Copy link
Intraoperative Hypothermia
Last updated: 09/13/2023
Key Points
- Unwarmed anesthetized patients become hypothermic, typically by 1-2°C, from a combination of anesthesia-induced thermoregulatory impairment, cool operating room (OR) ambient temperature, and evaporative losses from surgical incisions.
- Both general and neuraxial anesthesia significantly impair thermoregulation and synchronously reduce the thresholds for vasoconstriction and shivering.
- Intraoperative hypothermia typically has a characteristic three-phase pattern and results initially from an internal redistribution of heat from the core to the periphery, followed by heat loss exceeding metabolic heat production and a plateau phase when thermoregulatory thresholds are activated, or heat loss matches heat production.
- The core temperature of surgical patients should be maintained above 35.5°C since lower temperatures are associated with several complications, including coagulopathy, surgical-site infection, delayed drug metabolism, prolonged recovery, and shivering.
Normal Thermoregulation
- Normally, the core body temperature is tightly maintained within a narrow range of temperatures from 36.6°C to 37.4°C.1-3
- The hypothalamus is the primary center for thermoregulation, and it receives input from multiple temperature sensors in the skin and other parts of the body.
- In addition to behavioral adaptation, the major thermoregulatory autonomic responses in humans are arteriovenous shunt vasoconstriction, shivering, and sweating.
- Please see the Normal Thermoregulation summary for more details.
Effects of Anesthetics on Thermoregulation
- Both general and neuraxial anesthesia significantly impair thermoregulation and synchronously reduce the thresholds for vasoconstriction and shivering. As a result, unwarmed anesthetized patients typically become hypothermic by 1-2°C.1-3
Effects of General Anesthesia (GA)
- All volatile anesthetic agents, nitrous oxide, and most intravenous anesthetic agents (propofol, dexmedetomidine, and opioids) impair thermoregulation in a dose-dependent fashion. Midazolam does not appreciably impair thermoregulatory control.1-3
- GA decreases the vasoconstriction threshold to approximately 34.5°C, and the shivering threshold is decreased 1°C even lower than the vasoconstriction threshold (Figure 1). Interestingly, the normal 1°C difference between the vasoconstriction and shivering thresholds is maintained.2
- Sweating and other warm defenses usually remain intact during general anesthesia. As a result, the interthreshold range increases significantly, often a 10-fold increase1-3 (Figure 1).
- In addition to the preserved or slightly increased sweating threshold, the gain and maximum intensity of sweating are well preserved.1-3
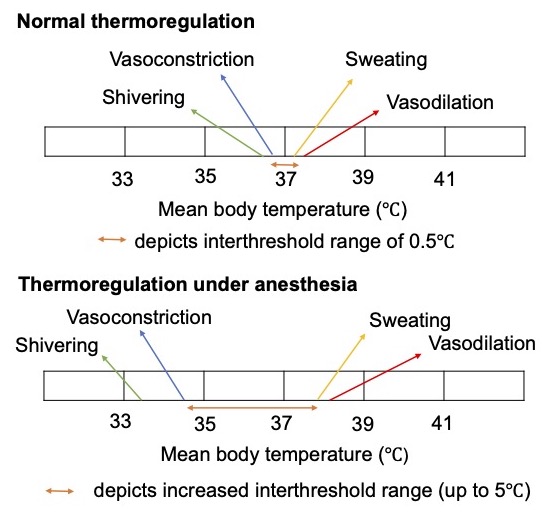
Figure 1. Effects of anesthesia on thermoregulation. Adapted from Doherty M, Bugg D. Thermoregulation. In: Hemmings & Hopkins, ed. Foundations of Anesthesia. 2nd edition, PA. Elsevier; 2006: 8090-26.
Effects of Regional Anesthesia
- Neuraxial anesthesia also impairs thermoregulatory control by reducing the vasoconstriction and shivering thresholds, albeit to a lesser degree than GA. The changes in the shivering threshold are proportional to block height. Neuraxial anesthesia blocks the afferent and efferent thermoregulatory signals.1-3
- In addition to reducing the vasoconstriction and shivering thresholds, the gain and maximum intensity of shivering is approximately half normal.1-3
- Patients with epidural or spinal anesthesia typically do not complain of feeling cold, even if they are hypothermic. This is due to thermal perception being primarily determined by skin temperature rather than core temperature, and skin temperature increases with neuraxial anesthesia. Thus, behavioral thermoregulation is impaired.1
- Unlike neural anesthesia, peripheral nerve blocks do not have significant thermoregulatory effects.
- Patients under combined general and neuraxial anesthesia are at the highest risk for hypothermia secondary to additive thermoregulatory impairment from each technique.1-3
Phases of Hypothermia
- Intraoperative hypothermia occurs in a characteristic three-phase pattern (Figure 2).
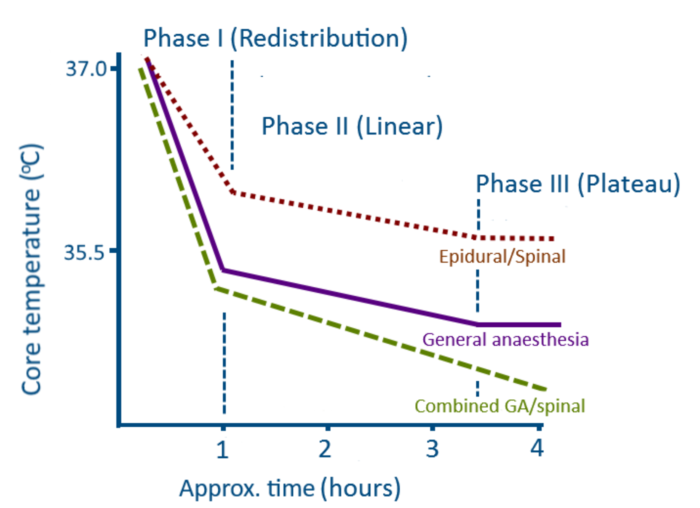
Figure 2. Three-phase pattern of intraoperative hypothermia. Source: Perioperative hypothermia. Perioperative CPD, WFSA. CC BY NC SA 4.0.
- During the initial hour after induction of GA or activation of the neuraxial block, the patient’s core temperature decreases rapidly by 1-1.5°C due to redistribution from the core to peripheral tissues from anesthesia-induced vasodilation.1-3
- This redistribution hypothermia is followed by a slower, linear reduction in core temperature when heat loss exceeds heat production. The main mechanism of heat loss is radiation, followed by convection. Usually, only small amounts are lost via conduction or evaporation. See the Normal Thermoregulation summary for mechanisms of heat loss.
- The third phase, or plateau phase, occurs when the patient becomes sufficiently hypothermic to activate thermoregulatory vasoconstriction (usually 34.5°C), which effectively retains heat in the core tissues, preventing further decreases. A plateau in core temperature can also occur when heat loss and heat production are matched.1-3
- The pattern of hypothermia during neuraxial anesthesia is similar to GA for the first two phases. As neuraxial anesthesia blocks vasoconstriction, the plateau phase may not occur.4
Consequences of Hypothermia
Coagulopathy
- Hypothermia causes coagulopathy primarily by impairing platelet aggregation via reduced release of thromboxane A3, thereby affecting platelet plug formation. It also reduces the activity of enzymes in the coagulation cascade. A combination of these factors increases perioperative blood loss and the need for transfusion.1,3,4
Surgical Site Infections
- Perioperative hypothermia increases the risk of surgical site infections. The primary mechanisms are reduced tissue perfusion, decreased motility of macrophages and other key immune cells, and reduced scar formation.1,3,4
Prolongation of Drug Effects
- Even mild hypothermia prolongs the action of neuromuscular blocking agents.1,3,4
- By decreasing hepatic flow, hypothermia increases plasma propofol concentrations.
- Hypothermia also decreases the minimum alveolar concentration (MAC) of volatile anesthetics. MAC decreases by 5% for every one-degree decrease in core temperature.1,3
Shivering/Myocardial Ischemia
- Postoperative shivering is common in hypothermic patients. Shivering increases metabolic activity and causes sympathetic stimulation, increasing myocardial oxygen consumption and the risk of myocardial ischemia and arrhythmias, especially in patients with coronary artery disease.
- Postoperative shivering may be treated with meperidine (12.5-25 mg IV in adults) or alpha-2 agonists, like clonidine or dexmedetomidine.1,3
Prevention and Management of Hypothermia
Several strategies can be used to prevent and treat intraoperative hypothermia.
Prewarming Before Induction of Anesthesia
- Actively warming patients in the preoperative area using radiant heat or a forced-air convective warmer increases the temperature of peripheral tissues and minimizes the redistribution hypothermia after induction of GA. The core temperature in prewarmed patients stays about 0.4°C warmer than in non-prewarmed patients.1,3
Passive Insulation
- Insulating the patient with a single layer of an insulator (linen blanket) reduces heat loss by approximately 30% as it traps the air between the skin and the blanket. Unfortunately, additional blankets provide only a slight additional benefit.1,3,4
Active Warming Devices
- Actively warming the skin surface using forced air, resistive heating, or circulating water blankets are the typical strategies.1,3
- Forced air warming blankets are the most commonly used as they are effective, inexpensive, and easy to use. Even though theoretical concerns have been raised regarding the potential for forced-air warming devices to disturb laminar flow and increase infection risk, there is no clinical evidence that there is an increased infection risk.1
Fluid Warming
- Fluid warming does not significantly warm patients since IV fluids can only slightly exceed core temperature. Fluid warming does not compensate for redistributive hypothermia or other heat losses.
- However, infusion of large amounts of unwarmed fluids can cause hypothermia. Each liter of IV fluid administered at ambient temperatures reduces the mean body temperature in an adult by 0.25°C. Similarly, a unit of refrigerated blood reduces the mean body temperature by 0.25°C.1,3
Airway Heating
- The heat capacity of air is low. Therefore, airway heating and humidification does not significantly warm the patient.1,3
References
- Sessler D. Perioperative temperature management. In: Post T, ed. UpToDate; 2023. Accessed July 30th, 2023. Link
- Sessler DI. Temperature monitoring and perioperative thermoregulation. Anesthesiology. 2008; 109(2): 318-38. PubMed
- Sessler DI. Perioperative thermoregulation and heat balance. Lancet. 2016; 387:2655. PubMed
- Rao S, Rajan M. Heat production and loss. Update in Anaesthesia. 2008; 24(2): 182-7. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.