Copy link
Utility of Magnesium in Anesthesia
Last updated: 05/01/2025
Key Points
- Magnesium is an essential electrolyte responsible for numerous physiological functions in the human body.
- Hypomagnesemia in the perioperative setting presents in multiple ways and should be treated for improved outcomes.
- Magnesium is versatile as a primary or secondary agent for addressing cardiovascular and neurological concerns that commonly arise throughout the perioperative course.
Introduction
- Magnesium (Mg2+) is the 4th most common cation in the body, and the 2nd most common intracellular cation in the body after potassium.1
- It acts as the cofactor of more than 300 enzymatic reactions, such as adenosine triphosphate (ATP) metabolism and nucleic acid synthesis.1,2
- Due to modern farming practices, food processing, acidic rain in the ecosystem, and the remarkable stress associated with the perioperative period, the prevalence of Mg2+ deficiency has markedly increased in surgical patients.1,3
- In addition to treating hypomagnesemia, Mg2+ has been demonstrated to furnish versatile utility in the perioperative setting for its antiarrhythmic, antihypertensive, anticonvulsant, and secondary analgesic effects.1,2,4
Physiology
Sources, Body Distribution, and Pharmacokinetics
- The recommended daily intake of Mg2+ ranges from 310 mg to 420 mg, depending on sex, pregnancy, and lactation status.5 Dietary sources of Mg2+ include various nuts, grains, seeds, legumes, cereals, and green leafy vegetables. Gastrointestinal absorption occurs primarily in the ileum and the colon.1,5
- Mg2+ supplements are available in various forms, including magnesium oxide, citrate, and chloride.5 Clinically, Mg2+ is most commonly obtained as magnesium sulfate (MgSO4). Of note, each gram of MgSO4 contains 8 mEq of Mg2+.1
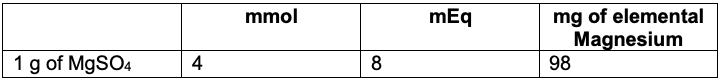
Table 1. Magnesium unit conversions
- Only 0.3% of total Mg2+ in the human body is present in the serum, 53% in the bone, 27% in the intracellular muscle compartments, and 19% in the soft tissues.1
- Normal reference range for serum Mg2+ level is 1.5 – 2.0 mg/dL (0.75 – 1.0 mmol/L).1
- According to radiolabeling studies, the half-life of Mg2+ ranges from 41 to 181 days.1
- Mg2+ is filtered and reabsorbed in the glomerulus and the ascending limb of the loop of Henle, respectively, of the kidney1. The kidney excretes about 120 mg of magnesium into the urine each day.5
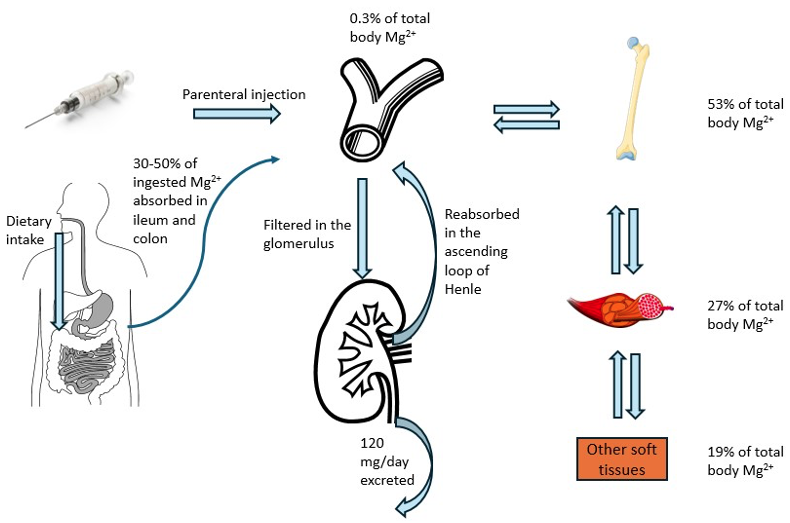
Figure 1. Homeostasis and body distribution of magnesium. Sources: Upper gastrointestinal tract, Wikimedia Commons, 2009, Accessed 03/05/2025, Link. Kidney icon, Wikimedia Commons, 2020, Accessed 03/05/2025, Link. Rheumatology femur, Wikimedia Commons, 2016, Accessed 03/05/2025, Link. Muscle fascicles and cells, Wikimedia Commons, 2016, Accessed 03/05/2025, Link. Blood vessels icon, Wikimedia Commons, 2020, Accessed 03/05/2025, Link. Injection with syringe, Wikimedia Commons, 2022, Accessed 03/05/2025, Link.
Mechanism of Action and Pharmacodynamics
- Mg2+ acts as a calcium channel competitive antagonist in the smooth muscles of arterioles, causing vasodilation with minimal venodilation. This maintains sufficient cardiac preload and output.6
- Mg2+ in the heart (12% in the mitochondria and 2-3% in the myofibrils) competitively antagonizes calcium channels and modulates cAMP-mediated pathways to downregulate sarcolemmal calcium influx into the myocyte.4
- Mg2+ levels directly regulate cAMP-mediated release of parathyroid hormone from the parathyroid gland, affecting calcium levels.7
- Mg2+ stabilizes the transmembrane gradients of sodium and potassium, affecting the sodium-potassium-ATPase system and preventing early afterdepolarization and torsade de pointes.4
- Mg2+ acts as a competitive antagonist at the calcium channels of the presynaptic nerve terminal, inhibiting acetylcholine release at the neuromuscular junction.6 This potentiates any nondepolarizing neuromuscular blockade.
- Mg2+ is a cofactor for enzymes involved in oxidative stress regulation, including antioxidative pathways by the superoxide dismutase and glutathione peroxidase systems. This facilitates membrane stability by decreasing oxidative damage to phospholipids in cell membranes due to free radical action.3
Perioperative and Anesthetic Considerations
Magnesium in Pregnancy
- Please see the OA summary on Magnesium in Pregnancy for more details. Link
Hypomagnesemia
- Magnesium deficiency has been associated with common chronic medical conditions such as hypertension, type II diabetes mellitus, alcohol-use disorder, and gastrointestinal or renal dysfunctions. It is a common electrolyte imbalance in the perioperative setting, especially in intensive care units.3
- Drugs associated with renal wasting of magnesium are amphotericin B, cisplatin, cyclosporine, digoxin, ethanol, gentamicin, loop diuretics, and pentamidine.2
- Decreased Mg2+ levels can result in hypocalcemia due to impaired parathyroid gland function.1
- As serum and urine levels of Mg2+ are unreliable detectors of magnesium, neurologic (mild tremors), neuromuscular (generalized weakness), and cardiovascular (ischemia) clinical manifestations of hypomagnesemia are essential clinical signs to monitor.2
Myocardial Protection and Antiarrhythmic Use
- Mg2+ has been demonstrated to be effective in treating various arrhythmias such as AV-nodal reentrant tachycardia, digoxin-toxicity related arrhythmias, and other supraventricular tachycardias with especially high rate of reversion to sinus when dual atrioventricular nodal pathways are present.2,4,8
- Mg2+ is particularly effective in torsade de pointes and preventing ventricular tachyarrhythmias in long QT syndromes.6,9
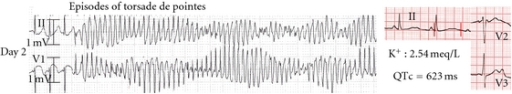
Figure 2. Electrocardiogram for Torsade de Pointes and Persistent QTc Prolongation. Source: Open-i. 2012. Accessed February 25, 2025. Link
- To stabilize the cardiac membrane, magnesium sulfate (slow 2 g intravenous [IV] push with a 1 to 4 g/hour infusion until serum levels are greater than 2 mmol/L) should be administered as soon as possible.1
- Synchronized electrical cardioversion and defibrillation should be employed for unstable and pulseless patients, respectively.1
- For patients in the intensive care units following coronary bypass surgery, Mg2+ has been demonstrated to effectively prevent atrial fibrillation and convert short-lasting but sustained atrial fibrillation. This is likely mediated by the slowing of conduction through the atrioventricular node.2,4
Hemodynamic Management of Pheochromocytoma8
- In the setting of excess catecholamines, Mg2+ works to maintain beta-adrenergic activity while antagonizing alpha-adrenergic activity.
- A single bolus dose of up to 60 mg / kg-1, repeated within 5-10 minutes if necessary, will furnish rapid control of hypertensive crises.6
- Mg2+ effectively controls the hemodynamics during the establishment of capnoperitoneum during laparoscopic removal of pheochromocytoma.6
- Combination therapy of magnesium and nicardipine for successful intraoperative management of laparoscopic adrenalectomy for pheochromocytoma has been reported.9
Neuromuscular Blockade1,6
- Mg2+ is known to potentiate nondepolarizing neuromuscular blockade by blocking presynaptic calcium channels, preventing the acetylcholine release at the neuromuscular junction.6
- Some studies have suggested the potential role of Mg2+ as a “priming agent” to facilitate a more rapid onset of nondepolarizing neuromuscular blockade with certain agents like pancuronium bromide.1
- Mg2+ is not a viable alternative to succinylcholine in rapid sequence intubation due to the prolonged recovery times after Mg2+ administration.1
Neuroprotection in the CNS and Analgesia6
- Mg2+ acts as an N-methyl-D-aspartate antagonist to protect the CNS from neurological injury.
- Mg2+ has been shown to reduce opioid consumption through oral and parenteral administration of Mg2+ through IV, intrathecal, or epidural routes, which have been shown to alleviate pain and perioperative anesthetic and analgesic requirements.1
- Magnesium does not have any known primary analgesic activity.
Other Uses
- Mg2+ has also been historically used to treat myocardial infarction.6
- Mg2+ is one of the preferred pharmacologic prevention and treatment of eclamptic convulsions.10
Safety Profile and Side Effects
- With its short-lasting, no proarrhythmic, and almost no negative inotropic effects, Mg2+ has a wide safety margin.4,6
- Mg2+ should be used with caution in patients with significant renal impairment or chronic use of oral magnesium-containing antacids due to the potential to result in hypermagnesemia.2
- Adverse effects of bolus Mg2+ injection can include flushing, bradycardia, hypotension, and PR interval prolongation without significant changes to QRS duration and QT duration4 (Figure 3). True neuromuscular toxicity and reduction of deep tendon reflexes are usually observed at significantly elevated serum levels.2
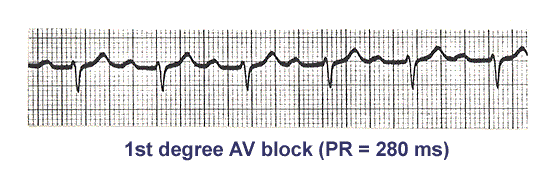
Figure 3. Electrocardiogram for PR interval prolongation. Source: Heal Collection. 2018. Accessed 25 February 2025. Link Abbreviations: AV, atrioventricular.
- Please see the OA summary on Magnesium in Pregnancy for details of clinical features at different serum magnesium levels. Link
References
- Fawcett WJ, Haxby EJ, Male DA: Magnesium: physiology and pharmacology. Br J Anaesth. 1999;83:302-20. PubMed
- McLean RM: Magnesium and its therapeutic uses: a review. Am J Med. 1994: 96:63-76. PubMed
- Parotto M, Djaiani G: Perioperative hypomagnesemia and increased postoperative morbidity and mortality: Myth or reality? J Cardiothorac Vasc Anesth. 2019: 33:480-1. PubMed
- Vester EG. Clinico-electrophysiologic effects of magnesium, especially in supraventricular tachycardia]. Herz. 1997. 22 Suppl 1:40-50. PubMed
- (ODS) NIoHNOoDS: Magnesium fact sheet for health professionals 2025. Accessed April 23 2025. Link
- James MF: Magnesium: an emerging drug in anaesthesia. Br J Anaesth. 2009:103:465-7. PubMed
- Gragossian A, Bashir K, Bhutta BS, et al. Hypomagnesemia: StatPearls. Treasure Island (FL) 2025. PubMed
- Van Braeckel P, Carlier S, Steelant PJ, et al. Perioperative management of phaeochromocytoma. Acta Anaesthesiol Belg. 2009: 60:55-66. PubMed
- Minami T, Adachi T, Fukuda K: An effective use of magnesium sulfate for intraoperative management of laparoscopic adrenalectomy for pheochromocytoma in a pediatric patient. Anesth Analg. 2002: 95:1243-4. PubMed
- Duley L, Gulmezoglu AM, Henderson-Smart DJ, et al.: Magnesium sulphate and other anticonvulsants for women with pre-eclampsia. Cochrane Database Syst Rev. 2003: (2):CD000025. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.