk of respiratory depression when compared to systemic opioids. See OA summary on neuraxial opioids. Link
- Commonly used neuraxial opioids for CD are listed in Table 1.
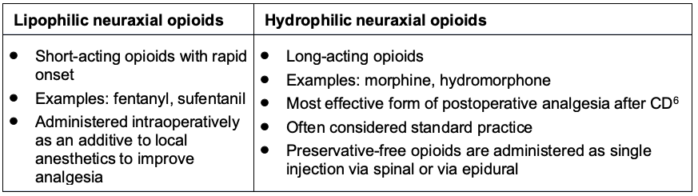
Table 1. Lipophilic and hydrophilic neuraxial opioids for CD
- The usual doses of neuraxial opioids are morphine 75 -150 mcg intrathecal (IT) or 1.5 – 3 mg epidural and hydromorphone 75 mcg IT or 0.4 – 1 mg epidural.
- Higher doses of neuraxial morphine can increase the duration of analgesia; however, there is a dose-response ceiling effect.6 Additionally, higher neuraxial morphine doses increase the risk of side effects. IT opioid administration results in lower systemic opioid levels than epidural injection.
- Single injections eliminate the need for catheter pumps or patient-controlled analgesia (PCA) and, therefore, allow earlier patient mobilization.4
Neuraxial Adjuvants
- Alpha-2 agonists like clonidine and dexmedetomidine have been shown to prolong or enhance postoperative analgesia, though the supporting data is limited.7
Acetaminophen
- Acetaminophen is highly effective in combination with NSAIDs and neuraxial opioids with limited side effects. Regularly scheduled per oral (PO) or intravenous (IV) administration is recommended for maximal efficacy.
- Plain acetaminophen should be used instead of a combination of acetaminophen-opioid. This results in a significant reduction in opioid consumption without affecting pain scores.1
- Dosing: During surgical closure, 1g IV acetaminophen can be given. Postoperatively, 650 mg PO can be given every 6 hours scheduled or 1000 mg every 8 hours for 48-72 hours with a maximum dose of 3g/day to avoid liver injury.
Nonsteroidal Anti-Inflammatory Drugs
- NSAIDs have been shown to reduce pain, opioid consumption, and sedation when administered as a part of a multimodal analgesia regimen.
- Regularly scheduled PO or IV administration (e.g., ibuprofen PO or ketorolac IV) is recommended. NSAIDs should be avoided in patients with thrombocytopenia, severe bleeding, or allergies.
- Side effects include increased blood pressure and bleeding secondary to platelet dysfunction. Careful consideration of NSAIDs is necessary before administering them to breastfeeding mothers of infants who are dependent on a patent ductus arteriosus. Selective COX-2 inhibitors may be associated with increased cardiovascular and thrombotic events.
- Most common NSAIDs given are IV ketorolac and PO ibuprofen. PO naproxen and PO diclofenac can also be administered.4
- Dosing: Ketorolac 15-30 mg IV q6-8h. Ibuprofen 600 mg PO q6h or 800 mg PO q8h scheduled for 48-72 hours. Naproxen 500 mg PO q12h scheduled. Celecoxib 200-400 mg PO q12h scheduled.
Alternate Regional Anesthesia Techniques
Patient-Controlled Epidural Analgesia (PCEA)
- Studies show that local anesthetics and opioids delivered via PCEA provide better pain relief compared to intravenous PCA.6
- Associated with decreased maternal mobility, increased nursing workload, increased cost, and interruptions in thromboprophylaxis.
- Dosing: bupivacaine 0.1% + fentanyl 2 mcg/mL. Continuous infusion at 10-15mL/hr, PCEA demand dose: 5 mL, lockout interval 15 minutes, one-hour maximum limit: 30-35 mL.
Peripheral Nerve Blocks (PNBs)
- Abdominal fascial plane PNBs may be used as rescue therapy for breakthrough pain. Patients should be monitored for local anesthetic systemic toxicity. PNBs have been shown to decrease systemic opioid requirements when neuraxial opioids are not administered.6
- Regional anesthesia techniques listed in Table 2 may be used for patients who did not receive long-acting neuraxial opioids and for patients with chronic pain or inadequate pain control.
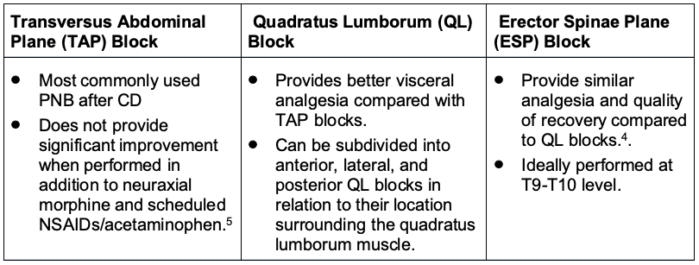
Table 2. Regional anesthesia blocks for CD
Systemic Opioids
- Intravenous PCA should ideally be discontinued after 24 hours and the patients should be transitioned to oral opioids. For PCA, IV hydromorphone or morphine is recommended.
- PO opioids have a similar efficacy to IV opioids.6 PO opioids have been shown to decrease nausea and drowsiness compared to IV opioids.4
- PO hydrocodone and oxycodone are preferred for breakthrough pain.
- Codeine and tramadol should be avoided due to potential increased CYP2D6 metabolism and resultant morphine in maternal breast milk.4
- Side effects of opioids include nausea, vomiting, sedation, fatigue, ileus, constipation, addiction risk, pruritus, and respiratory depression.
- Dosing: oxycodone 2.5-5mg PO q4h prn or hydromorphone 2mg-4mg PO q4h prn.
Adjuvant Analgesics
- Adjuvant analgesics that may be used for CD are listed in Table 3.
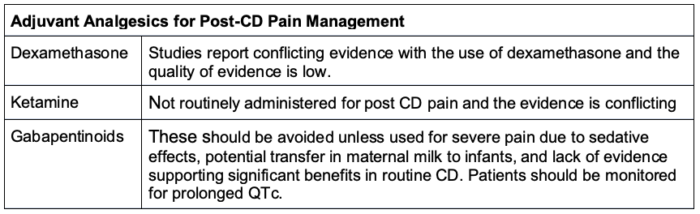
Table 3. Adjuvant analgesics that may be used for CD
General Anesthesia for CD
- Patients who received general anesthesia for CD, due to urgency or contraindications to neuraxial blocks, should receive multimodal analgesia.8
Breastfeeding Considerations
- The lowest effective dose of opioids should be given to avoid sedation and to facilitate successful breastfeeding.
- Drug concentrations in breast milk rise and fall in correlation with maternal plasma levels. NSAIDs and local anesthetics transfer less readily into breast milk compared to lipophilic drugs and other opioids since they are highly protein-bound.4
- High-risk transfer drugs such as tramadol, codeine, and meperidine should be avoided.
- See the OA summary on lactation and anesthesia. Link
SOAP Guidelines for Neuraxial Monitoring
- There is limited evidence to guide the optimal duration and frequency of respiratory monitoring necessary to detect and/or prevent adverse respiratory sequalae after CD in patients receiving neuraxial morphine.6
- Monitoring should be adjusted for high-risk patients with multiple comorbidities that predispose to respiratory depression (Figure 1).
- In the setting of low-dose neuraxial morphine in low-risk parturients, overly aggressive post-CD monitoring can negatively impact resource allocation and patient comfort without concurrently enhancing safety.6
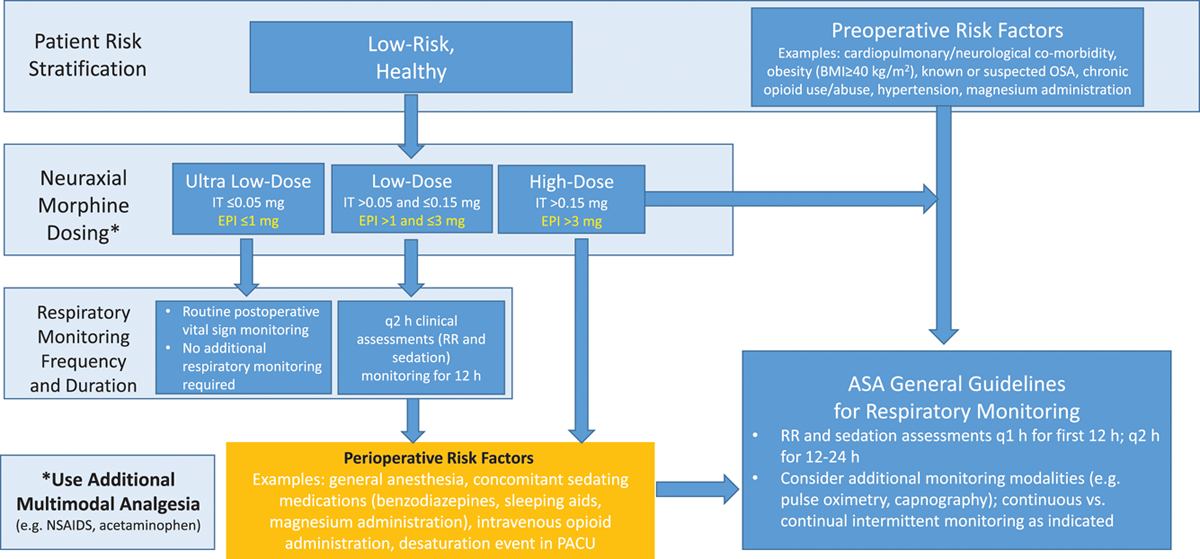
Figure 1. Respiratory monitoring algorithm following neuraxial morphine administration for post-CD analgesia.
Abbreviations: BMI = body mass index, EPI = epidural, Mg = magnesium, OSA = obstructive sleep apnea, PACU = postoperative anesthesia care unit, q = every, RR = respiratory rate.
Used with permission from Bauchat JR, et al. Society for Obstetric Anesthesia and Perinatology Consensus Statement. Monitoring recommendations for prevention and detection of respiratory depression associated with administration of neuraxial morphine for cesarean delivery analgesia. Anesth Analg. 2019;129(2):458-74.6
References
- Reed SE, Tan HS, Fuller ME, et al. Analgesia after cesarean delivery in the United States 2008–2018: A retrospective cohort study. Anesth Analg. 2021;133(1):1550-8. PubMed
- Stephenson J. Rate of first-time cesarean deliveries on the rise in the US. JAMA Health Forum. 2022;3(7):e222824. PubMed
- Carvalho B, Cohen SE, Lipman SS, et al. Patient preferences for anesthesia outcomes associated with cesarean delivery. Anesth Analg. 2005;101(4):1182-7. PubMed
- Carvalho B, Sutton C. Post-cesarean delivery analgesia. In: Post T (ed). UpToDate. 2023. Accessed September 21, 2023. Link
- Bollag L, Lim G, Sultan P, et al. Society for Obstetric Anesthesia and Perinatology: consensus statement and recommendations for enhanced recovery after cesarean. Anesth Analg. 2021;132(5):1362-77. PubMed
- Bauchat JR, Weiniger CF, Sultan P, et al. Society for Obstetric Anesthesia and Perinatology Consensus Statement. Monitoring recommendations for prevention and detection of respiratory depression associated with administration of neuraxial morphine for cesarean delivery analgesia. Anesth Analg. 2019;129(2):458-74. PubMed
- Edinoff AN, Houk GM, Kaye AD, et al. Adjuvant Drugs for Peripheral Nerve Blocks: The Role of Alpha-2 Agonists, Dexamethasone, Midazolam, and Non-steroidal Anti-inflammatory Drugs. Anesth Pain Med. 2021;11(3):e117197. PubMed
- Zanolli NC, Fuller ME, Krishnamoorthy V, et al. Opioid-sparing multimodal analgesia use after cesarean delivery under general anesthesia: A retrospective cohort study in 729 US hospitals. Anesth Analg. 2023;137(2):256-66. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.