Copy link
Vasopressors and Inotropes: Overview and Selection of Agents
Last updated: 10/16/2025
Key Points
- Shock is a state of inadequate oxygen delivery to meet the body’s metabolic demands, which, if untreated, can lead to multiple system organ dysfunction.
- There are four main types of shock: distributive, cardiogenic, hypovolemic, and obstructive.
- Vasopressors increase systemic vascular resistance, inotropes increase cardiac output (CO), and mixed agents increase both.
- Selection of the appropriate agent depends on the type of shock.
Types of Shock and Use of Vasoactive Infusions
- Shock is a condition characterized by inadequate oxygen delivery to meet metabolic demands at the cellular and tissue levels.1 Shock is initially reversible but becomes irreversible if left untreated. The consequences of unmet demands include circulatory instability, lactic acidosis, severe systemic hypotension, and multiple system organ dysfunction.
- There are different types of shock, which are categorized based on the etiology of circulatory failure. The various kinds of shock and effective vasoactive infusions are summarized in Table 1.2
- Distributive: shock secondary to severe peripheral vasodilation, despite possible increased CO.
- Cardiogenic: shock secondary to reduced CO from intracardiac dysfunction.
- Hypovolemic: shock secondary to reduced CO from decreased intravascular volume.
- Obstructive: shock secondary to reduced CO from extracardiac causes, limiting forward circulatory flow.
- Please see the OA summary “Shock: Overview and Classification.” Link
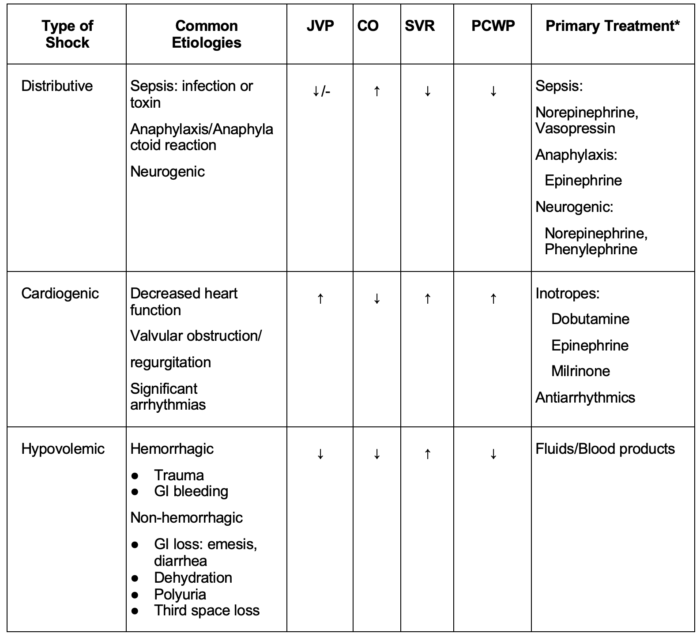
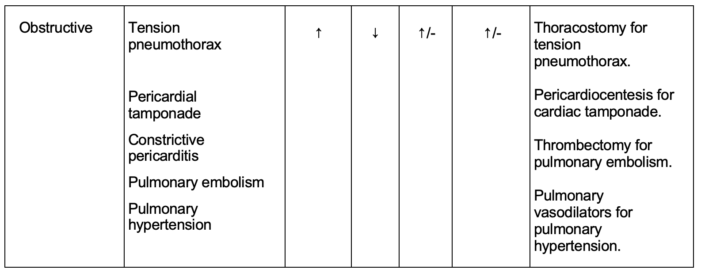
Table 1. Etiologies, clinical features, and primary treatment of different types of shock.
Abbreviations: JVP, jugular venous pressure, CO, cardiac output, SVR, systemic vascular resistance, PCWP, pulmonary capillary wedge pressure, GI, gastrointestinal. *Primary treatment refers to immediate intervention to stabilize a patient.
Vasopressors: Mechanism of Action
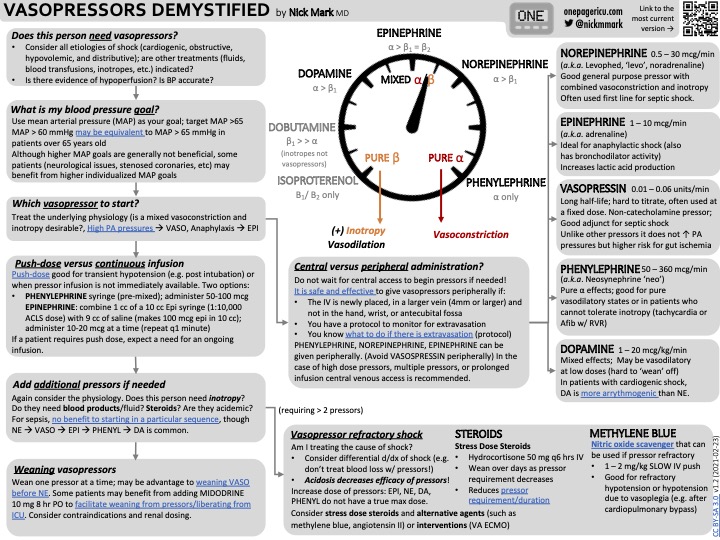
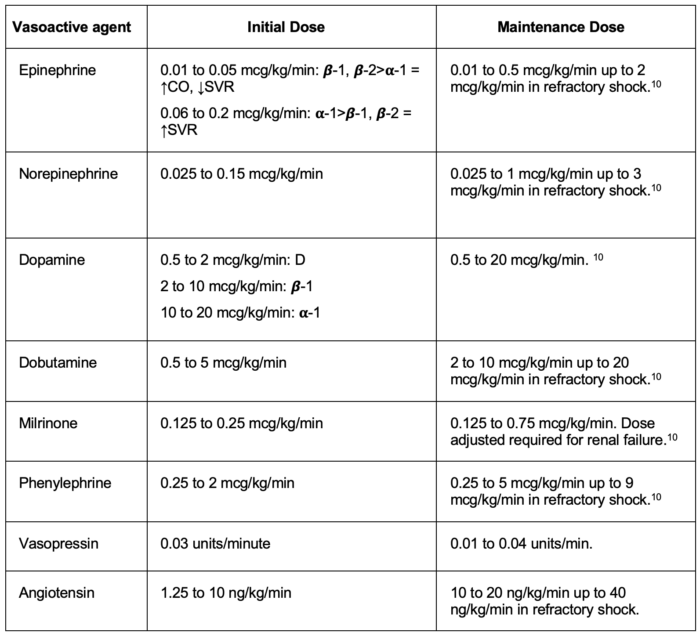
- When supporting a patient in shock with hemodynamic instability, three main categories of vasoactive agents can be used: pure vasopressors, mixed vasopressor and inotropes (often called inopressor), and pure inotropes.
- Pure vasopressor: Predominantly increases vascular tone or systemic vascular resistance (SVR) without significant impact on cardiac contractility (examples: phenylephrine, vasopressin, angiotensin II)
- Mixed vasopressor and inotrope: Increases SVR and cardiac contractility (examples: epinephrine, norepinephrine, dopamine)
- Pure inotrope: Predominantly increased cardiac contractility (examples: milrinone, isoproterenol, dobutamine)
- Table 2 summarizes the mechanism of action and effects of vasopressors (pure and mixed inotropes).1-3
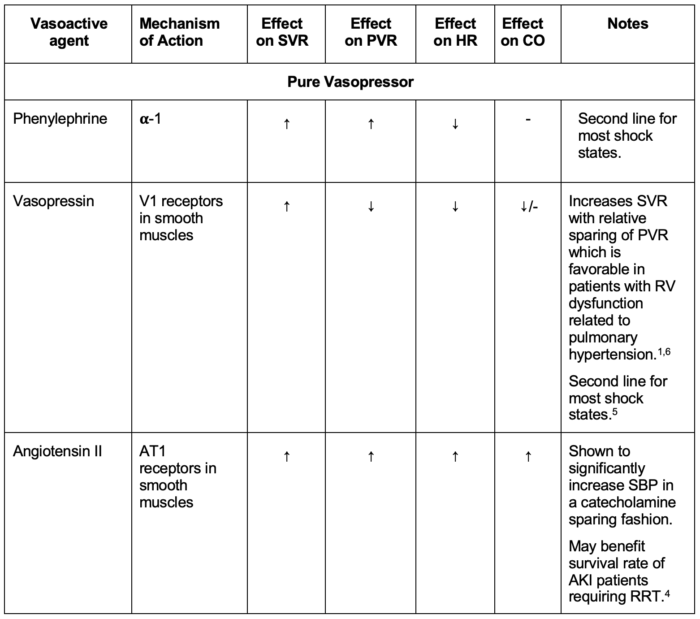
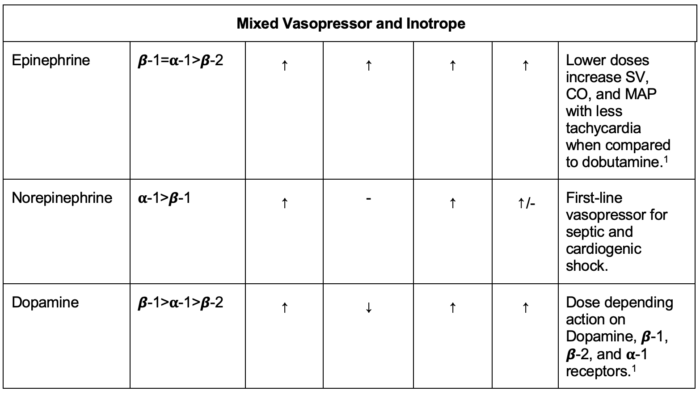
Table 2. Mechanism of action and effects of vasopressors
Abbreviations: PVR, pulmonary vascular resistance, SVR, systemic vascular resistance, RV, right ventricle, SBP, systemic blood pressure, AKI, acute kidney injury, RRT, renal replacement therapy, SV, stroke volume, CO, cardiac output, MAP, mean arterial pressure.
- Vasopressors induce vasoconstriction, increasing the mean arterial pressure (MAP) by augmenting the SVR. MAP = (CO × SVR) + CVP, where CO is CO and CVP is central venous pressure. The mixed vasopressors and inotropes increase the MAP by increasing both the SVR and the CO.
- The vasopressors and mixed vasopressor inotropes most commonly used are phenylephrine, epinephrine, norepinephrine, dopamine, vasopressin, and angiotensin II.
- Phenylephrine is an α-1 agonist that induces vasoconstriction, reflex bradycardia, and decreased CO.
- Norepinephrine acts on α-1 and α-2 receptors more than β-1 and β-2 receptors, increasing MAP without decreasing CO.
- Epinephrine exhibits dose-dependent activity on all adrenergic receptors, resulting in a more pronounced vasoconstriction with higher doses. Epinephrine acts on β receptors at a lower dose, and on α receptors at a higher dose.
- Dopamine acts on dopaminergic and adrenergic receptors, increasing the SVR at higher doses.
- Vasopressin produces vasoconstriction by acting on V1 receptors in the vascular smooth muscles. Vasopressin is used as the second line for septic shock.5
- Angiotensin II produces vasoconstriction by stimulating AT1 receptors in the vascular smooth muscles.
Inotropes: Mechanism of Action
- Inotropes include both adrenergic and non-adrenergic agents. The inotropic adrenergic agents include epinephrine, dopamine, dobutamine, and isoproterenol. The non-adrenergic inotropic agents include milrinone, digoxin, and levosimendan.
- Epinephrine is a mixed inotrope and vasopressor with affinity for both α and β receptors. Low dose of epinephrine acts on β receptors, while at high doses, it acts on α receptors.
- Dopamine is a precursor of epinephrine and norepinephrine and acts in a dose-dependent fashion on dopaminergic receptors and α and β receptors. Dopamine acts on dopamine receptors at lower doses, β receptors at medium doses, and α receptors at higher doses.
- Dobutamine is a synthetic adrenergic agent that acts on β-1 more than β-2 receptors.
- Isoproterenol is a synthetic non-selective β-adrenergic receptor agonist used primarily for treating bradycardia.
- Milrinone is a phosphodiesterase inhibitor that increases cyclic adenosine monophosphate (cAMP), which stimulates cardiomyocytes and enhances CO; it also has a vasodilatory effect in smooth muscles, decreasing SVR and PVR.
- Digoxin is a Na+/K+ pump inhibitor that increases the intracellular calcium in cardiac myocytes, leading to increased contractility and decreased chronotropy.
- Levosimendan increases the sensitivity of cardiac troponin C to calcium ions within cardiomyocytes, leading to enhanced contractility.
- Table 3 summarizes the mechanism of action and effects of commonly used inotropes.
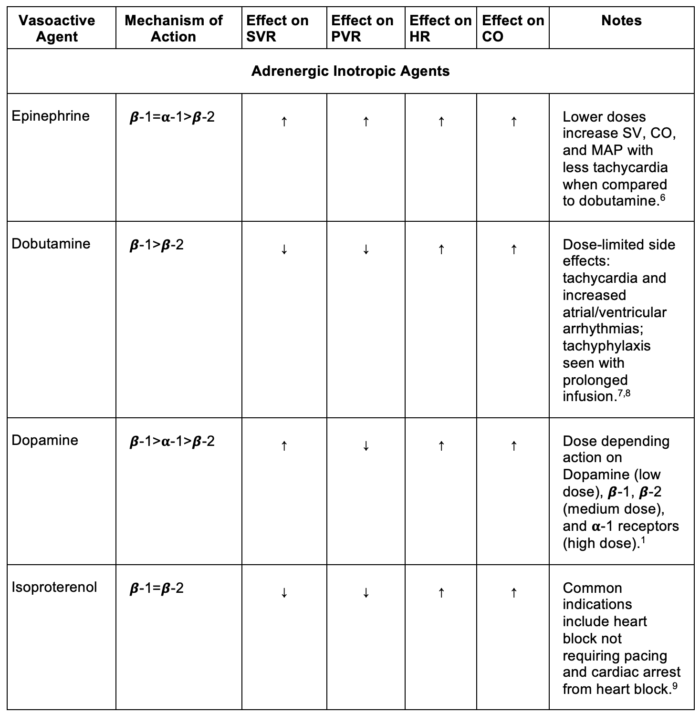
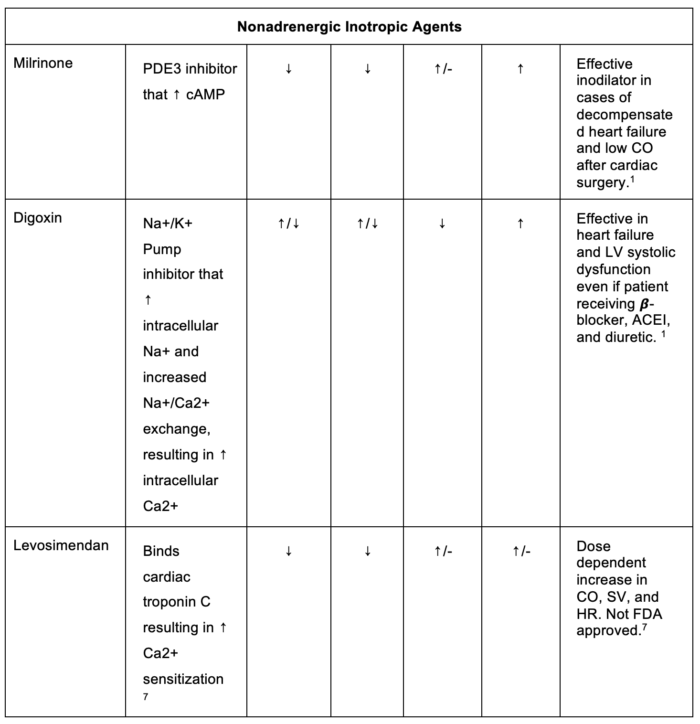
Table 3. Mechanism of action and effects of inotropes.
Abbreviations: PVR, pulmonary vascular resistance, SVR, systemic vascular resistance, SV, stroke volume, CO, cardiac output, PDE3, phosphodiesterase 3, cAMP, cyclic monophosphate, MAP, mean arterial pressure, LV, left ventricle, ACEI, angiotensin-converting enzyme inhibitor, HR, heart rate, FDA, Food and Drug Administration.
References
- Kaplan JA, Augoustides JGT, Gutsche JT, eds. Kaplan’s Cardiac Anesthesia: Perioperative and Critical Care. 8th edition. Elsevier; 2024.
- Gropper MA, Miller RD, Cohen NH, eds. Miller’s Anesthesia. Ninth edition. Elsevier; 2020.
- Cullen BF. Barash, Cullen, and Stoelting’s Clinical Anesthesia. 9th ed. Wolters Kluwer Health; 2023.
- Khanna A, English SW, Wang XS, et al. Angiotensin II for the treatment of vasodilatory shock. N Engl J Med. 2017;377(5):419-430. PubMed
- Russell JA, Walley KR, Singer J, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358(9):877-87. PubMed
- Jentzer JC, Coons JC, Link CB, Schmidhofer M. Pharmacotherapy update on the use of vasopressors and inotropes in the intensive care unit. J Cardiovasc Pharmacol Ther. 2015;20(3):249-260. PubMed
- McCann P, Hauptman PJ. Inotropic therapy. Medical Clinics of North America. 2012;96(5):943-954. PubMed
- Follath F, Cleland J, Just H, et al. Efficacy and safety of intravenous levosimendan compared with dobutamine in severe low-output heart failure (the LIDO study): a randomised double-blind trial. Lancet. 2002;360(9328):196-202. PubMed
- Szymanski MW, Singh DP. Isoproterenol. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. Link
- Manaker S, Teja B. Use of vasopressors and inotropes. In: UpToDate [Internet]: UpToDate Publishing, 2025, April. Link
- Patel P, Sanghavi DK, Morris DL, et al. Angiotensin II. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.