Copy link
Sustainable Healthcare: An Overview
Last updated: 04/30/2024
Key Points
- The daily use of volatile agents generates up to 50% of the operating room's (OR) overall greenhouse gas emissions. This is more than the combined emissions from surgical materials waste, lighting, and temperature management.
- Nitrous oxide and desflurane are high-impact volatile agents that contribute significantly more to global warming potential than any other volatile agent.
- Total intravenous anesthesia (TIVA) can be beneficial, provided that medications are judiciously utilized and disposed of appropriately.
- Up to 20-50% of unused anesthesia-related medications are discarded, contributing to pharmaceutical waste. Considerations in sustainable healthcare should include using low-flow gases, appropriate utilization of TIVA, and recycling when possible.
Environmental Impact of Anesthetics
Impact
- Sustainable healthcare is a topic of paramount importance as the everyday implications of the field of anesthesiology can contribute to ongoing waste and increased greenhouse gas emissions.
The daily use of volatile agents in the OR can generate up to 50% of the overall greenhouse gas emissions. This is more than the combined emissions from surgical materials waste, lighting, and temperature management combined.1 - Volatile anesthetic agents are potent greenhouse gases that remain in the atmosphere to retain heat from solar radiation, contributing to global warming.2
Volatile Agents and Global Warming
- Global warming potential (GWP) compares the global warming contribution of a volatile agent to that of an identical mass of CO2 over a specific period of time.
- The higher the GWP value, the larger its warming impact over a designated period of time.2 Desflurane has the highest 100-year global warming potential (GWP100) of the volatile agents used in modern practice today.
- In addition to GWP values, the length of time greenhouse gases remain in the atmosphere to exert their impact is also significant.2 Nitrous oxide has the longest atmospheric lifetime of all modern volatile agents.

Table 1. 100-year Global Warming Potential of Volatile Agent. Adapted from American Society of Anesthesiologists, The Environmental Impact of Inhaled Anesthetics. MAC = minimum alveolar concentration. The GWP of CO2 is 1 for reference. Link
Reducing Volatile Agent Waste
- In January 2024, the American Society of Anesthesiologists (ASA) issued an updated Anesthesiology Sustainability Checklist, which included the following recommendations to reduce volatile agent waste in the OR (Table 2).
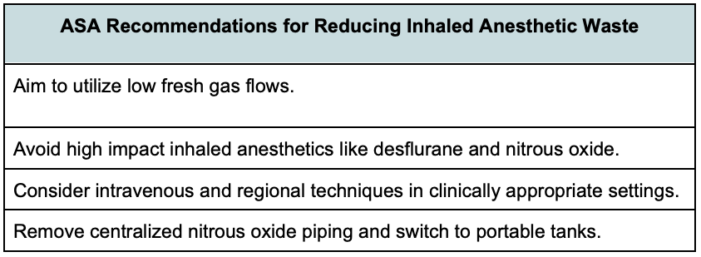
Table 2. ASA recommendations for reducing inhaled anesthetic waste. Adapted from ASA Sustainability Checklists. Link
Considerations for Reducing Inhaled Anesthetic Waste
Absorbent Choices in Low Flow Anesthesia
- Historically, CO2 absorbents consisted of calcium hydroxide (CaOH) and strong bases like sodium and potassium hydroxide that enhanced the absorptive capacity of CaOH.3 These strong bases can produce compound A in the setting of sevoflurane utilization and carbon monoxide (CO) in the setting of desiccation.
- Modern potassium hydroxide-free absorbents containing less than 2% sodium hydroxide produce minimal amounts of compound A when utilized with sevoflurane.4
- Moreover, modern absorbents that are free of KOH or NaOH do not produce carbon monoxide, regardless of the desiccation state.3
Sevoflurane in Low-Flow Anesthesia
- Based on animal studies, the Food and Drug Administration recommends against the use of sevoflurane with fresh gas flow (FGF) less than 2 L/min. Due to the lack of evidence for human harm attributed to low-flow sevoflurane utilization and compound A, the ASA has supported low fresh gas flow practices with sevoflurane.5
- In 2023, the ASA published a statement on the safety of sevoflurane with low-flow anesthesia, below the lower limits of 2L/min as stated in the FDA sevoflurane insert:5 Link
Low-Flow Inhalational Induction
- An inhalational induction aims to deliver the anesthetic to allow for a rapid increase in end-tidal volatile concentration. To accomplish this, the fresh gas flow should equal minute ventilation to minimize rebreathing of exhaled gases, which can dilute the desired concentration of the inhaled anesthetic.
- If the mask seal is adequate, gas flow greater than minute ventilation results in excessive waste without an increase in induction speed. Fresh gas flow may need to exceed minute ventilation if there is a mask leak.
- For pediatric patients, minute ventilation (VE) can be approximated as 150 mL x weight (kg) or VE~120 mL/kg estimate based on VCO2 from Brody’s equation6.
- The Society for Pediatric Anesthesia (SPA) has published a one-pager for weight-based FGF utilization during inhalational induction: Link.
- Per the 2024 ASA statement on Fresh Gas Flow Management, overpressurization of the circuit can be employed during low-flow inductions to achieve similar circuit concentrations of volatile anesthetic as higher-flow inductions. Providers should monitor the rise in end-tidal volatile concentration to avoid overdosing.
Nitrous Oxide Avoidance and Removal from Central Supply
- Nitrous oxide is an ozone-depleting greenhouse gas with the longest atmospheric lifetime of all commonly used inhaled agents.
- Between 75 and 95% of nitrous oxide is wasted prior to reaching the patient via leaks through central piping manifolds.7
- The ASA recommends replacing the central nitrous oxide supply with portable e-cylinder tanks in the ORs for direct use. Link
Pharmacologic Waste
- ORs can contribute up to 70% of the total waste in hospital systems. The major source of this waste is due to incorrectly sorted recyclables and disposal of open but unused supplies.8
- Anesthesia-related waste is categorized into regulated medical waste, requiring special processing, and solid waste, which does not require special processing.
- Anesthesia-related medications can contribute up to 10–13% of a hospital’s total pharmaceuticals budget. Studies and audits demonstrate that approximately 20–50% of anesthesia-related medications are wasted or discarded.9
- Preventable pharmaceutical waste was most frequently ephedrine, succinylcholine, propofol, and lidocaine.9-10
References
- MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health. 2017;1(9):e381-e388. PubMed
- Ryan SM, Nielsen CJ. Global warming potential of inhaled anesthetics. Anesth Analg. 2010;111(1):92-8. PubMed
- Branche R, Feldman J, Hendrick J. Low flow and CO2 absorbents. APSF Newsletter. 2017;32(2). Link
- Kobayashi S, Bito H, Morita K, et al. Amsorb Plus and Drägersorb Free, two new-generation carbon dioxide absorbents that produce a low compound A concentration while providing sufficient CO2 absorption capacity in simulated sevoflurane anesthesia. J Anesth. 2004;18(4):277-81. PubMed
- ASA Committee on Environmental sustainability: Greening the operating room Link
- Glenski T, Narayanasamy S. Low flow anesthesia in pediatric patients. Society for Pediatric Anesthesia. Accessed Jul 2, 2023. Link
- Sherman JD. It's time hospitals abandon nitrous oxide pipes. ASA Monitor 2024; 88:33 Link
- Braschi C, Tung C, Chen KT. The impact of waste reduction in general surgery operating rooms. Am J Surg. 2022 Dec;224(6):1370-3. PubMed
- Rinehardt EK, Sivarajan M. Costs and wastes in anesthesia care. Curr Opin Anaesthesiol. 2012; 25 (2): 221-5. PubMed
- Atcheson CL, Spivack J, Williams R, Bryson EO. Preventable drug waste among anesthesia providers: opportunities for efficiency. J Clin Anesth. 2016; 30:24-32. PubMed
Other References
- Anesthesia Patient Safety Foundation. Low Flow Anesthesia course. Accessed April 30, 2024. Link
- Anesthesia Patient Safety Foundation. Episode #110 How Low Can You Go? Keeping Patients Safe During Low-Flow Anesthesia Care. Published August 9, 2022. Accessed April 30, 2024. Link
- Betchtel A. Anesthesia Patient Safety Foundation. Episode #102 The Next Patient Safety Movement: Sustainable Health Care. Published 2022. Accessed April 30, 2024. Link
- Betchtel A. Anesthesia Patient Safety Foundation. Episode #103. Keeping patients and the environment safe. Published 2022. Accessed April 30, 2024. Link
- Betchtel A. Anesthesia Patient Safety Foundation. Episode #104 Continuing the conversation on sustainable healthcare. Published 2022. Accessed April 30, 2024. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.