Copy link
Total Anomalous Pulmonary Venous Return
Last updated: 08/08/2023
Key Points
- Total anomalous pulmonary venous return (TAPVR) is one of the few remaining pediatric cardiac surgical emergencies.
- There are four types of TAPVR that are classified by the anatomy of the defect.
- The degree of pulmonary venous obstruction dictates patient presentation.
Introduction
- TAPVR is uncommon with an incidence of 7 per 100,000 live births and accounting for less than 3% of congenital anomalies.1,2 It is the fifth most common cause of cyanotic congenital heart disease.3
- TAPVR consists of a spectrum of disease in which the pulmonary veins (PV) fail to form a connection to the left atrium (LA). Pulmonary venous blood returns to the systemic venous circulation via systemic veins or by a direct connection to the right atrium.
- TAPVR is classified based on the location of the anomalous venous return:
- Type I – Supracardiac (45%): This is the most common type of TAPVR. PVs drain to a confluence behind the LA and a connection is formed to the innominate vein or directly to the right superior vena cava via a vertical vein. Pulmonary venous obstruction is present in ~50% of cases and occurs at two common locations: 1. the insertion of the vertical vein to the innominate vein, and 2. between the tracheal bronchus and left pulmonary artery.1,2 As obstruction worsens, the pulmonary artery pressure rises, increasing dilation and creating a “hemodynamic” vice.3
- Type II – Cardiac (~25%): The pulmonary venous confluence connects to the coronary sinus or directly to the right atrium. Pulmonary venous flow is typically unobstructed and clinical features are that of a large atrial septal defect (ASD).2
- Type III – Infracardiac (~25%): The pulmonary venous confluence drains to either the portal vein, ductus venosus, hepatic vein, or the inferior vena cava via a vertical vein that traverses the diaphragm. Due to the greater distance travelled by the vertical vein, there is a higher incidence of pulmonary venous obstruction in this subset.2,3
- Type IV – Mixed (~5%): The remaining patients will have a combination of the above types 1, 2, or 3, at two or more levels.
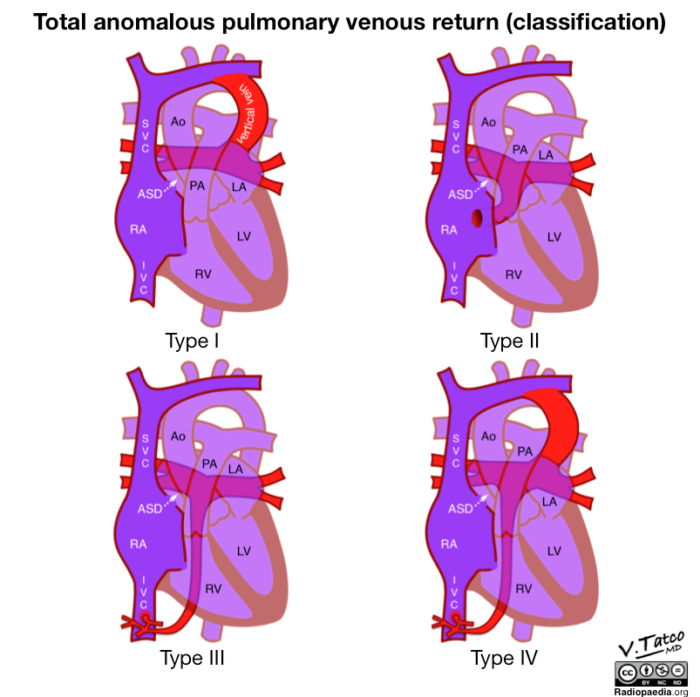
Figure 1. Classification of total anomalous pulmonary venous return. Image courtesy of Vincent Tatco, radiopedia.org, rID: 51911. Link.
Etiology
Embryology
- During normal development, venous drainage from the lung bud is to the vascular plexus of the foregut (splanchnic plexus). There is no connection to the heart. Eventually a primitive connection will form to the dorsal side of the LA as the common pulmonary vein projects out and connects to the pulmonary venous complex. As the common pulmonary vein further incorporates into the LA, the connections between the primitive pulmonary venous plexus and the systemic veins involute.
- TAPVR occurs when there is atresia of the common pulmonary vein or failure of the common pulmonary vein to connect to the LA.
Epigenetic Factors
- There are no known environmental factors.
Genetic Factors
- TAPVR most often occurs without a family history of congenital heart disease and has a low recurrence rate. However, several genetic abnormalities have been isolated in patients with TAPVR.
- There are case reports of familial association with segregation to an autosomal dominant inheritance pattern.4 TAPVR has also been reported in single-gene disorders such as Holt-Oram, Noonan syndrome, etc.2,4
Pathophysiology
- All pulmonary venous blood returns to the right side of the heart resulting in a large left-to-right shunt. There is complete mixing of pulmonary venous and systemic venous blood.
- A right-to-left shunt (ASD, patent foramen ovale, and/or patent ductus arteriosus) is necessary for survival in the neonatal period.
- All TAPVR is assumed to have some degree of obstruction, with the clinical presentation depending on the degree of pulmonary vein obstruction (PVO) and the presence or absence of a nonrestrictive atrial communication.
- The presence of PVO can lead to elevated pulmonary vascular resistance (PVR), and the subsequent development of pulmonary hypertension in utero.
Associated Anomalies
- TAPVR is associated with other cardiac anomalies (e.g., complete atrioventricular canal defect, single ventricle lesions, transposition of the great arteries, and/or PDA) in ~30% of patients. Abnormalities of atrial and visceral situs are also common. This is especially true for heterotaxy with right-sided isomerism.1,4
Diagnosis
Presentation
- Prenatal diagnosis: TAPVR has the lowest prenatal detection rate of any critical cardiac disease. Screening ultrasonography only detects 2-10% of cases.2
- Postnatal diagnosis:
- Without PV obstruction: Patients will have minimal symptoms at birth but will develop cyanosis (due to intracardiac mixing) and pulmonary overcirculation (due to increased left-to-right shunting) with signs of heart failure as the PVR falls.
- With PV obstruction: Patients will present in extremis immediately after birth with pulmonary edema, severe and progressive cyanosis, metabolic acidosis, and/or cardiogenic shock. Neonates with hypoxemic respiratory failure are often treated for persistent pulmonary hypertension of the newborn prior to the diagnosis of TAPVR.
Diagnostic Studies
- Chest radiography (CXR): Findings depend on the degree of PVO. CXR may show either pulmonary overcirculation (no PVO) or severe pulmonary edema without cardiomegaly (with PVO). A classic image seen in older patients with supracardiac TAPVR is the “snowman sign,” in which the “head” of the snowman is formed by the dilated venous structures.
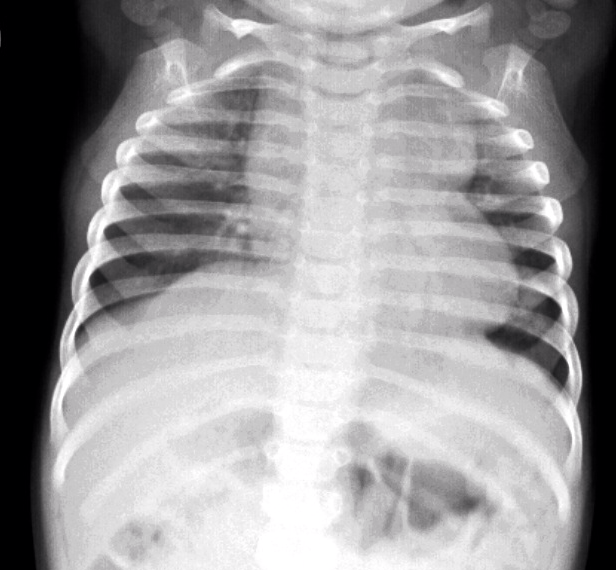
Figure 2. Chest radiograph of a patient with supracardiac TAPVR demonstrating the classic “snowman sign.” Source: Case courtesy of Aditya Shetty, Radiopaedia.org, rID: 27800. Link.
- Echocardiography is extremely important for the diagnosis of TAPVR and is essential for locating the PVs and their course, determining the presence of obstruction, and evaluating RV pressures, and the size of left-sided structures. Shunting at the atrial level is exclusively right-to-left. Associated intracardiac disease should also be ruled out.
- Electrocardiogram (ECG) will show right-axis deviation with right atrial dilation and RV hypertrophy.
- Computed tomography angiography (CTA) and/or cardiac catheterization can be performed if echocardiography is not sufficient for surgical planning and the patient is stable enough to tolerate these studies.2,6
Treatment Strategies
- Medical Management – Initial management typically includes intubation, mechanical ventilation, and hemodynamic support with inotropic medications. Caution is advised when pulmonary vasodilators such inhaled nitric oxide (iNO) are used to manage pulmonary artery hypertension as they may worsen pulmonary edema in the setting of fixed PVO.3,6
- Interventional Management – Temporary stabilization with extracorporeal membrane oxygenation (ECMO) support may be necessary prior to surgical intervention. There are rare cases in which the patient is not a surgical candidate and may require an intervention such as stenting of the common PV to relieve obstruction prior to surgical management.2
- Surgical Management – Definitive therapy involves reconnection of the pulmonary venous confluence to the posterior aspect of the LA and closure of any right to left shunts.
Anesthetic Considerations for Interventional/Surgical Management
Preoperative
Labs
- Complete blood count
- Basic metabolic profile
- Arterial blood gas
- Type and crossmatch
Imaging/Diagnostics
- A ECG should be performed and possibly a CTA.
- A CXR should be obtained to assess for the presence/severity of pulmonary edema and the appropriate placement of invasive umbilical lines. Umbilical venous lines should be left low-lying to avoid obstruction of the ductus venosus and worsening of infracardiac PVO.
- Head ultrasound may be needed to rule out intraventricular hemorrhage before heparinization.
Intraoperative
Monitoring
- Standard American Society of Anesthesiologists monitors
- Near-infrared spectroscopy
- Invasive pressure monitoring – central venous pressure, arterial pressure
- Intraoperative TEE is typically avoided due to risk of compression of the pulmonary venous confluence, which tends to be immediately anterior to the esophagus.1,6
- Intracardiac lines – typically, a LA line will be left by the surgeon for monitoring of left-sided filling pressures in the postoperative period.
Access
- Two large-bore peripheral intravenous (IV) catheters
- Central line (may be umbilical or intracardiac)
Anesthesia Technique
- General endotracheal anesthesia
Hemodynamic Goals
- Precardiopulmonary bypass (CPB):
- Patients with TAPVR and PVO have compromised end-organ perfusion. Cardiac output is optimized by maintaining an age-appropriate heart rate along with supporting contractility and ensuring adequate preload.
- Increases in PVR should be avoided.
- Ventilation is titrated to maximize PaO2.
- Post-CPB:
- Reactive PVR and/or pulmonary hypertension should be anticipated. Care should be taken to avoid further increases in PVR and consideration given to empiric iNO.
- Left atrial hypertension may be encountered due to a small, noncompliant LA and ventricle. Careful volume administration is best guided by using a LA pressure line.3.6
- Inotropic support with dopamine, epinephrine, and/or milrinone may be required to support the RV and maintain systemic perfusion.
- Pacing may be required to support heart rate.
- Poor lung compliance should be anticipated.
Postoperative
- Bleeding, pulmonary hypertension, atrial tachyarrhythmias, and low cardiac output syndromes are the most commonly encountered postoperative complications encountered in the immediate postoperative period.
- Long-term complications include anastomotic obstruction and pulmonary vein stenosis.
References
- Ross FJ, Joffe D, Latham GJ. Perioperative and anesthetic considerations in total anomalous pulmonary venous connection. Semin Cardiothorac Vasc Anesth. 2016; 21(2):138–44. PubMed
- Files MD, Morray B. Total anomalous pulmonary venous connection: Preoperative Anatomy, physiology, imaging, and interventional management of postoperative pulmonary venous obstruction. Semin Cardiothorac Vasc Anesth. 2016; 21(2): 123–31. PubMed
- Nasr VG, DiNardo JA. Total anomalous pulmonary venous return. In: The Pediatric Cardiac Anesthesia Handbook. John Wiley & Sons Ltd; 2017:107-111.
- Kim HS, Jeong K, Cho HJ, et al. Total anomalous pulmonary venous return in siblings. J Cardiovasc Ultrasound. 2014 Dec;22(4):213-9. PubMed
- Berenstain LK, Spaeth J. Total anomalous pulmonary venous return and heterotaxy syndrome. In: Congenital Cardiac Anesthesia: A Case-Based Approach. Cambridge University Press; 2021:169-177.
- Mery CM, Penny DJ. Chapter 10 Pulmonary Venous Anomalies. In: Texas Children's Hospital Handbook of Congenital Heart Disease. Houston, TX: Texas Children's Hospital; 2020:56-70.
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.