Copy link
Vasopressin
Last updated: 08/20/2025
Key Points
- Vasopressin is a hormone produced by the posterior pituitary that causes potent vasoconstriction and reabsorption of water at the renal collecting duct through the activation of G protein-coupled receptors, making it vital to maintaining intravascular volume and cardiac homeostasis.
- Vasopressin has clinical utility in the management of refractory hypotension in patients on angiotensin-converting enzyme (ACE) inhibitors, hemorrhagic shock, cardiopulmonary bypass-associated vasoplegia, and septic shock. It is particularly useful in settings where renal protection is a priority.
- Potential side effects include extravasation-induced tissue necrosis, gastrointestinal ischemia at high doses, thrombosis, hypersensitivity reactions, and hyponatremia.
Biochemical Information
Physiochemical Properties
- Vasopressin, also known as arginine vasopressin or antidiuretic hormone (ADH), is a nonapeptide that is freely soluble in water and dilute acids.
- It exists as a positively charged molecule at physiological pH but is highly sensitive to enzymatic degradation by peptidases in the gastrointestinal (GI) tract, high temperatures, and high pH.
- It is a hydrophilic molecule that exhibits a very low degree of protein binding.1
Mechanism of Action and Systemic Effects
- Vasopressin activates V1, V2, and V3 receptors, which act through G protein-coupled receptors to release downstream second messengers essential for maintaining intravascular volume and cardiac homeostasis.
- V1 receptors: cause robust vasoconstriction, particularly in skin, muscle, and splanchnic beds, while sparing pulmonary vasculature
- V2 receptors: increase water reabsorption at the renal collecting duct to preserve intravascular volume and concentrate urine
- V3 receptors: stimulate ACTH release, activating cortisol-induced stress response2
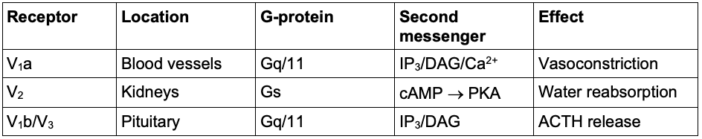
Table 1. Summary of vasopressin receptor subtypes, location, and physiological effects.2,9 Abbreviations: IP3, inositol triphosphate, DAG, diacylglycerol, cAMP, cyclic adenosine monophosphate, PKA, protein kinase pathway, ACTH, adrenocorticotrophic hormone
- Vasopressin is released in response to physiological stressors, including hypernatremia and/or hypovolemia, to maintain tonicity homeostasis.
- ADH plays an insignificant role when sympathetic tone and the renin-angiotensin aldosterone system are functioning normally, but acts as a “backup” system when they are compromised during different states of shock or catecholamine depletion.
- Systemic hypotension is the most potent activator.
- Pain, nausea, hypoglycemia, nicotine, and opiates contribute to the release of ADH, while ethanol inhibits ADH release, resulting in increased diuresis.3
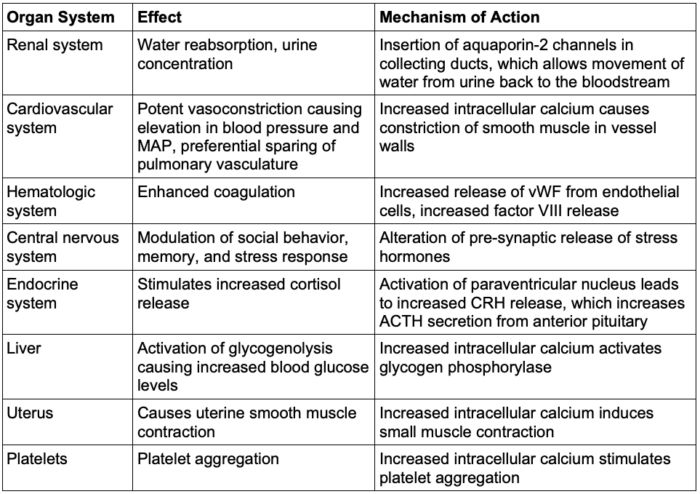
Table 2. Systemic effects of vasopressin3,4,8,9 Abbreviations: vWF = von Willebrand factor, CRH = corticotropin-releasing hormone, ACTH = adrenocorticotropic hormone, MAP = mean arterial pressure.
Pharmacokinetics
- Absorption of vasopressin is primarily intravenous (IV), intramuscular, or subcutaneous. Oral absorption is poor due to the destruction of the compound by trypsin within the gastrointestinal tract.
- IV administration causes the most rapid onset, with peak effects occurring within 15 minutes.
- The antidiuretic effect of vasopressin lasts for 2-8 hours and is highly variable after subcutaneous or intramuscular administration. Pressor effects begin to wane within 20 minutes of stopping IV infusion of vasopressin.
- Vasopressin is distributed within the extracellular fluid and exhibits minimal binding to plasma proteins.
- Vasopressin is primarily metabolized by the liver and kidneys.4
- Vasopressin must be refrigerated at 2-8 degrees Celsius.3
Clinical Uses
Refractory Hypotension (Vasoplegia)
- Vasopressin may be used after fluids and other vasopressors have failed to elevate the patient’s systemic vascular resistance (SVR).
- Vasopressin is especially useful in patients taking ACE inhibitors.
- Low-dose infusion or boluses (0.01-0.04 U/min or 0.5-1U bolus) can be used to reverse refractory hypotension in patients on ACE inhibitors or with vasodilatory shock during general anesthesia, minimizing reliance on catecholamines and the risk of ischemia.1
Hemorrhagic Shock
- Low-dose vasopressin infusion (0.04 U/min) rapidly increases SVR, mean arterial pressure, and urine output in cases of perioperative hemorrhagic shock.
- Urine output increases through constriction of the efferent arteriole, rather than constriction of the afferent caused by other pressors, which elevates glomerular filtration rate.
- It decreases the need for exogenous catecholamines while simultaneously preserving cardiac function and critical organ blood flow.5
- Vasopressin is especially useful as an adjunct in the case of GI hemorrhage caused by esophageal varices, inflammatory bowel diseases, peptic ulcer disease, acute gastritis, colitis, colonic diverticulosis, Mallory-Weiss tear, or intestinal perforation.4
Cardiopulmonary Bypass (CPB)-Associated Vasoplegia
- CPB is associated with increased nitric oxide production and severe vasopressin depletion. Administration of vasopressin is recommended as a first-line adjunct to norepinephrine.6
Septic Shock
- Sepsis may cause decreased levels of ADH, which makes maintenance of intravascular volume difficult, in addition to systemic vasodilation.
- Vasopressin release is stimulated by both hypoxemia and acidosis, leading to its depletion in cases of prolonged shock.2
- Vasopressin is considered a first-line adjunct to norepinephrine.
- Reduced norepinephrine infusion rates with no difference in mortality in patients with severe sepsis.
- Decreased mortality by 10% in patients with low-severity septic shock.3
- The potency of vasopressin is maintained in the setting of hypoxia and acidosis, while other vasopressors may not be as effective, making it particularly useful in cases of severe shock.
Diabetes Insipidus
- The lack of ADH release from the posterior pituitary is the cause of central diabetes insipidus (DI), resulting in polyuria, polydipsia, dehydration, and electrolyte abnormalities.
- Desmopressin (DDAVP), a synthetic hormone resembling vasopressin, can be used to treat central DI. DDAVP is generally preferred over vasopressin as it does not lead to systemic hypertension.
- Neither vasopressin nor DDAVP can be used to treat primary nephrogenic DI, which is due to a defect in the V1 receptor at the kidney rather than inadequate release of ADH.3,4
von Willebrand Disease and Hemophilia A
- Desmopressin can be used to increase the secretion of von Willebrand factor, which promotes adhesion of collagen on the endothelial surface to glycoprotein Ib receptors on platelets. It is an effective treatment for the bleeding diathesis associated with von Willebrand disease.
- It also promotes the release of factor VIII from endothelial cells, which effectively combats the inherited or acquired deficiency of this factor seen in Hemophilia A.3
- Vasopressin’s primary role as an adjunctive therapy remains supported, particularly when renal protection is paramount.7
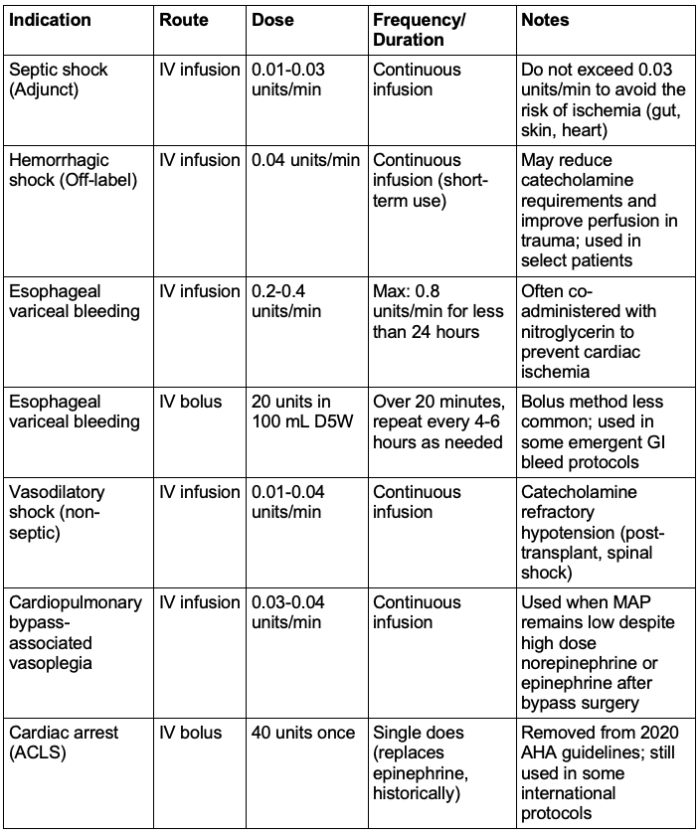
Table 3. Clinical indications of vasopressin with associated route of administration, dose, frequency/duration, and additional comments. Note that the use of vasopressin is no longer indicated in ACLS; however, it is included in the table for historical purposes.4,10 Abbreviations: ACLS = Advanced Cardiac Life Support, AHA = American Heart Association, MAP = mean arterial pressure.
Side Effects
Extravasation Risk
- Local tissue necrosis can occur if peripheral infiltration occurs.
- Administration through a central line is preferred.3
Ischemic Phenomena
- Particularly high doses have been shown to provoke vasospasm, demonstrated in intramyometrial injections.8
- Risk for ischemia to the GI tract, skin, and myocardium during prolonged infusions as doses exceeding 0.03 units/min4
Thrombosis Risk
- Activation of V2 receptors on endothelial cells activates the release of endothelial vWF, causing enhanced platelet aggregation.
- Caution should be taken in patients with coronary artery disease, a history of thrombosis, or other thrombotic risk factors.3,9
Hypersensitivity Reaction
- Urticaria, angioedema, bronchoconstriction, fever, rash, wheezing, dyspnea, and anaphylaxis have been reported.3,4
Hyponatremia
- Excessive water reabsorption at the collecting duct may lead to hyponatremia that can become severe. Monitor for altered mental status and seizures that could potentially progress to coma and death.
- Judicious dosing and extra caution should be taken in patients with a history of seizure disorder, heart failure, coronary artery disease, and renal disease, where rapid addition of extracellular fluid could exacerbate the existing condition.4
References
- National Center for Biotechnology Information. PubChem compound summary for CID 11979316, Vasopressin. Accessed July 1, 2025. Link
- Holmes CL, Landry DW, Granton JT. Science review: Vasopressin and the cardiovascular system part 1--receptor physiology. Crit Care. 2003;7(6). PubMed
- Cuzzo B, Padala SA, Lappin SL. Physiology, Vasopressin. In StatPearls (Internet). Treasure Island (FL). StatPearls Publishing. 2023. Link
- Vasopressin. Drugs.com. Updated February 1, 2024. Accessed July 1, 2025. Link
- Tsuneyoshi I, et al. Low-dose vasopressin infusion in patients with severe vasodilatory hypotension after prolonged hemorrhage during general anesthesia. J Anesth. 2005;19(2):170–3. Link
- Muhammad R, Dharmadjati BB, Mulia EPB, et al. (2022). Vasoplegia: Mechanism and management following cardiopulmonary bypass. Eurasian J Med. 2022; 54(1), 92–99. Link
- Sedhai YR, et al., Vasopressin versus norepinephrine as the first-line vasopressor in septic shock: A systematic review and meta-analysis. J Clin Transl Res. 2022.8(3): 185-99. PubMed
- Jayaraman L, Sinha A, Punhani D. Intramyometrial vasopressin: Anesthesiologists' nightmare. J Anaesthesiol Clin Pharmacol. 2013;29(1):135-136. Link
- Hall JE. Antidiuretic hormone (vasopressin). In: Guyton and Hall Textbook of Medical Physiology. 14th ed. Elsevier; 2021:938-939. Link
- Voelckel W G. (2025). Vasopressin in traumatic hemorrhagic shock. Curr Opin Anaesthesiol. 2025: 38(2): 81-92. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.