Copy link
Sepsis in Pregnancy
Last updated: 07/30/2025
Key Points
- Sepsis remains a leading cause of potentially preventable maternal morbidity and mortality across the world.
- Reducing morbidity and mortality related to maternal sepsis requires improvement in the recognition of infection, expedited treatment, and management of end-organ dysfunction with appropriate escalation of care when needed.
- Protocols and bundles may facilitate the diagnosis of maternal sepsis and ensure consistent management.
Introduction
- Maternal sepsis is a life-threatening condition defined as organ dysfunction resulting from infection during pregnancy, childbirth, postabortion, or the postpartum period.
- Based on the Sepsis-2 definition of severe sepsis, the rate of sepsis in the pregnant population is estimated to be between 1/2000 and 1/10,000.1
- The mortality rate of sepsis in the United States remains around 11–13% of all maternal deaths over the last three decades, despite the publication of Surviving Sepsis guidelines starting in 2004.2
Etiology
Diagnoses
- The most common sources of infection during pregnancy are:1
- Genitourinary (45%)
- Chorioamnionitis (25-30%)
- Endometritis (25%)
- Respiratory (11-30%)
- Gastrointestinal (10%)
- Skin and soft tissue infections (6%)
- Others: endocarditis, meningitis, central line-associated bacterial infection, bacteremia, osteomyelitis, infective arthritis, encephalitis, and septic thrombophlebitis
- Genitourinary (45%)
Organisms
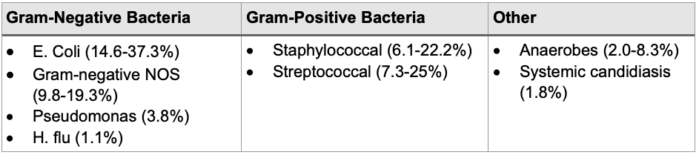
Table 1. Common culprit organisms in maternal sepsis1,3
Risk Factors for Maternal Sepsis
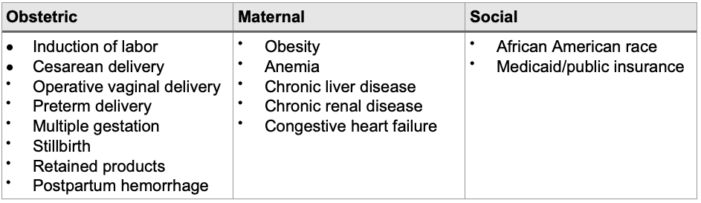
Table 2: Risk factors for maternal sepsis.4
Signs and Symptoms of Sepsis
- Sepsis-3 definition defines septic shock as a subset of sepsis in which profound circulatory, cellular, and metabolic abnormalities are associated with an increased risk of mortality than with sepsis.5
- Normal maternal physiology mimics a hyperdynamic state that makes it challenging to detect evolving sepsis.
- Normal baseline increase in heart rate up to 100bpm
- Expected PaCO2 of 30 mmHg due to increased minute ventilation
- Normal elevated white blood cell count during active labor
- Elevated lactate levels up to 4.0mmol/L
- Systemic Inflammatory Response syndrome criteria combined with suspected and/or confirmed infection and various other indicators of end-organ dysfunction may identify developing sepsis
- High sensitivity, poor sensitivity in detecting maternal sepsis
- Quick Sequential Organ Failure Assessment score identifies patients in emergency room or general floor who are at risk of developing sepsis
- Low sensitivity, high specificity in detecting maternal sepsis
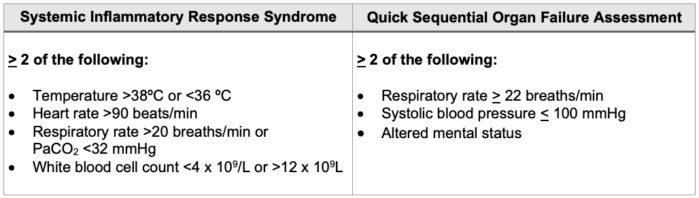
Table 3. Systemic Inflammatory Response syndrome versus Quick Sequential Organ Failure Assessment definitions
Early Warning Systems
- Early warning systems seek to identify preventable morbidity and mortality from several conditions, including sepsis.
- Maternal Early Warning Criteria (MEWC) were developed using pregnancy-adjusted vital sign and symptoms triggers. Any patient who meets one or more criteria should receive a prompt bedside evaluation by a clinician for possible diagnostic or therapeutic intervention.
- The sensitivity and specificity of the MEW (>1) criteria in peripartum patients with known sepsis is 82% and 87%.4
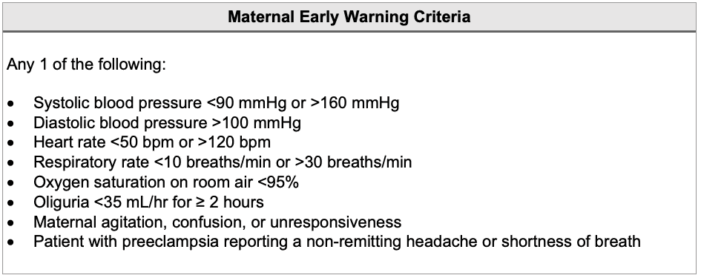
Table 4. Maternal early warning criteria6-7
Initial Management for Suspected Sepsis
Recognition and Immediate Management
- The World Health Organization (WHO) and the California Maternal Quality Care Collaborative (CMQCC) both provide diagnostic and therapeutic algorithms to assist providers in detecting and promptly managing maternal sepsis.
- WHO criteria: if infection and organ dysfunction are present → diagnose maternal sepsis
- Identify and control the source → send cultures; start antibiotics within 1 hour of suspected sepsis; monitor
- Clinical evaluation and management → point-of-care assessment of organ function; fluid resuscitation; hemodynamic and respiratory support; monitor
- CMQCC criteria
- An initial sepsis screen based on physiologic triggers → if 2 of the 4 pregnancy-adjusted screening values are met, the provider is prompted to start antibiotics and administer fluids as well as increase monitoring and surveillance.
- A second, confirmation step based on additional pregnancy-adjusted measurements for end-organ dysfunction → if 1 of the 7 systems has criteria met, the provider is prompted to take action and identify sepsis versus septic shock, and again, provide treatment and possible consultation.
Surviving Sepsis Campaign Key Recommendations8
- Administer 30 mL/kg crystalloid for hypotension or lactate > 4 mmol/L
- Resuscitation may be guided by a decrease in serum lactate in patients with an elevated lactate level.
- Administer broad-spectrum antibiotics immediately, ideally within 1 hour of recognition of sepsis (Table 5)
- Obtain blood cultures prior to administration of antibiotics
- Administer vasopressors if the patient remains hypotensive during or after fluid resuscitation for a goal mean arterial pressure ≥ 65 mmHg
- Patients with sepsis or septic shock who require intensive care unit (ICU) admission should be admitted within 6 hours.
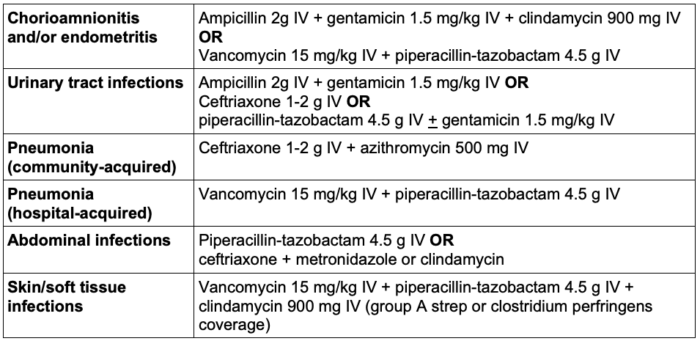
Table 5. Recommended antibiotics based on the suspected source of infection targeted to cover the most common pathogens.9
Critical Care Management of Sepsis
ICU Admission Indications
- Aggressive hemodynamic support, including vasopressors
- Invasive monitoring, including arterial and/or central venous monitoring, maintenance, and interpretation
- Invasive mechanical ventilation
- Mechanical circulatory support
Preventable Morbidity
- Delayed antibiotic initiation
- Inadequate antibiotic coverage
- Delayed ICU admission or escalation of care
- Lack of recognition
Post-ICU Care
- Postpartum separation of mother and child may affect maternal-infant bonding and the ability to breastfeed.
- Posttraumatic stress disorder, depression, and/or anxiety are common psychiatric consequences of maternal ICU admission.
- Patients may experience also impaired quality of life including worsened mobility, self-care, and pain.
- Close follow-up with providers with particular attention to mental health crisis following critical illness is imperative.
References
- Bauer ME, Bateman BT, Bauer ST, Shanks AM, Mhyre JM. Maternal sepsis mortality and morbidity during hospitalization for delivery: temporal trends and independent associations for severe sepsis. Anesth Analg. 2013;117(4):944-50. PubMed
- Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy-related mortality in the United States, 2011-2013. Obstet Gynecol. 2017;130(2):366-73. PubMed
- Bauer ME, Lorenz RP, Bauer ST, Rao K, Anderson FWJ. Maternal deaths due to sepsis in the state of Michigan, 1999-2006. Obstet Gynecol. 2015;126(4):747-52. PubMed
- Bauer ME, Housey M, Bauer ST, et al. Risk factors, etiologies, and screening tools for sepsis in pregnant women: A multicenter case-control study. Anesth Analg. 2019;129(6):1613-20. PubMed
- Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801-10. Link
- Ryan HM, Jones MA, Payne BA, et al. Validating the performance of the modified early obstetric warning system multivariable model to predict maternal intensive care unit admission. J Obstet Gynaecol Can. 2017;39(9):728-733.e3. PubMed
- Mhyre JM, D'Oria R, Hameed AB, et al. The maternal early warning criteria: a proposal from the national partnership for maternal safety. Obstet Gynecol. 2014;124(4):782-6. PubMed
- Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181-1247. PubMed
- Shields A, de Assis V, Halscott T. Top 10 pearls for the recognition, evaluation, and management of maternal sepsis. Obstet Gynecol. 2021;138(2):289-304. PubMed
- ACOG Practice Bulletin No. 211: Critical care in pregnancy. Obstet Gynecol. 2019;133(5):e303-e319. PubMed
Other References
- Bauer MEB. OpenAnesthesia. OA-SOAP Fellows Webinar Series. Maternal Sepsis. Published: June 1, 2018. Accessed July 30, 2025. Link
- World Health Organization. Trends in maternal mortality 2000 to 2020: estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division. Geneva: World Health Organization. License: CC BY-NC-SA 3.0 IGO.Published: February 23, 2023. Accessed: July 30, 2025. Link
- Gibbs R, Bauer M, Olvera L, et al. California Maternal Quality Care Collaborative (CMQCC). Improving Diagnosis and Treatment of Maternal Sepsis. Published: January 2020. Updated: July 1, 2022. Accessed: July 30, 2025. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.