Copy link
Perioperative Care of the Patient with Obesity
Last updated: 04/06/2023
Key Points
- Patients with obesity have multiple comorbidities and a thorough preoperative evaluation should be performed to optimize the patient’s status and mitigate risk.
- Atelectasis-induced hypoxemia, hypercarbia, and adequate end-organ perfusion should be carefully monitored in the patient with obesity.
- Patients with obesity are at increased risk for postoperative pulmonary complications (PPC) which can lead to increased postanesthesia care unit (PACU) time, increased hospitalization length of stay, and mortality.
Introduction
- Over 40% of the adult population in America is obese. Patients with obesity frequently have concurrent comorbidities such as heart disease, diabetes, and pulmonary dysfunction. The presence of these comorbidities increases the risk for anesthesia.
- A thorough preoperative evaluation allows the clinician to optimize the patient’s health prior to anesthesia to mitigate risk.
Preoperative Assessment
- Preoperative assessment of patients with obesity should be thorough and prioritize the identification of pathophysiology with anesthetic implications. The history and physical examination of the patient with obesity can be approached in a systems-based manner as outlined in Table 1.
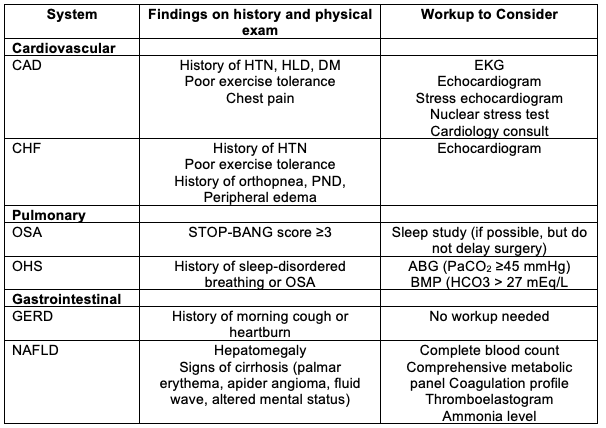
Table 1. Preoperative Evaluation of the Patient with Obesity. ABG, arterial blood gas; BMP, basic metabolic panel; CAD, coronary artery disease; CHF, congestive heart failure; DM, diabetes mellitus; EKG, electrocardiogram; GERD, gastroesophageal reflux disease; H&P, history and physical examination; HLD, hyperlipidemia; HTN, hypertension; NAFLD, nonalcoholic fatty liver disease; OSA, obstructive sleep apnea; OHS, obesity hypoventilation syndrome; PND, paroxysmal nocturnal dyspnea
Airway
- A critical component of the preoperative assessment of patients with obesity is a detailed airway exam. Several risk factors are associated with difficult intubation and/or mask ventilation. These airway risk factors are outlined in Table 2 and illustrated in Figure 1.
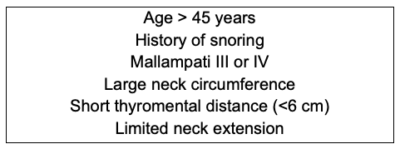
Table 2. Airway Risk Factors
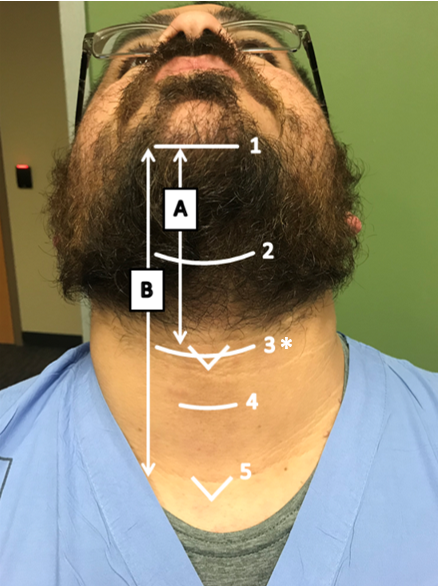
Figure 1. External neck measurements
1, Mentum; 2, Hyoid; 3, Thyroid; 4, Cricoid; 5, Sternal notch;
A, Thyromental distance; B, Sternomental distance.
*Neck circumference measured at the level of the thyroid cartilage
- Patients with obesity have a significantly reduced functional residual capacity (FRC), which results in rapid desaturation following induction.
- Proper positioning of patients before laryngoscopy is important. One can use the 25-degree reverse Trendelenburg position or the ramped position where the patients’ external auditory meatus is at the same level as the sternum.
- Apneic oxygenation with 15 L/minute oxygen through a nasopharyngeal airway and a standard nasal cannula can significantly increase the safe apneic duration during induction of anesthesia.1
- Both direct laryngoscopy and video laryngoscopy can be used to facilitate endotracheal intubation. There is no conclusive evidence that video laryngoscopy is superior to direct laryngoscopy in patients with obesity.3

Figure 2. Apneic oxygenation during laryngoscopy and intubation
Monitoring and Mechanical Ventilation
- Monitoring oxygenation, ventilation, and circulation in the patient with obesity can have unique challenges.
- Atelectasis-induced hypoxemia is a risk that should be monitored intraoperatively. Patients with obesity are at an increased risk of atelectasis due to decreased total lung capacity, vital capacity, and functional residual capacity. Application of positive end-expiratory pressure (PEEP) intraoperatively minimizes atelectasis. PEEP titration can be difficult in patients with obesity, but titration of PEEP using esophageal manometry has shown to be beneficial in this population.2 Use of esophageal manometry, a surrogate for pleural pressures, allows for monitoring of transpulmonary pressure, and alveoli are kept open if the transpulmonary pressure P L (i.e., the difference between airway pressure and pleural pressure) exceeds atmospheric pressure.
- Protective mechanical ventilation should be used in patients with obesity using low tidal volumes (6-8 mL/kg of ideal body weight), low to moderate levels of PEEP, and titrating the inspired oxygen fraction to achieve oxygen saturations of 92-95%.4
- Capnography has limitations in patients with obesity due to a greater expired CO2/arterial CO2 gradient than in lean subjects. Furthermore, patients with obesity have an increased production of CO2 secondary to high oxygen consumption (VO2). One may consider arterial blood gasses to guide ventilation settings.
- When monitoring circulation, the goal is to maintain adequate end-organ perfusion. Currently, standard noninvasive blood pressure (NIBP) is our best available routine surrogate measurement but is vulnerable to greater inaccuracy in patients with obesity compared to nonobese patients.3 In patients with obesity, forearm NIBP exhibits better measurement performance than upper arm or lower leg readings.5 Furthermore, NIBP measured at the wrist has the highest correlation with radial arterial catheter blood pressure measurements.6
Extubation and Postoperative Care
- When extubating patients with obesity, one must ensure adequate tidal volumes are being achieved, which can be facilitated by positioning the patient in the ramped position or 25-degree reverse Trendelenburg position prior to extubation.3
- If there is a concern for obstruction after extubation, use of an oral airway or nasal trumpet is advised.
- Patients with obesity have altered respiratory mechanics, which places them at an increased risk for postoperative pulmonary complications (PPC), which can range from mild (unplanned need for oxygen) to severe (acute respiratory distress syndrome or need for reintubation). PPCs are associated with increased PACU time, increased length of hospitalization, and mortality.
- Given their increased risk for PPCs, patients with obesity should be carefully monitored in the PACU, with specific attention to recurrent respiratory events, including apnea, bradypnea, pain-sedation mismatch, CO2 retention, and oxygen desaturation. Should postoperative respiratory events persist, an inpatient admission may be warranted.4
References
- Moon TS, Tai K, Kim A, et al. Apneic oxygenation during prolonged laryngoscopy in obese patients: a randomized, double-blinded, controlled trial of nasal cannula oxygen administration. Obes Surg. 2019; 29(12), 3992-9. PubMed
- Eichler, L, Truskowska, K, Dupree, A, et al. Intraoperative ventilation of morbidly obese patients guided by transpulmonary pressure. Obes Surg. 2018; 28(1), 122-9. PubMed
- Moon, TS, Van de Putte, P, De Baerdemaeker, L, et al. The obese patient: facts, fables, and best practices. Anesth Analg. 132(1), 53-64. PubMed
- Bazurro S, Simone L, Pelosi P. Perioperative management of obese patient. Curr Opin Crit Care. 2018; 24(6): 560-7. PubMed
- Schumann R, Meidert AS, Bonney I, et al. Intraoperative blood pressure monitoring in obese patients. Anesthesiology. 2021; 134(2): 179-88. PubMed
- Mostafa MM, Hasanin AM, Alhamade F, et al. Accuracy and trending of non-invasive oscillometric blood pressure monitoring at the wrist in obese patients. Anaesth Critl Care Pain Med. 2020; 39(2), 221-7. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.