Copy link
Pneumothorax
Last updated: 06/25/2025
Key Points
- Pneumothorax is defined as gas in the pleural space outside of the lungs.
- Perioperative pneumothorax may present as hypoxemia, decreased tidal volumes, increased peak airway pressures, and acute cardiovascular collapse, typically not responsive to fluid or vasopressor administration.
- Tension pneumothorax is a clinical emergency and refers to continuous entrapment of air in the pleural space, causing compression of the lungs and/or impeding the filling of the heart.
- In skilled hands, ultrasound has proven to be more effective than chest X-ray (CXR) in diagnosing pneumothorax quickly.
- Needle decompression is an effective, potentially life-saving intervention in the setting of pneumothorax with hemodynamic instability.
Introduction
- Pneumothorax is defined as gas in the pleural space outside of the lungs.
- Air accumulates between the visceral and parietal pleura, exerting pressure on the lung and potentially leading to lung collapse.1
- Air may enter the chest either by external injury to the chest wall or internally by injury to the visceral pleura.1
- Management depends on the identification of the etiology, size, and degree of clinical instability.2
Types/Causes
The causes of pneumothorax can fall into the following categories:
Traumatic Pneumothorax
- Causes include penetrating trauma, blunt trauma, rib fractures, diving, or flying.1
- Simple: Does not shift mediastinal structures1
- Open: Open injury to the chest wall that allows air to move in and out.1
Iatrogenic
- Accidental injury to the chest wall/visceral pleura caused during a medical procedure.
- Examples: Central line placement, intercostal/brachial plexus nerve block, pleural/lung/pulmonary nodule biopsy, tracheostomy, positive pressure ventilation, etc.
Capnothorax
- A specific type of pneumothorax that consists of carbon dioxide in the thoracic cavity outside of the lungs.
- This type is seen in the setting of insufflation during laparoscopic procedures.
Atraumatic Pneumothorax
- Primary spontaneous pneumothorax:
- It occurs without a clear inciting event and in the absence of preexisting lung disease.2
- It is three to six times more common in males than in females.2
- Risk factors include tall and thin stature, Marfan syndrome, smoking, pregnancy, and a familial history.1
- Secondary spontaneous pneumothorax:
- It presents as a complication of underlying lung disease.3
- It occurs more commonly in older patients (older than 55 years).
- Risk factors include acute respiratory distress syndrome, asthma, sarcoidosis, chronic obstructive pulmonary disease, cystic fibrosis, tuberculosis, and other lung pathologies.1
- Pulmonary cysts or bullae are air cavities within the thorax outside of the lung that may be congenital or acquired as a result of emphysema. These air cavities can act as one-way valves, allowing air to enter but not escape. This can lead to progressive enlargement and rupture during positive-pressure ventilation, resulting in a tension pneumothorax (see below).4
Tension
- Tension is a specific subtype of pneumothorax in which air can enter the pleural space without the ability to escape.
- This can quickly lead to a rapid increase in size, midline tracheal shift, and hemodynamic instability due to rising intrathoracic pressure, which limits venous return to the heart (preload).
- Causes include penetrating/blunt trauma, positive pressure ventilation, and conversion from a spontaneous pneumothorax.1
Clinical Presentation
- Perioperative pneumothorax may present as hypoxemia, decreased tidal volumes, increased peak airway pressures, and acute cardiovascular collapse, typically not responsive to fluid or vasopressor administration.5
- Potential signs:
- Hypotension
- Tachycardia
- Narrowed pulse pressure
- Tachypnea
- Decreased or absent breath sounds
- Tracheal shift
- Jugular venous distension
- Hypocapnia (due to V/Q mismatch) or hypercapnia (capnothorax)
- Chest pain (possibly radiating to ipsilateral shoulder)1
- Dyspnea
Diagnosis
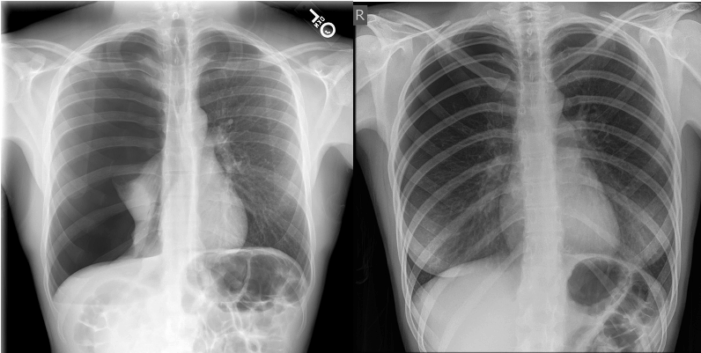
- CXR, computed tomography, or ultrasonography are the most common methods used to diagnose pneumothorax.1
- On CXR, a pneumothorax is considered small if the distance from the pleural line to the apex is less than 2 cm, while a large pneumothorax is when the distance from the pleural line to the apex is larger than 2 cm.2,3
- Intraoperative findings suggestive of pneumothorax include the constellation of the following: unilateral absent or diminished lung sounds, hypoxemia, increased peak airway pressures, and characteristic findings on lung point-of-care ultrasound (POCUS) (see below).
- Intraoperative differential diagnosis must exclude endobronchial intubation, endotracheal tube obstruction, and auto-positive end-expiratory pressure (PEEP) (exclude by briefly disconnecting the breathing circuit).6
Lung POCUS
- In skilled hands, ultrasonography has proven to be more effective than CXR (with a sensitivity of 94% and a specificity of 100%) in diagnosing pneumothorax quickly.1
- The easiest lung POCUS window to use intraoperatively is placing the US probe at the midclavicular line of the 2nd intercostal space to evaluate for lung sliding (Figure 2 below).7
- Lateral and posterior lung windows may also be obtained.
- On lung POCUS findings, pneumothorax is characterized, at minimum, by focal absence of lung sliding.7
- However, focal absence of lung sliding is also seen in the following conditions.8
- Mainstem intubation
- Lung adhesions
- Emphysematous blebs
- For more details on how to diagnose a pneumothorax using ultrasonography, please see the OA summary Lung Point-of-Care Ultrasound (Link)
Management
Management depends on the etiology, size, degree of clinical instability, and likelihood of recurrence.2,3
Needle Decompression
- If clinically unstable, the insertion of a 14 or 16 gauge and 4.5 cm angiocath just superior to the rib in the 2nd intercostal space, along the midclavicular line, allows for the rapid release of air from the pleural space, resulting in improvement in hemodynamic stability.1
- Needle compression can also occur in the 4th or 5th intercostal space between the anterior and midaxillary line.6
- There has been debate regarding which site for needle decompression has a higher success rate. The 2018 Advanced Trauma Life Support guidelines recommend the 4th or 5th intercostal space between the anterior and midaxillary line for adult patients due to research suggesting it is associated with higher failure and complication rates, including potential injury to underlying structures.8 However, Azizi et al. reported an increased chest wall thickness in the 4th or 5th intercostal space between the anterior and midaxillary line compared to the 2nd intercostal space at the midclavicular line in the obese and overweight population. This may be predictive of a higher rate of success of needle decompression at the 2nd intercostal space at the midclavicular line in obese or overweight patients.10
- The 2nd intercostal space at the midclavicular line remains the suggested site for pediatric needle decompression.9
- The needle should be left in place while awaiting chest tube placement.6
Further Management
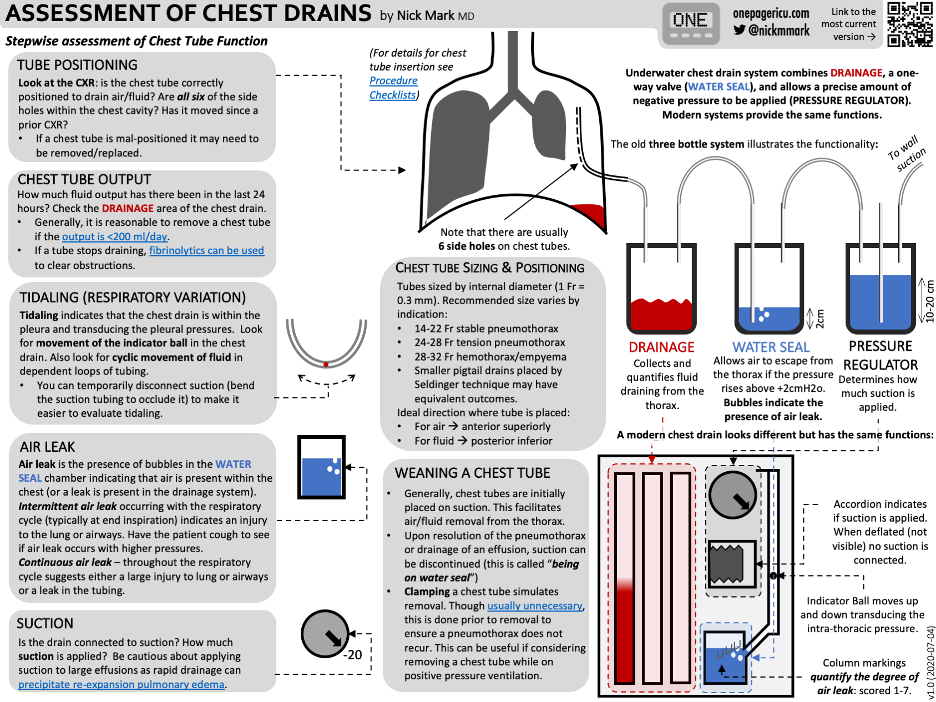
- Needle decompression is usually followed by chest tube placement in the 5th intercostal space just superior to the rib, slightly anterior to the midaxillary line.1
- A small-bore catheter (14 French or smaller) or tube (22 French or smaller) is generally preferred over large-bore tubes.2
- Generally, suction is not initially applied, and subsequently, the tube or catheter is connected to a water seal device.2
- Please see the ICU One-Pager on how to assess and manage chest drains below (Figure 3).
- The underlying disorder should be treated.
- If clinically stable, small pneumothoraces may be treated with observation. A stable patient is defined as one who can speak in full sentences and has a respiratory rate of less than 24 breaths per minute, a heart rate between 60 and 120 beats per minute, normal blood pressure, and room air oxygen saturation greater than 90%.2
- Larger pneumothoraces may warrant chest tube placement, even in the presence of hemodynamic stability.1
- Supplemental oxygen may aid in the resorption of air without intervention.1
- Nitrous oxide should be discontinued as it can rapidly expand in air-filled cavities, increasing the size of the pneumothorax.
- If capnothorax is present, PEEP may be applied. If the patient is hypoxemic, the pneumoperitoneum should be released.
- If an open “sucking” chest wound is present secondary to chest wall trauma, a three-way occlusive dressing may be placed while awaiting chest wall reconstruction.1
- Video-assisted thoracoscopic surgery may be performed in patients with persistent air leak or recurrent pneumothorax.1
References
- McKnight CL, Burns B. Pneumothorax. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. Link
- Lee YCG, Broaddus VC, Finlay G. Pneumothorax in adults: Epidemiology and etiology. In: Post T, ed. UpToDate; 2025. Accessed May 28th, 2025. Link
- Lee YCG, Broaddus VC, Finlay G. Treatment of secondary spontaneous pneumothorax in adults. In: Post T, ed. UpToDate; 2025. Accessed May 28th, 2025. Link
- Butterworth IV JF, Mackey DC, Wasnick JD, eds. Anesthesia for Thoracic Surgery. In: Butterworth IV JF, Mackey DC, Wasnick JD, eds. Morgan & Mikhail's Clinical Anesthesiology. 7th ed. New York, NY: McGraw-Hill Education; 2022:555-584.
- Butterworth IV JF, Mackey DC, Wasnick JD, eds. Anesthesia for Patients with Respiratory Distress. In: Butterworth IV JF, Mackey DC, Wasnick JD, eds. Morgan & Mikhail's Clinical Anesthesiology. 7th ed. New York, NY: McGraw-Hill Education; 2022:537-554.
- Goldhaber-Fiebert SN, Austin N, Sultan E, et al. Stanford Anesthesia Cognitive Aid Program, Emergency Manual: Cognitive aids for perioperative crises. Version 4, 2021. Accessed June 5, 2025. Link
- Husain LF, Hagopian L, Wayman D, Baker WE, Carmody KA. Sonography diagnosis of pneumothorax. In: J Emerg Trauma Shock; 2012; 5(1): 76-81. PubMed
- Bronshteyn YS, Krishnan S, Abramson L, et al. Scan that barcode carefully, limitations of “M-mode” ultrasound when screening for ultrasound. AA Pract. 2024;18(12): e01854. PubMed
- American College of Surgeons. Advanced Trauma Life Support (ATLS®) Student Course Manual. 10th ed. Chicago, IL: American College of Surgeons; 2018. Link
- Azizi N, Ter Avest E, Hoek AE, et al. Optimal anatomical location for needle chest decompression for tension pneumothorax: A multicenter prospective cohort study. Injury 2020. 52(2):213-8. Link
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.