Copy link
Topical Hemostatic Agents
Last updated: 05/22/2025
Key Points
- Intraoperative hemostasis is generally achieved by electrosurgical coagulation, suture ligation, or suture repair of blood vessels. The use of topical hemostatic agents may assist hemostasis in certain circumstances.1
- Topical hemostatic agents are substances that can be applied to wounds to control bleeding. They can be used in place of or in addition to sutures or electrocautery.
- Most anesthetic agents can slightly impair platelet aggregation, making it harder for platelets to clump together and form clots, which is the primary mechanism of hemostasis.
Introduction
- Uncontrolled exsanguination remains the leading cause of death for trauma patients, many of whom die in the prehospital setting. Without expedient intervention, trauma-associated hemorrhage induces a host of systemic responses and acute coagulopathy of trauma. For this reason, healthcare providers and prehospital personnel face the challenge of swift and effective hemorrhage control.2
- Hemostasis is critical in achieving a positive outcome in any surgical intervention. Severe hemorrhage causes significant metabolic and cellular dysfunction secondary to deficient tissue perfusion and oxygen delivery. If bleeding continues, hemodynamic destabilization, hypoxemia, multiple organ failure, and death will occur.3,4
- Different hemostatic methods can be employed, and topical hemostatic agents are used in various surgical settings. They may be particularly useful when suturing and electrocautery are ineffective or potentially hazardous. Procoagulation agents have different hemostatic properties, and the choice of a specific one is determined by the type of surgical procedure and bleeding.1,3
- Topical hemostatic agents promote platelet activation and aggregation when directly applied to the bleeding tissue, and they can absorb body fluids several times their weight.3
- To achieve successful hemostasis, several vital factors must be considered by surgeons and perioperative nurses, such as the size of the wound, bleeding severity and efficacy, possible adverse effects, and method of application of potential hemostatic agents.5
Categories
- Topical hemostatic agents—including mechanical hemostats, active hemostats, flowable hemostats, and fibrin sealants—are frequently used in efforts to control bleeding, and new options such as hemostatic dressings, initially used in combat situations, are increasingly being used in civilian settings.5
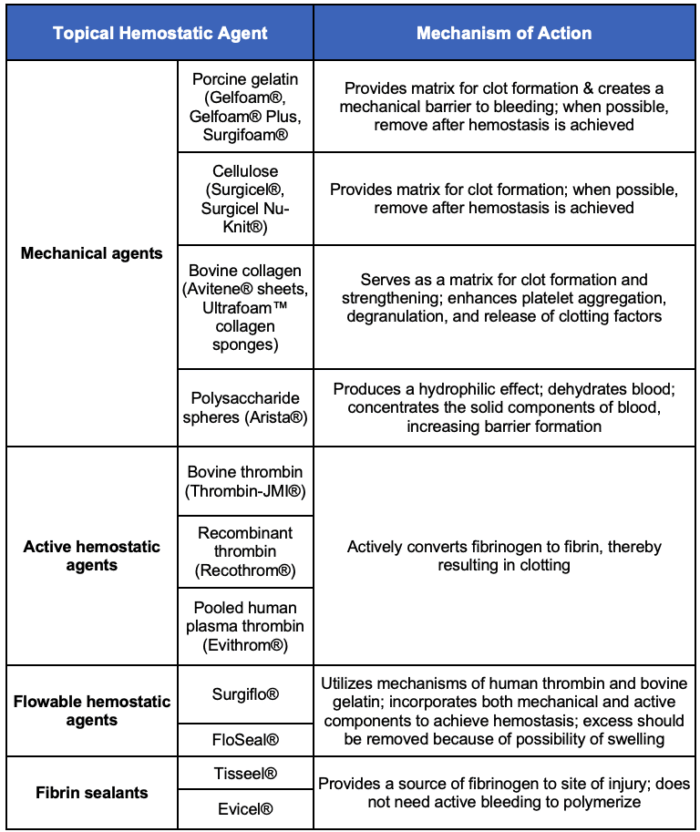
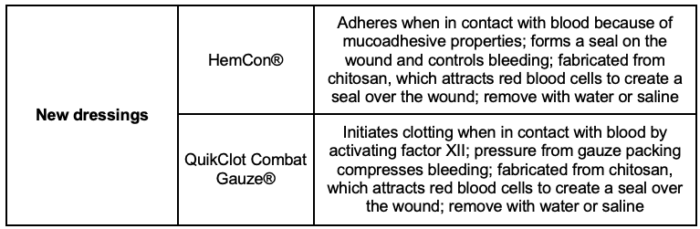
Table 1. Categories of topical hemostatic agents5
Clinical Uses
- The ideal hemostatic agent balances efficacy with safety, practicality, and cost-effectiveness. Selection should be tailored to each patient’s injury pattern and physiologic state. Their utilization is often limited to treating accessible locations in the body. Topical active agents contain fibrinogen and/or thrombin and fibrin, which actively trigger the coagulation cascade and fibrin clot formation; thus, they are suitable for congenital or acquired bleeding disorders and coagulation abnormalities.2,4
- Topical hemostatic agents are most commonly used in situations where the use of electrocautery or sutures for hemostatic control of surgical bleeding is not ideal or safe, including bleeding in areas with nearby vulnerable structures or in the presence of diffuse bleeding from peritoneal surfaces or cut surfaces of solid organs.6
- Mechanical hemostats rely on fibrin production to achieve hemostasis; therefore, these agents are only appropriate for patients with an intact coagulation cascade. Patients with hemorrhage secondary to a significant coagulopathy, for example, would not be suitable candidates for this type of hemostatic treatment.5
- Topical thrombins that stimulate fibrinogen at the bleeding site to produce a fibrin clot are known as active hemostats. These agents can be used effectively in patients with coagulation systems that are impaired as a result of heparinization, mild coagulopathy, or other conditions.5
- Composed of either a porcine or bovine gelatin matrix plus thrombin, flowable hemostatic agents are another essential tool for perioperative nurses because they provide both a mechanical and an active hemostat in a single application to effectively control bleeding.5
- Fibrin sealants are absorbable dressings containing fibrinogen and thrombin that can be applied to raw surfaces anywhere in the body cavity to create a watertight occlusive effect. Fibrin sealants achieve hemostasis by providing higher concentrations of fibrinogen and thrombin at the bleeding site, thus increasing clot formation.5
- Hemostatic dressings are a relatively new hemostatic option that was initially used in combat situations and is increasingly being used in civilian settings. Although the use of these dressings outside the combat setting currently is likely limited to large trauma centers, their use in the prehospital setting is increasing.5
General Indications
- Topical hemostatic agents are primarily used for diffuse bleeding from:7
- Peritoneal or pleural surfaces
- Cut surfaces of solid organs
- Cut edges of bone
- Bleeding near nerves
- Bleeding near vital structures at risk for cautery-induced injury
- Bleeding from vascular structures or grafts due to suture holes
- Nasal structures as nasal packing
- Dental extraction sites.
- Topical hemostatic agents can also be used for other purposes, including the management of:7
- Air leak following lung resection
- Eardrum perforation
- Endoscopic control of gastrointestinal bleeding
- Leakage prevention from colonic anastomoses following the reversal of temporary colostomies
General Contraindications
- Topical hemostatic agents should not be used intravascularly because they will cause thrombosis. Also, they should not be used in confined spaces where expansion of the product could lead to compression.7
- Caution should be exercised when using porcine-based topical hemostatic agents (e.g., Gelfoam®, Gelfoam® Plus, Surgifoam®), as their pig-derived components may conflict with certain religious beliefs.
- Jehovah’s Witnesses forbid transfusions of whole blood and its four main components–red cells, white cells, platelets, and plasma. However, they consider blood fractions (e.g., albumin, clotting factor concentrates) a personal choice, to be decided by the individual; therefore, they do not prohibit the use of topical hemostatic agents, even if they are porcine-derived, since they are not considered “blood” or primary blood components.
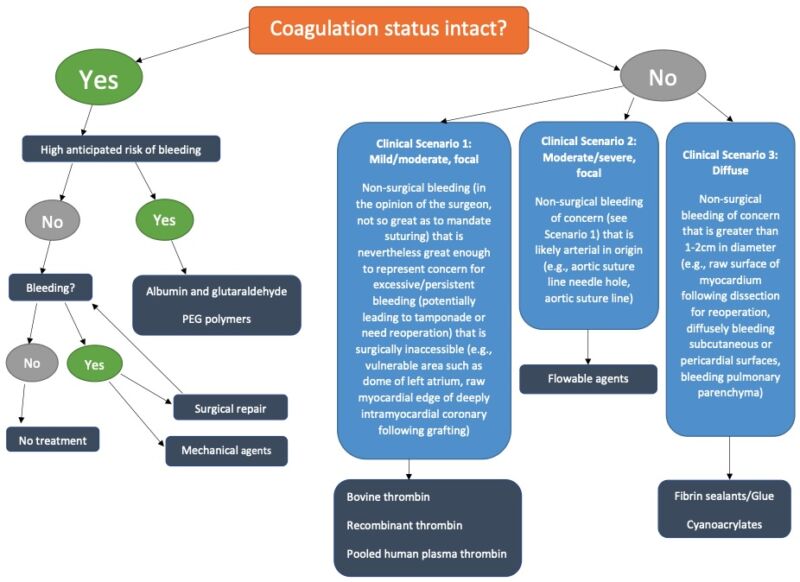
Figure 1. Topical hemostatic agent selection flowchart. Adapted from Art B, et al. The use of topical hemostatic agents in cardiothoracic surgery. Ann Thorac Surg. 2017;104(1): 353 – 60.8
Complications
- Topical hemostatic agents with bovine or porcine ingredients carry the risk of causing intraoperative or postoperative anaphylactic reactions in some patients.9
- Fibrin sealants lacking aprotinin and fibrin stabilizing factor XIII would not bind firmly to ePTFE grafts.9
- BioGlue has been found to result in several complications, including vena cava stenosis and coronary embolism.9
- When used during surgery, topical hemostatic agents can potentially affect anesthesia via their vasoconstrictive actions. They can constrict blood vessels and influence blood pressure, which can indirectly impact the anesthetic requirements and potentially reduce the need for higher doses of anesthetic because of decreased bleeding.
- Ultimately, anesthesia can potentially impair the effectiveness of topical hemostatic agents by impacting platelet function, primarily through the inhibition of platelet aggregation, which is crucial for clot formation; certain anesthetic agents like halothane are known to have a more pronounced effect on platelet function, potentially leading to increased bleeding during surgery.
References
- Brown KGM, Solomon MJ. Topical haemostatic agents in surgery. Br J Surg. 2024;111(1): znad361. PubMed
- Tompeck AJ, Gajdhar AUR, Dowling M, et al. A comprehensive review of topical hemostatic agents: The good, the bad, and the novel. J Trauma Acute Care Surg. 2020; 88(1): e1-e21. PubMed
- Emilia M, Luca S, Francesca B, et al. Topical hemostatic agents in surgical practice. Transfus Apher Sci. 2011; 45 (3): 305-11. PubMed
- Huang L, Liu GL, Kaye AD. et al. Advances in topical hemostatic agent therapies: A comprehensive update. Adv Ther. 2020; 37: 4132-48. PubMed
- Schreiber MA, Neveleff DJ. Achieving hemostasis with topical hemostats: making clinically and economically appropriate decisions in the surgical and trauma settings. AORN J. 2011; 94 (5):S1-S20. PubMed
- American College of Obstetricians and Gynecologists’ Committee on Gynecologic Practice. Topical hemostatic agents at time of obstetric and gynecologic surgery: ACOG Committee Opinion, Number 812. Obstet Gynecol. 2020;136(4): e81-e89. PubMed
- Peralta, E. Overview of topical hemostatic agents and tissue adhesives. In: Post T(ed). UpToDate. Dec 2023. Link
- Art B, Shander A, Aronson S, et al. The use of topical hemostatic agents in cardiothoracic surgery. Ann Thorac Surg. 2017;104(1): 353 - 360. PubMed
- Allotey JK, King AH, Kumins NH, et al. Systematic review of hemostatic agents used in vascular surgery. J Vasc Surg. 2021;73(6):2189-97. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.