Copy link
Lactation and Anesthesia
Last updated: 03/28/2023
Key Points
- Most anesthetic medications are short-acting and have no significant impact on a breastfeeding baby whose mother has received general anesthesia or sedation.
- Anesthesia is generally safe in lactating women, and continued breastfeeding throughout recovery should be encouraged.
- There is no need to "pump and dump" breastmilk after anesthesia.
- Long-acting oral opioids should be used judiciously in lactating women.
Introduction
- The American Society of Anesthesiologists (ASA) issued a statement in 2019, encouraging women to continue nursing their babies and/or pumping without discarding the breast milk postanesthesia.1
- Most anesthetic agents have low oral bioavailability and are short-acting, making the impact on a breastfeeding infant insignificant.1-3
- If the mother is awake and alert enough to hold her baby, then she may feed her baby. If there is a concern, the milk can be saved and given later.
- Exceptions are premature or critically ill infants at risk for apnea, hypotension, and hypotonia for whom medication exposure should be carefully considered.
Medications
- Various pharmacological factors determine the transmission of a drug into breast milk and its effect on the baby.2-4
- plasma protein binding;
- molecular weight;
- volume of distribution;
- pKA;
- lipid solubility; and
- maternal pharmacogenomics.
- Relative infant dose (RID) is a method to quantify safe dosing of a medication based on the properties previously mentioned.1 It is generally acceptable to use drugs with an RID <10%; however, each medication should be assessed individually (Table 1).
- Lactmed is a freely accessible peer-reviewed online database on the safety of drugs in lactating women Link.
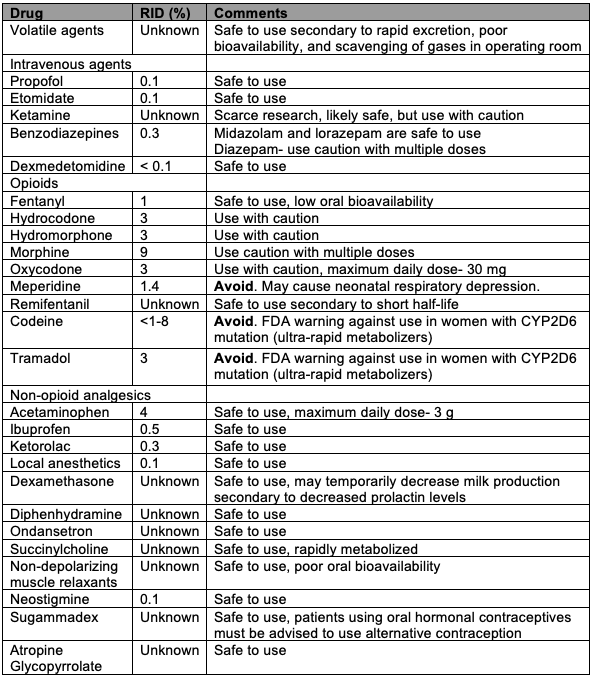
Table 1. Safety of commonly used anesthetic medications in lactating women. Adapted from references 1-3.
Perioperative Considerations2,3
Preoperatively
- It should be discussed with the mother if she wishes to continue breastfeeding and the anesthetic options that would be least disruptive to her breastfeeding schedule.
- Postponing elective procedures should be considered until the breastfeeding relationship is well established.
- A caretaker for the mother should be assigned to ensure safe timing of feeding the infant.
- Liberal fasting guidelines should be used and an early case start time should be scheduled, if possible.
- The mother should pump or breastfeed just prior to the procedure.
Intraoperatively
- Regional anesthesia and multimodal analgesia should be utilized to minimize the use of sedating and opioid medications.
- Aggressive postoperative nausea and vomiting prophylaxis should be used with nonsedating medications.
- Euvolemia without overhydration should be maintained.
Postoperatively
- It should be ensured that the mother has access to directly feed the infant once safe and ready. Access to and assistance with pumping should be ensured if separated from the infant.
- Opioids should be used judiciously, and another adult, besides the mother, must care for the infant if the mother requires opioids.
- If not considered safe to breastfeed because of an infant’s medical condition, milk should be pumped and saved for later use. It can be mixed or diluted with other milk that does not contain medications and used when the infant is older.
References
- ASA Committee on Obstetric Anesthesia. Statement on resuming breastfeeding after anesthesia. American Society of Anesthesiologists. Published 2019. Accessed November 28th, 2022. Link
- Reece-Stremtan S, Campos M, Kokajko L. ABM Clinical Protocol #15: Analgesia and anesthesia for the breastfeeding mother, revised 2017. Breastfeed Med. 2017;12(9):899-905. PubMed
- Mitchell J, Jones W, Winkley E, et al. Guideline on anaesthesia and sedation in breastfeeding women. Guideline from the Association of Anaesthetists. Anaesthesia. 2020;75(11): 1482-93. PubMed
- Hotham N, Hotham E. Drugs in breastfeeding. Aust Prescr. 2015;38(5):156-9. PubMed
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.