Copy link
Types of Pain
Last updated: 09/14/2023
Key Points
- Chronic pain is complex and exists on a continuum but can be broadly categorized as nociceptive, neuropathic, and nociplastic.
- Neuropathic pain is from nerve injury and nociceptive pain is due to tissue injury. Nociplastic pain is caused by sensitization of the nervous system.
- Pain is complex and can often have multifactorial causes requiring a holistic evaluation and approach to treat effectively.
Introduction
- The International Association for the Study of Pain (IASP) defines pain as “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.”1
- Pain often exists on a continuum but elucidating the primary etiology theoretically allows for more effective treatment rather than a symptom-based approach.2
- A broad classification for the types of chronic pain as defined by the IASP includes nociceptive pain, neuropathic pain, and/or nociplastic pain.1,3
- Neuropathic pain is defined as pain caused by damage or disease affecting the somatosensory nervous system.1,3
- Approximately 15-20% of chronic pain is neuropathic in origin and common examples include diabetic neuropathy, postherpetic neuralgia, radiculopathy, trigeminal neuralgia, etc.1
- Neuropathic pain is a clinical description (not a diagnosis) and is always a maladaptive response.3
- Nociceptive pain arises from actual or threatened damage to nonneural tissue and is due to the activation of nociceptors.
- This is the most common form of chronic pain that is expected after surgical and other traumatic injuries.1,3 Common examples include osteoarthritis, postsurgical pain, etc.
- Nociplastic pain arises from the abnormal processing of pain signals without any clear evidence of tissue damage or discrete pathology involving the somatosensory system.1,2
- Nociplastic pain can occur simultaneously with nociceptive pain. This category was previously known as functional pain syndromes. Common examples include fibromyalgia, irritable bowel syndrome, interstitial cystitis, etc.
Pathophysiology and Characteristics
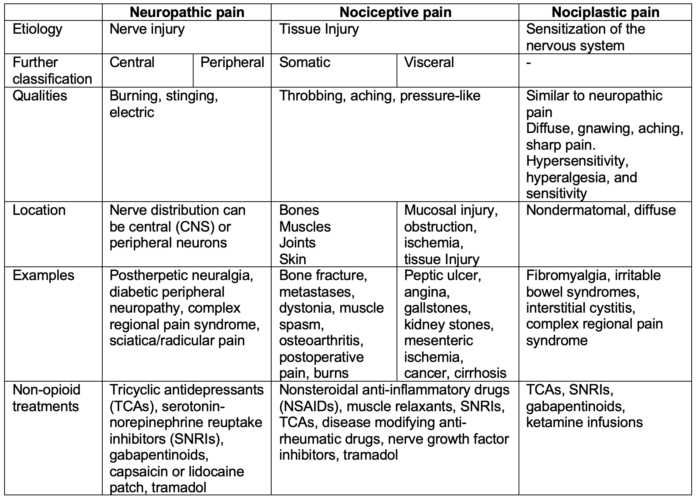
Table 1. Characteristics of the different types of chronic pain
Approach to Treatment
- Pain is often multifactorial in nature and requires a thorough evaluation and multidisciplinary approach.
- Considerations include addressing individual needs as someone from a vulnerable population or barriers to access to care.
- Treatment options range and must be evaluated on an individual basis.
- Many meta-analyses have shown mixed results to different psychological, exercise, and complementary or alternative treatments.3
- Nociceptive pain is often most responsive to anti-inflammatory medications such as NSAIDs and acetaminophen.
- A treatment algorithm proposes the following model for neuropathic pain:4
- 1st line: TCAs, SNRIs, gabapentinoids, topicals
- 2nd line: Tramadol, or combination of 1st line therapies
- 3rd line: Specialist referral and potential SSRIs/anticonvulsants, NMDA antagonists, or interventional pain therapies
- 4th line: Neuromodulation
- 5th line: Low-dose opioids
- 6th line: Targeted drug delivery
Interventional Pain Management
- Interventional therapies include numerous treatments that have the potential to reduce pain, and are often performed under fluoroscopic or ultrasound imaging guidance.
- Examples include epidural steroid injections, facet joint blocks, radiofrequency ablations, sympathetic blocks, intrathecal drug pumps, and more.
- Regional anesthesia can be a diagnostic and therapeutic step leading to further interventional procedures.
- Epidural steroid injections involve steroid and local anesthetic injections into the epidural space to provide pain relief.
- Facet joint medial branch nerve blocks and radiofrequency ablation
- Lumbar facet joint pain can be temporarily relieved with intra-articular injections or medial branch nerve blocks and later denervation of nerves can provide longer-term relief.
- Sympathetic blocks for pain syndromes and specific conditions to produce short-term reduction in pain with examples including stellate ganglion blocks, celiac plexus blocks, and lumbar sympathetic blocks.
- Intrathecal drug delivery involves an implanted programmed pump that delivers medication (typically opioids, local anesthetics, or ziconotide) into the cerebrospinal fluid.
Neuromodulation
- Neuromodulation is another therapeutic modality used to manage chronic pain.5
- Mechanistically, neuromodulation techniques promote neuroplasticity to reduce pain.
- Targets for stimulation include pathways at the brain, spinal cord, nerve root, peripheral nerves, or at transcutaneous levels.
- The quality of evidence for these techniques are mixed with low-to-moderate quality reported in meta-analyses.5
- Spinal cord stimulation
- Interferes with pain propagation with an implanted pulse generator with many applications
- Leads placed in the epidural space
- Dorsal root ganglion stimulators
- These stimulators are similar to spinal cord stimulators but target a specific dorsal root ganglion to provide more localized therapeutic specificity.
References
- International Association for the Study of Pain Terminology Working Group. Definition of pain. IASP. Publish date 1994. Updated 2022. Accessed January 23rd, 2023. Link
- Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. Lancet. 2021; 397(10289): 2082-97. PubMed
- Fitzcharles MA, Cohen SP, Clauw DJ, et al. Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet. 2021;397(10289):2098-2110. PubMed
- Bates D, Schultheis BC, Hanes MC, et al. A Comprehensive Algorithm for Management of Neuropathic Pain [published correction appears in Pain Med. 2023 Feb 1;24(2):219]. Pain Med. 2019;20(Suppl 1):S2-S12. PubMed
- Knotkova H, Hamani C, Sivanesan E, et al. Neuromodulation for chronic pain. Lancet 2021; 397(10289):2111-2124. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.