Copy link
Turner Syndrome
Last updated: 04/29/2025
Key Points
- Turner syndrome (TS) is a genetic disorder caused by the partial or complete absence of one X chromosome.
- TS affects multiple organ systems, including cardiovascular, renal, endocrine, musculoskeletal, and gastrointestinal systems.
- Anesthetic management in TS requires multidisciplinary planning due to associated comorbidities such as cardiovascular anomalies, airway challenges, and metabolic issues.
Introduction
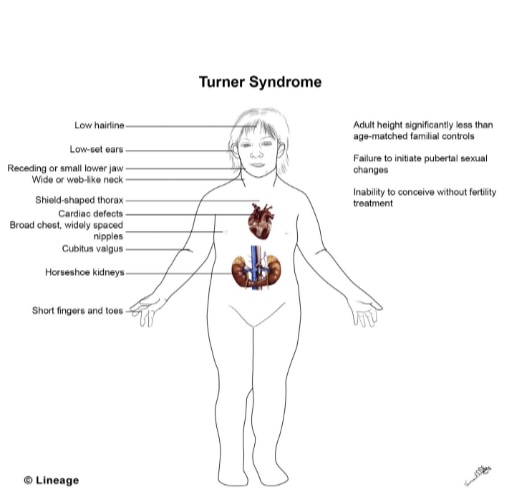
- Turner syndrome (TS) is a chromosomal disorder characterized by monosomy or structural abnormalities of the second sex chromosome, affecting approximately 3.2 per 10,000 female live births.1 The disorder presents with a spectrum of clinical manifestations, including short stature, gonadal dysgenesis, cardiovascular malformations, renal anomalies, and endocrine dysfunction.1,2
- TS is often diagnosed through clinical evaluation supported by karyotyping. Due to the multisystem involvement, anesthetic management in TS requires careful preoperative evaluation, intraoperative monitoring, and postoperative care to minimize perioperative risks.2
- The diagnosis of TS is based on clinical features and confirmed through chromosomal analysis (karyotyping). Classic signs include short stature, webbed neck, low posterior hairline, broad chest with widely spaced nipples, and lymphedema of the hands and feet in neonates.2
- Additional diagnostic work-up may include:
- Genetic testing: Karyotyping to confirm monosomy X or structural abnormalities (e.g., isochromosome, ring chromosome)2
- Imaging: Echocardiography or cardiac magnetic resonance imaging (MRI) to evaluate for congenital heart defects3
- Laboratory studies: Assessment of hormone levels to evaluate ovarian insufficiency, thyroid function tests, liver enzymes, and renal function tests3
- Prenatal diagnosis: Can be identified through noninvasive prenatal testing or amniocentesis2
Comorbidities
- TS is associated with a wide range of comorbidities affecting multiple organ systems (Figure 1).
Cardiovascular System
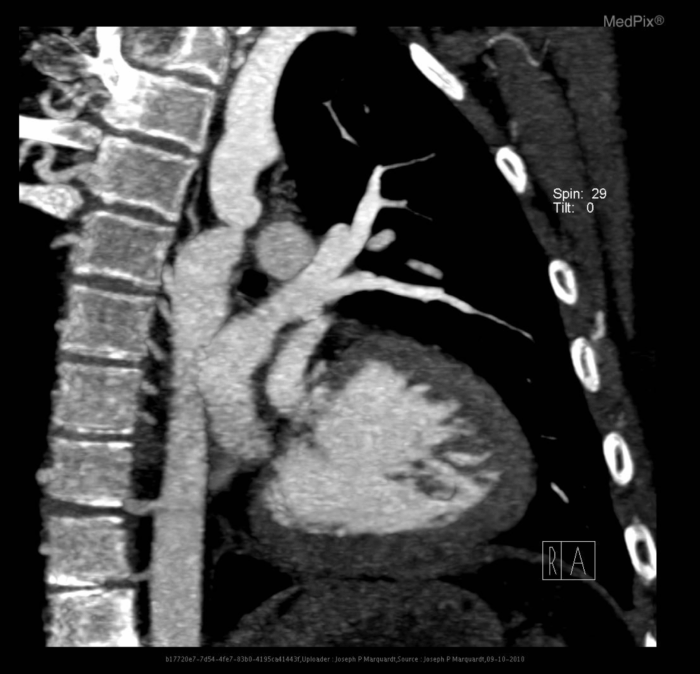
- Common anomalies: Bicuspid aortic valve, coarctation of the aorta (Figure 2), aortic dilation, and hypertension3
- Risks: Increased risk of aortic dissection, particularly during pregnancy or under hemodynamic stress3
- Management: Requires regular cardiac imaging (e.g., echocardiography, MRI) to monitor aortic size and function3
Renal Abnormalities
- Common anomalies: Patients with TS can have a horseshoe kidney, unilateral renal agenesis, duplicate collecting systems, and renal malrotation2 (Figure 3).
- Impact: Patients have an increased risk of hypertension, urinary tract infections, and impaired renal function.2
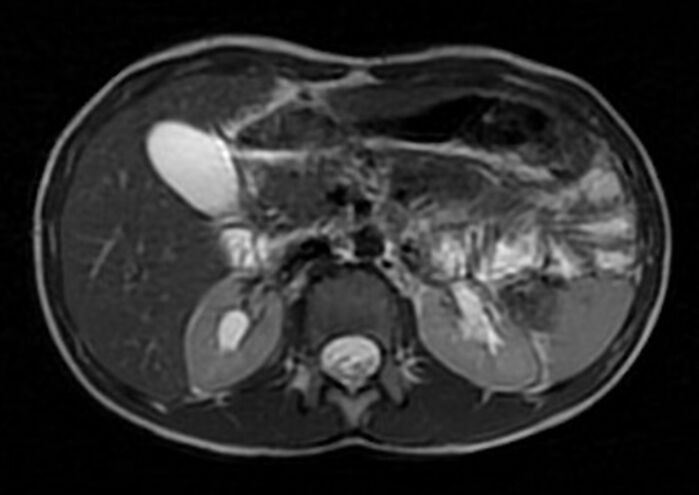
Figure 3. Horseshoe kidney: Midline fusion of lower poles of both kidneys anterior to the abdominal aorta. Anterolaterally directed bilateral extrarenal pelvis. Case courtesy of Varun Babu, Radiopaedia.org, rID:57384. Link
Endocrine and Metabolic Disorders²
- Hypothyroidism: Requires regular thyroid function monitoring
- Diabetes mellitus type 1 & 2, and insulin resistance: Increased risk due to metabolic syndrome
- Osteoporosis: Resulting from estrogen deficiency, leading to increased fracture risk
Gastrointestinal Conditions²
- Conditions: Malrotation, celiac disease, inflammatory bowel disease, nonalcoholic fatty liver disease, and gallstones
- Impact: Risk of liver dysfunction affecting drug metabolism during anesthesia
Ear, Nose, Throat and Airway Concerns²
- Common issues: Recurrent otitis media, conductive and sensorineural hearing loss, high-arched palate, micrognathia, and webbed neck
- Risks: Difficult airway management due to craniofacial abnormalities

Figure 4. Teenaged girl with Turner syndrome and webbed neck. By Imen Mehri Turki - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5340086/, CC BY 4.0, Link
Musculoskeletal Abnormalities2
- Scoliosis and kyphosis: May contribute to restrictive lung disease and affect positioning
- Klippel-Feil anomaly: Cervical vertebral fusion causing limited neck mobility, impacting airway management and neuraxial anesthesia
- Short stature and skeletal dysplasia: Affects drug dosing, airway alignment, and positioning during surgery
- Joint hypermobility and osteoporosis: Increased risk of fractures and joint dislocations

Figure 5: Fusion of multiple cervical vertebrae, namely C2 with C3, C4 with C5, and C6 with C7 vertebrae. Case courtesy of Bassem Marghany, radiopaedia.org, rID:75116. Link
Perioperative Management
- A comprehensive perioperative plan is essential to minimize complications in patients with Turner syndrome, given their multisystem involvement.2
Preoperative Considerations
Cardiovascular Evaluation3
- Perform an echocardiogram or cardiac MRI to assess aortic root dilation, valve abnormalities, and other congenital defects
- Maintain blood pressure near baseline to reduce the risk of aortic dissection
- Cardiology consultation for patients with significant cardiac pathology
Airway and Pulmonary Evaluation2
- Assess for difficult airway due to craniofacial anomalies (e.g., high-arched palate, micrognathia, webbed neck)
- Consider airway imaging or preoperative airway exam in severe cases
- Pulmonary function tests (PFTs) if scoliosis or kyphosis is present
- Evaluate history of recurrent respiratory infections or obstructive symptoms
Renal and Endocrine Evaluation2
- Renal function tests (creatinine, electrolytes, urinalysis) to screen for congenital anomalies and UTIs
- Consider thyroid function tests if there is a history of hypothyroidism
- Blood glucose monitoring due to increased risk of insulin resistance and diabetes
Musculoskeletal and Neuraxial Considerations2
- Spinal deformities (scoliosis, kyphosis): Assess for restrictive lung disease (PFTs) and potential difficulty with neuraxial anesthesia
- Cervical spine abnormalities (e.g., Klippel-Feil syndrome): Evaluate neck mobility and consider imaging if instability is suspected
- Osteoporosis and joint hypermobility: Use careful handling to prevent fractures or joint dislocations
Intraoperative Considerations
Airway Management
- Prepare for difficult intubation; video laryngoscopy or fiberoptic bronchoscopy may be required.2
- Review past airway records, consider awake fiberoptic intubation with multiple alternative plans, including a surgical airway
- Pay attention to the position of the endotracheal tube intraoperatively, given the short neck and risk of endobronchial intubation4
Cardiovascular Monitoring and Hemodynamics
- Consider arterial line for tight blood pressure (BP) control if significant cardiovascular anomalies such as aortic stenosis, coarctation, or aortic root dilation are present3,4
- Avoid rapid BP fluctuations to reduce the risk of aortic dissection3
Ventilation and Pulmonary Strategies2
- Adjust ventilation for restrictive lung physiology
- Use lung-protective strategies with positive end-expiratory pressure to prevent atelectasis while avoiding baro- or volutrauma
Renal Protection and Drug Metabolism2
- Avoid nephrotoxic drugs (e.g., nonsteroidal anti-inflammatory drugs(NSAIDs)) and follow renal dosing guidelines
- Maintain adequate hydration to preserve renal perfusion
- Adjust anesthetic drug dosing based on renal and hepatic function
Musculoskeletal Considerations and Positioning
- Positioning challenges: Scoliosis, osteoporosis, and joint hypermobility require proper padding and gentle manipulation to prevent nerve injury, dislocation, or fractures.2
Neuraxial Anesthesia Considerations2
- Technical challenges: Spinal deformities may complicate neuraxial anesthesia—ultrasound guidance can improve success rates.
- Spinal cord risk: Cervical spine abnormalities may be associated with spinal cord malformations—consider preoperative imaging if neuraxial blockade is planned.
- Dose Adjustments: Short stature may require lower doses of local anesthetics to prevent high spinal blockade.
Postoperative Considerations
Airway and Respiratory Care2
- Monitor for airway obstruction due to residual anesthesia effects and craniofacial abnormalities
- Encourage incentive spirometry to reduce the risk of atelectasis
Cardiovascular Monitoring3
- Continue BP monitoring, particularly in hypertensive patients
- Watch for aortic dissection in patients with known dilation
Renal and Fluid Management2
- Monitor urine output closely
- Reassess renal function postoperatively if significant fluid shifts or hypotension have occurred
Pain Management2
- Avoid NSAIDs in patients with renal impairment
- Use multimodal analgesia, including regional anesthesia, when appropriate
Endocrine and Metabolic Monitoring2
- Monitor blood glucose in diabetic or insulin-resistant patients
- Assess thyroid function if hypothyroidism is poorly controlled
References
- Yoon SH, Kim GY, Choi GT, et al. Organ abnormalities caused by Turner syndrome. Cells. 2023;12(10):1365. PubMed
- Martin-Giacalone BA, Lin AE, Rasmussen SA, et al. Prevalence and descriptive epidemiology of Turner syndrome in the United States, 2000–2017. Am J Med Genet A. 2023;191(5):1339-49. PubMed
- Dulac Y, Pienkowski C, Abadir S, Tauber M, Acar P. Cardiovascular abnormalities in Turner’s syndrome: what prevention? Arch Cardiovasc Dis. 2008;101(7-8):485-90. PubMed
- Mashour GA, Sunder N, Acquadro MA. Anesthetic management of Turner syndrome: a systematic approach. J Clin Anesth. 2005;17(2):128-30. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.