Copy link
Normal Thermoregulation
Last updated: 09/13/2023
Key Points
- Core body temperature is tightly maintained within a narrow range of temperatures from 36.6°C to 37.4°C.
- The hypothalamus is the primary center for thermoregulation, and it receives input from multiple temperature sensors in the skin and other parts of the body.
- While behavioral modification is a very strong thermoregulatory response in awake humans, surgical patients depend on autonomic responses such as vasoconstriction, shivering, and sweating.
- Radiation is the major mechanism of heat loss from the body.
Normal Thermoregulation
- Normally, the core body temperature is tightly maintained within a few tenths of a degree Celsius.1,2
- To understand physiological thermoregulation, it is useful to divide the body into a central core and a peripheral compartment.2
- The core (brain, thoracic, and abdominal organs) holds about 2/3rd of the body heat content and is usually maintained within a narrow range of temperatures from 36.6°C to 37.4°C.2
- The periphery (limbs, skin, and subcutaneous tissue) acts as a buffer and contains about 1/3rd of the total body heat. The temperature of the periphery varies widely depending on the environment and is usually 30-32°C. This 5-7°C difference is primarily mediated via vasoconstriction of blood vessels to the periphery.2
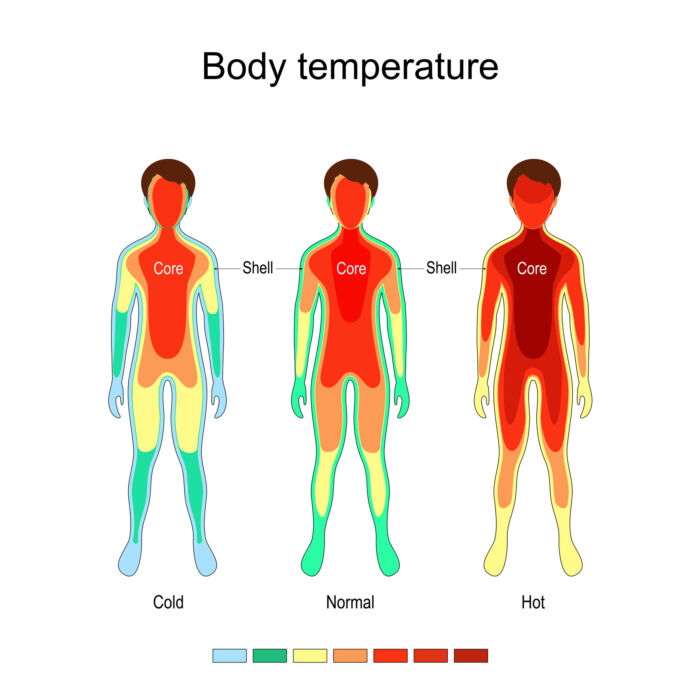
Figure 1. Central core and peripheral compartment for thermoregulation. Source: ttsz, iStockphoto.com.
Physiological Control
- The processing of thermoregulation occurs in three phases: afferent thermal sensing, central regulation, and efferent responses.3
- The hypothalamus is the primary center for thermoregulation. It receives input from temperature sensors throughout the body. The skin provides about 20% of the thermal input, while thermally sensitive cells throughout the body (hypothalamus, other parts of the brain, deep abdominal, and thoracic tissues) each contribute roughly 20% of the input.2,3
- Human skin is very sensitive to temperature changes. However, skin temperatures and the ability to influence thermoregulatory responses is not uniform. For example, the face is approximately five times as sensitive as other areas.3
- Cold receptors respond to temperatures from 10 to 36°C and send their impulses via A-delta fibers.2,3 Warm receptors respond to temperatures from 30 to 45°C and send their impulses via unmyelinated C fibers.2,3 This is the reason why patients often cannot distinguish between sharp pain and intense heat.
- Inputs from various sites are integrated in the hypothalamus, and appropriate responses are initiated.
- Behavioral modification is a very powerful thermoregulatory response. These include moving from direct sun to shade, dressing up in layers, or altering the ambient temperature using heating or air-conditioning.3
- Surgical patients largely depend on autonomic responses such as shivering, vasoconstriction, and sweating.
- The body’s responses to cold include shivering and arteriovenous vasoconstriction.1
- Vasoconstriction is the most important autonomic thermoregulatory response.3 Vasoconstriction of arteriovenous shunts in acral regions (fingers, toes, nose, etc.) occurs via norepinephrine released from sympathetic nerves.
- Shivering augments metabolic heat production by 50-100% in adults but is largely ineffective.3
- In elderly patients, these cold-defense thresholds are reduced by approximately 1°C.1 In infants, nonshivering thermogenesis is another potent defense mechanism and source of heat production. See the Temperature Regulation in Pediatric Anesthesia summary.
- The body’s responses to heat are precapillary vasodilation and sweating.
- Sweating is a remarkably effective way to dissipate heat.3 Adults can sweat up to 1 liter per hour, and trained athletes can sweat twice as much. Each gram of sweat dissipates 0.58 kcal.3
- Sweating is prevented by nerve blocks and atropine administration.3
Threshold Temperatures
- The temperature at which a response is triggered is called the threshold temperature (Figure 2). The threshold temperature varies with gender, exercise, nutrition, drugs, and during infection.2,3 Note that the shivering threshold is 1°C below the vasoconstriction threshold. By the time humans shiver, they are fairly hypothermic.1
- Both the sweating and vasoconstriction thresholds are 0.3-0.5°C are higher in women than men.3
- The temperature range between the sweating and vasoconstriction thresholds is called the interthreshold range, when no thermoregulatory defenses are activated. The interthreshold range is usually 0.2-0.4°C in humans, and that range defines the normal body temperature.3
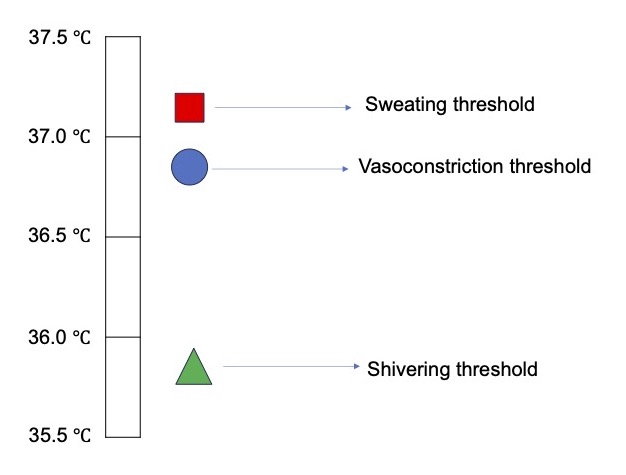
Figure 2. Thresholds for thermoregulatory defenses. Adapted from Sessler D. Perioperative temperature management. In: Post T, ed. UpToDate; 2023.
Heat Production
- Heat is produced via normal metabolic activity. At rest, the basal metabolic rate is about 1700 kcal/day in a 70 kg adult man. About 2/3rd of this energy is dispersed as heat, and the rest is stored as chemical energy in the form of adenosine triphosphate.2
- Heat production can be increased by voluntary muscle activity (exercise), involuntary muscle activity (shivering), and nonshivering thermogenesis, an important method of heat production from brown adipose tissue in neonates.2
Heat Loss
The major mechanisms of heat loss are radiation, convection, conduction, evaporation, and respiration (Figure 3).
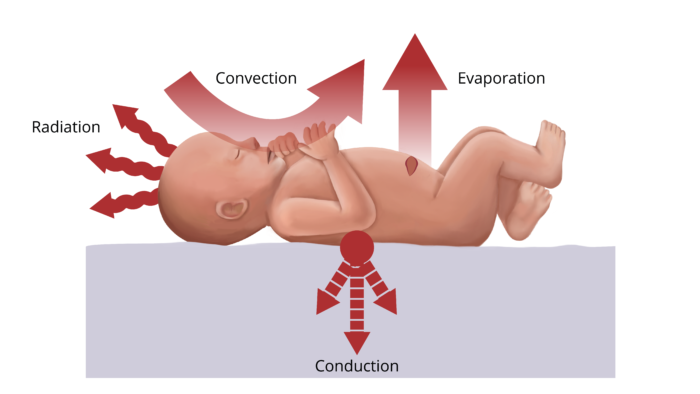
Figure 3. Methods of heat loss in the operating room.
Radiation
- Radiation is the major method of heat loss and accounts for about 60% of the total heat loss. It involves the transfer of heat in the form of infrared waves to cooler objects in the surrounding area, not in direct contact with the body.
- The amount of heat loss via radiation is proportional to the fourth power of the temperature difference between the objects. If the operating room temperature is decreased by 2°C, heat loss will increase by a factor of 16 (24).2
Convection
- Convection occurs when the layer of air next to the patient’s skin moves and carries heat away from the body. This is the reason windy days are cooler than calm days at the same temperature.2
- Convection accounts for about 25% of heat loss but varies on the surface area of the body that is exposed and the amount of airflow.2
Conduction
- Conduction involves heat transfer through a solid medium (transfer of energy of motion of the molecules to adjacent molecules). For example, contact of the patient’s body with an object of lower temperature.
- Conduction only accounts for 1-2% of heat loss.2
Evaporation
- Heat is consumed during the vaporization of water. Heat loss by evaporation occurs via sweat, abdominal cavities, wound surfaces, evaporation of skin-preparation solutions.2
Respiration
- Normal respiration accounts for a small amount of heat loss, typically 10%. Heat loss through this route can be reduced by humidifying inspired gases and using low fresh gas flows.2
References
- Sessler D. Perioperative temperature management. In: Post T, ed. UpToDate; 2023. Accessed July 30th, 2023. Link
- Rao S, Rajan M. Heat production and loss. Update in Anaesthesia. 2008; 24(2): 182-7. Link
- Sessler DI. Temperature monitoring and perioperative thermoregulation. Anesthesiology. 2008; 109(2): 318-38. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.