Copy link
Postoperative Visual Loss
Last updated: 01/27/2023
Key Points
- Postoperative visual loss (POVL) is a rare but serious complication of nonophthalmic surgeries.
- The most common causes of POVL include ischemic optic neuropathy, central retinal artery occlusion, and cortical blindness.1
- Several factors such as intraoperative hypotension, blood loss, patient positioning, and surgical duration have been associated with postoperative vision loss.
- The highest rates of postoperative visual loss are reported after cardiac and spinal surgeries.1
Etiology
Ischemic Optic Neuropathy
- Ischemic optic neuropathy (ION) is the most common cause of POVL and is presumed to be due to impaired blood supply to the optic nerve.
- ION is classified as anterior ION or posterior ION, depending on the affected segment of the optic nerve.
- Anterior ION represents an acute ischemic disorder of the optic nerve head supplied by the posterior ciliary artery.
- Posterior ION is an acute optic neuropathy due to ischemia in the retrobulbar portion of the optic nerve.
- ION presents with painless vision loss that may be unilateral or bilateral and includes symptoms ranging from no light perception to color vision deficits, visual field defects, and decreased visual acuity.
- Symptoms are typically reported within one to two days after surgery and frequently upon awakening, although they may be recognized as late as 12 days postoperatively, particularly in patients who remain sedated with the need for postoperative mechanical ventilation.1
- Fundoscopic exam: Anterior ION is typically associated with optic disc edema and flame-shaped hemorrhage upon symptom onset. In posterior ION, the optic disc often appears normal initially, with mild disc edema days later.2
Central Retinal Artery Occlusion
- Central retinal artery occlusion (CRAO) is the blockage of the central retinal artery, resulting in retinal hypoperfusion, rapidly progressive cellular damage, and vision loss.
- Causes include embolism, retrobulbar hemorrhage, and external eye compression resulting in raised intraocular pressure and impaired blood flow through the central retinal artery.
- Patients present with sudden, painless, monocular vision loss.
- On fundoscopy, the retina will appear diffusely pale with a cherry red central spot.
Cortical Blindness
- Cortical blindness is loss of vision caused by ischemia in the visual cortex or afferent sensory pathways.
- This can result from emboli, severe hypotension, acute anemia, hypoxia, or a combination of these factors.3
- Cortical blindness may present as painless vision loss ranging from partial to complete with retention of pupillary reactions to light.
- Fundoscopic exam is usually normal.
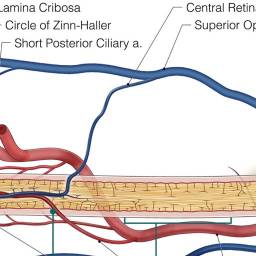
Figure 1. Sites of various postoperative ocular injury. Source: Mendel E, Stoicea N, Rao R, et al. Revisiting postoperative vision loss following non-ocular surgery: A short review of etiology and legal considerations. Frontiers in Surgery. 2017; 4:34. CC BY.
Risk Factors
Ischemic Optic Neuropathy
- Relative hypotension
- Significant, prolonged hypotension can result in ischemic injury to the optic nerve.
- Significant blood loss
- Significant blood loss increases fluid shifts, capillary leak, interstitial edema, and systemic inflammation, as well as predisposes to reduced cardiac output and end-organ blood flow.5
- Longer anesthetic duration
- Longer anesthetic length is associated with an increased risk of postoperative vision loss, likely due to an increased risk of prolonged hypotension, blood loss, and subsequent fluid resuscitation.5
- Surgical procedure
- Highest rates of postoperative vision loss are seen with cardiac, spinal, head and neck surgery.6
- Anterior ION is most commonly associated with cardiac surgery.
- Posterior ION is most commonly associated with spinal surgery.
- Patient positioning
- Prone positioning increases intraocular pressure as well as central venous pressure by compressing the abdomen and impairing venous drainage via the ophthalmic veins, a complication further exacerbated by obesity.2
- Use of the Wilson frame predisposes patients to increased venous congestion in the optic canal due to the lower positioning of the head compared to the body.5
- Prolonged steep Trendelenburg positioning may also decrease cranial venous outflow, causing local capillary bed stasis in the eyes.2
- Obesity
- Due to increased abdominal girth, obese patients may have increased intraabdominal and central venous pressures in the prone position, thereby causing increased cerebral venous pressure. Subsequently, systemic venous return and cardiac output are reduced, leading to decreased end-organ blood flow.5
- Male gender
Central Retinal Artery Occlusion
- Ocular compression
- Sustained increases in intraocular pressure may impede or stop blood flow in the central retinal artery.
- Various factors that increase the vulnerability for external compression include altered facial anatomy, osteogenesis imperfecta, and exophthalmos.6
- For prone procedures, the horseshoe headrest may increase the risk of CRAO as the edges of the headrest are very close to the eyes and may cause globe compression.
- Embolism
- In cardiac and head and neck surgery, the etiology of CRAO is often embolic. Identified risk factors for embolism resulting in CRAO include hyperlipidemia, diabetes, carotid stenosis, stroke, aging, and hypercoagulable states.
Cortical Blindness
- Embolism
- Cortical blindness is most often associated with cases with high embolic loads such as cardiopulmonary bypass, spine, bone and joint surgeries.
- Patient comorbidities such as hypertension, hyperlipidemia, diabetes, carotid stenosis, and hypercoagulable states increase the risk of emboli.
- Cerebral hypoperfusion
- Risk factors include intraoperative hypotension, significant blood loss, hypoxia, anemia.
References
- Anesthetic Complications. In: Butterworth JF, IV, Mackey DC, Wasnick JD. eds. Morgan & Mikhail's Clinical Anesthesiology. 6e. New York, McGraw Hill; 2013: 1244-45.
- Kla MK, Lee LA. Perioperative Visual Loss. Best Pract Res Clin Anaesthesiol. 2016;30(1):69-77. PubMed
- Aldrich MS, Alessi AG, Beck RW, Gilman S. Cortical blindness: etiology, diagnosis, and prognosis. Ann Neurol. 1987;21(2):149-58. PubMed
- Mendel E, Stoicea N, Rao R, et al. Revisiting postoperative vision loss following non-ocular surgery: A short review of etiology and legal considerations. Frontiers in Surgery. 2017; 4:34. PubMed
- Postoperative Visual Loss Study Group. Risk factors associated with ischemic optic neuropathy after spinal fusion surgery. Anesthesiology. 2012; 116(1):15-24. PubMed
- Grover V, Jangra K. Perioperative vision loss: A complication to watch out. J Anaesthesiol Clin Pharmacol. 2012;28(1):11-16. PubMed
- Roth S. Perioperative visual loss: what do we know, what can we do?. Br J Anaesth. 2009;103 Suppl 1(Suppl 1): i31-i40. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.