Copy link
Trigeminal Neuralgia
Last updated: 09/14/2023
Key Points
- Trigeminal neuralgia (TN) is characterized by recurrent episodes of innocuous, stimulus-evoked, brief, unilateral facial pain that occurs in one or more divisions of the trigeminal nerve.
- The pathophysiologic mechanism involves compression and demyelination of the trigeminal afferent nerve root.
- The criteria for diagnosis of trigeminal neuralgia are defined by the International Classification of Headache Disorders, Third Edition (ICHD-3) which further classifies trigeminal neuralgia as classical (CTN), secondary (STN), and idiopathic.
Introduction
- TN is characterized by recurrent episodes of innocuous, stimulus-evoked, brief, unilateral facial pain that occurs in one or more divisions of the trigeminal nerve.
- TN was previously called tic douloureux to describe the characteristic wince that TN patients exhibit during a sudden-onset and unexpected pain paroxysm.
Clinical Presentation
- The pain of TN is evoked by innocuous stimuli to the ipsilateral face. Typically, it is short-lasting, unexpected, and recurrent throughout the day.1,2
- The pain is often described as an “electric shock” or shooting pain.1,2
- Frequently, the pain is triggered by innocuous stimuli such as chewing, light touch, talking, brushing teeth, and other activities of daily living.1,2
- Episodes of pain are typically followed by a refractory period where new attacks cannot be elicited.1
- The right side of the face, specifically, the maxillary (cranial nerve V2), and mandibular (cranial nerve V3) divisions are more commonly affected.1
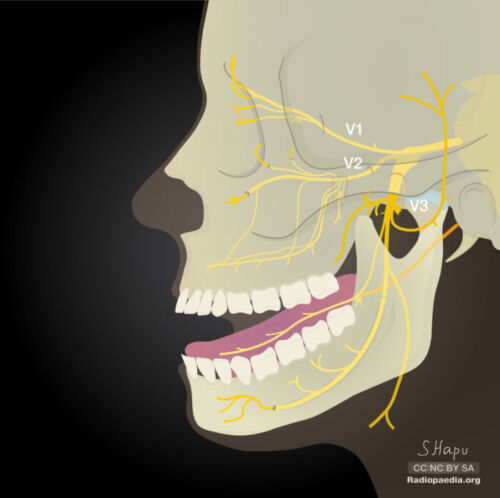
Figure 1. Divisions of the trigeminal nerve. V1- ophthalmic division, V2- maxillary division, and V3- mandibular division. Case courtesy of Sachintha Hapugoda, Radiopaedia.org. rID:54722
- Approximately half of patients experience a concomitant continuous pain, also known as background pain. This pain is dull and continuous, and it is more common in women.1
- Patients rarely experience autonomic symptoms such as tearing or rhinorrhea.1
- The overall incidence of TN is higher among women than men and increases with age.2
Pathophysiology
- The pathophysiology of TN involves demyelination, typically due to vascular compression of the nerve, as it enters the pons. This is referred to as neurovascular conflict with compression. The responsible vessel is usually the superior cerebellar artery.2 TN can also be caused by multiple sclerosis or other mechanical damage (such as secondary TN; see below).2
- The transition zone from Schwann cell to oligodendrocyte myelination is a particularly vulnerable area.
- Demyelination thins the membrane of the nerve, making it easier for ions to pass through. Additionally, the nerve is unable to pump sodium out of the cell. This causes hyperexcitability and a sudden generation of high-frequency impulses.
- A-β fibers are the type of fibers most likely to be demyelinated.
- The brain-stem neurons perceive the high-frequency impulses as pain.
Diagnosis
- The International Classification of Headache Disorders (ICHD-3 Beta) classifies TN into three subcategories: classical (CTN), secondary (STN), and idiopathic.3
- Classical TN does not have an underlying cause other than neurovascular compression.
- Secondary TN is caused by an underlying disease such as multiple sclerosis or a space-occupying tumor.
- Idiopathic TN does not show any abnormalities on MRI or in electrophysiological tests.
- The ICHD-3 Beta lists the following criteria for diagnosis of classical TN.3
A. The patient has at least three attacks of unilateral facial pain fulfilling criterion B and C below.
B. The attacks occur in one or more divisions of the trigeminal nerve, with no radiation beyond the trigeminal distribution.
C. The pain has at least three of the following four characteristics:
1. recurring in paroxysmal attacks lasting from a fraction of a second to 2 minutes
2. severe intensity
3. electric shock-like, shooting, stabbing, or sharp in quality
4. precipitated by innocuous stimuli to the affected side of the face
D. There is no clinically evident neurological deficit.
E. The attacks are not better accounted for by another ICHD-3 diagnosis.
Management
- The primary pharmacologic management for TN is carbamazepine (CMZ) or oxcarbazepine, with oxcarbazepine, both of which are sodium channel blockers also used to treat seizure disorders. These anticonvulsants result in stabilization of hyperexcited neuronal membranes and inhibition of repetitive firing.2
- CMZ has been shown to have a higher incidence of dermatologic reactions, such as Stevens-Johnson syndrome and toxic epidermal necrosis. CMZ also has a black box warning for agranulocytosis and aplastic anemia and monitoring of blood levels via complete blood cell (CBC) testing should be utilized particularly early in the treatment course.
- Another widely used treatment is repetitive transcranial magnetic stimulation.
- Lamotrigine and pimozide are utilized for refractory cases of TN.
- Surgical treatments include many types of rhizotomy and microvascular decompression depending on the patient’s previous medical history and presentation.4
- Balloon compression:
- Affected root of the trigeminal nerve is compressed at its exit point from the skull resulting in relief for roughly 1-2 years. Baloon compression can be performed as an inpatient or outpatient procedure.
- Glycerol injection:
- Glycerol is injected at the exit point of the mandibular division of the trigeminal nerve. This leads to damage of the insulatory fibers of the trigeminal ganglion leading to relief. This procedure is the least likely to have lasting relief; however, it can be performed multiple times.
- Radiofrequency thermal lesioning:
- The affected branch of the trigeminal nerve is heated with an electrode to the desired point of sensory loss (usually loss of sharp pain and preservation of touch. This treatment has an increased risk of anesthesia dolorosa.
- Stereotactic radiosurgery:
- Radiation is focused on the point the trigeminal nerve exits the pons to lesion only the sensory component of the nerve. Relief usually comes weeks after the procedure. Less than half of those successfully treated have a recurrence within 3 years.
- Microvascular decompression:
- This is the most invasive procedure; however, microvascular decompression offers the lowest probability of pain recurrence. It is now favored for most cases of TN that do not respond to medications. After a suboccipital craniotomy, the neurosurgeon uses microscopy to expose the trigeminal nerve emerging from the ventral pons and then identifies the vessel compressing the nerve. Subsequently, a small sponge is placed between the trigeminal nerve and the vessel (usually artery) that is compressing it. Roughly half of the successful procedures will have a recurrence of pain in 10-15 years.
- Balloon compression:
References
- Maarbjerg S, Di Stefano G, Bendtsen L, et al. Trigeminal neuralgia - diagnosis and treatment. Cephalalgia. 2017;37(7):648-57. PubMed
- Cruccu G, Di Stefano G, Truini A. Trigeminal neuralgia. N Engl J Med. 2020;383(8):754-62. PubMed
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013; 33: 629–808. PubMed
- Trigeminal neuralgia fact sheet. National Institute of Neurological Disorders and Stroke. Published June 2013. Accessed November 2022. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.