Copy link
Cerebral Palsy
Last updated: 05/15/2024
Key Points
- Patients with cerebral palsy (CP) often have developmental delays along with other comorbidities, including gastroesophageal reflux disease (GERD), chronic aspiration, immobility/contractures, pulmonary conditions, and epilepsy.
- Anesthetic issues commonly seen in patients with CP can include temperature control, challenges with positioning due to contractures, analgesic considerations, respiratory considerations, bleeding, varied developmental ability, and medication dosing variability.
- Additional postoperative challenges may include evaluation and effective pain management, spasticity, temperature control, and return to respiratory and neurological baseline.
What is Cerebral Palsy?
CP is a heterogeneous group of disorders with permanent motor dysfunction that affects muscle tone, posture, and/or movement. The incidence of CP is as high as 3.4 per 1,000 live births in pre-perinatal diagnoses for low- and middle-income countries. A recent meta-analysis showed that high-income countries had a lower prevalence at 1.5 per 1,000 births.1
- There is a spectrum of the diagnosis of CP, with 80% of cases being acquired prenatally without any obvious insult. There is a strong association with prematurity (40%) and low birth weight, as well as intrauterine growth restriction, intracranial hemorrhage, and trauma. In premature infants, periventricular leukomalacia is commonly seen, while in term infants, insults immediately after birth seem to be a common etiology of CP.4 However, no genetic link has been identified at this time.3 Approximately 11% of babies delivered between 24-27 weeks gestational age are diagnosed with CP.4
- Given their comorbidities, patients with CP are frequently scheduled for various surgical and medical procedures requiring general anesthesia. For this reason, a thorough understanding of a patient’s condition is imperative to formulate appropriate preoperative, intraoperative, and postoperative plans.
Classification of Cerebral Palsy
CP can be classified by physiology, topography/physical features, etiology, and functional capacity.
- Physiological classification includes spastic, athetoid, rigid, ataxic, tremor, atonic, mixed, or unclassified CP.
- Topography can include monoplegia, paraplegia, hemiplegia, triplegia, quadriplegia, diplegia, or double hemiplegia.
- The etiology of CP can be prenatal, perinatal, or postnatal.
- Prenatal/intrauterine causes include infection, metabolic, anoxic, genetic, or other conditions.
- Perinatal causes are related to the time of delivery and possibly due to anoxic causes.
- Postnatal causes occur after birth and may be secondary to toxins, trauma, infection, or other causes.
- Functional capacity is classified by the limitation of activity that is present.2
- Class 1: no limitation of activity
- Class 2: slight to moderate limitation
- Class 3: moderate to great limitation
- Class 4: no useful physical activity
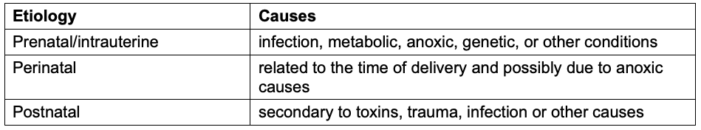
Table. 1 Etiology of CP
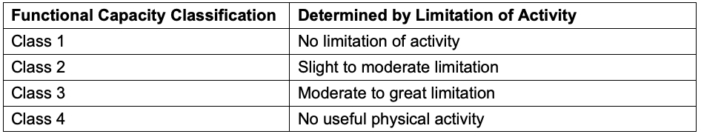
Table 2. Functional Capacity classification of CP
- Patients with CP may also have choreoathetosis, ataxia, and hypotonia to varying degrees. Muscle spasticity is thought to be related to the inadequate release of gamma aminobutyric acid at the dorsal horn of the spinal cord, resulting in a relative excess of glutamate on the alpha motor neurons that produce simultaneous contraction of agonist and antagonist mucsles.2
- CP encompasses a vast spectrum of patients; some may have severely limited physical abilities, while others have minimal deficits with normal intelligence and can assent for procedures. Patients may come to the operating room (OR) for procedures that are common for many pediatric patients, and more common in patients with CP, such as ventriculoperitoneal shunts or other orthopedic procedures to address contractures.
Clinical Features
- Clinical features of CP vary depending on the severity of symptoms and the restrictions and challenges that it can cause in daily activities. The most common clinical features of CP are listed below.
- GERD
- Chronic aspiration
- Immobility/limited mobility
- Pulmonary disease/ obstructive sleep apnea (OSA)/central sleep apnea
- Epilepsy
- Contractures
- Given the challenging medical implications of CP, this group of patients often require additional medications or considerations for these comorbidities (Table 3). CP patients with bulbar and hypothalamic dysfunction may also have ongoing issues with aspiration, sleep apnea, and hypothermia.3 The most common cause of death in CP patients is pulmonary complications.
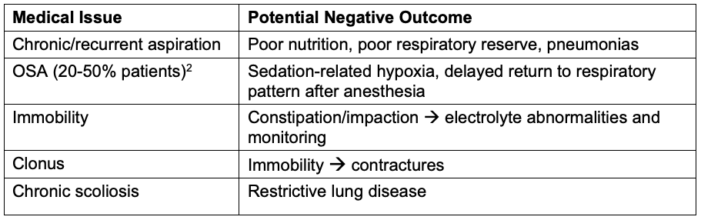
Table 3. Common medical conditions and potential negative outcomes
- Common medical procedures in CP patients are listed in Table 4.
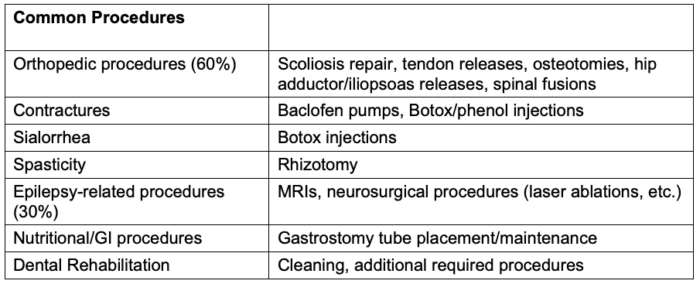
Table 4. Common medical procedures in CP patients
Anesthetic Considerations
Pharmacologic Considerations
- Patients with CP may be on anticonvulsants, corticosteroids, sedation medications, as well as ketogenic diets (Table 5). Additionally, they may have baclofen pumps that deliver intrathecal baclofen for ongoing spasticity.
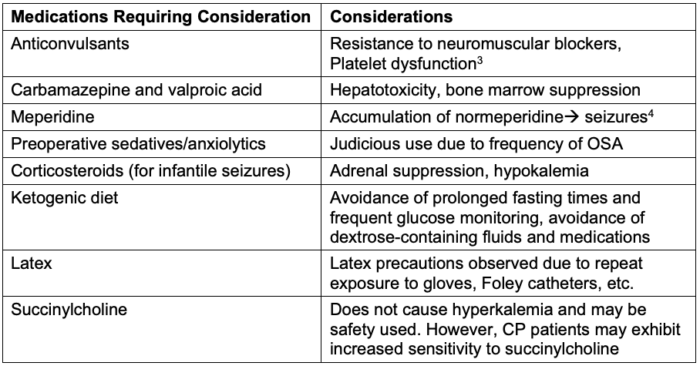
Table 5. Common medications taken by CP patients and their anesthetic considerations
Temperature Considerations
- Patients with CP have poorly regulated homeostatic systems and hypothalamic imbalances, which often lead to hypothermia perioperatively. Hypothermia can subsequently lead to poor platelet function, coagulopathy, and decreased metabolism of anesthetic medications. Maintaining the appropriate temperature is crucial for patients with CP, and there should be a low threshold for utilizing active warming strategies to mitigate this common issue.
Analgesic Considerations
- Patients with CP often undergo extensive orthopedic surgeries, so it is crucial to pay attention to pain management in the perioperative period. These patients can have pain that is undertreated, as many patients are nonverbal or have difficulty with language expression. Additionally, there are concerns about opioid-induced respiratory depression.
- Pain should be adequately managed as these patients still have a normal analgesic requirement.
- Minimum alveolar concentrations (MAC) of halothane have previously been noted to be decreased by as much as 20%.5 Delayed emergence may be noted with patients with CP, given the decreased MAC requirement and hypothermia, which can exacerbate delayed emergence.
Gastrointestinal Considerations
- Increased activity of salivary glands can result in copious secretions. Glycopyrrolate and frequent suctioning may be necessary to manage secretions. Additionally, the endotracheal tube securement should be reinforced due to increased secretions.
Respiratory Considerations
- Given the frequent diagnosis of OSA and central sleep apnea, patients with CP may be accustomed to using a home ventilator with bilevel positive airway pressure or continuous positive airway pressure. OSA is present in 20-50% of patients.2
- Anxiolytics, opioids, and other sedating medications should be administered judiciously, given the concerns around OSA/CSA.
- Lastly, decreased functional residual capacity is a consideration given the restrictive lung disease that can be present. Difficulty clearing secretions may pose an additional risk for pneumonia as well.
Developmental Considerations
- The spectrum of ability and understanding of a patient with CP may be extremely wide, which the anesthesiologist must appreciate. It is always appropriate to obtain assent for procedures for the developmentally appropriate child.
References
- McIntyre S, Goldsmith S, Webb A, et al. Global prevalence of cerebral palsy: A systematic analysis. Dev Med Child Neurol. 2022;64(12):1494-1506. PubMed
- Zuckerberg A, Yaster M. Anesthesia for pediatric orthopedic surgery. In Smith’s Anesthesia for Infants and Children. 9th edition. Philadelphia. Elsevier; 2017: 885.
- Crean P, Tirupathi S. Essentials of neurology and neuromuscular disorders. In: Coté CJ, Lerman J, Todres ID. A practice of anesthesia for infants and children. 6th edition. Philadelphia; Elsevier. 2012 562.
- Kanjia M. Cerebral palsy. In Clinical Pediatric Anesthesia: A Case-Based Handbook. 2nd edition. Oxford University Press; 2018:399-402.
- Darcey M. Anaesthetic Management of Patients with Cerebral Palsy. Semantic Scholar. Published 2010. Accessed April 25, 2024. Link
Other References
- OA Summary: Preparation and Preoperative Considerations for Neurodiverse Patients Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.