Copy link
Rheumatoid Arthritis
Last updated: 09/04/2025
Key Points
- Rheumatoid arthritis (RA) is a chronic autoimmune disorder that primarily affects synovial joints, leading to joint degeneration, systemic inflammation, and extra-articular manifestations.
- Common RA treatments, including corticosteroids and disease-modifying antirheumatic drugs (DMARDs), may result in immunosuppression and require perioperative adjustments such as stress-dose steroids.
- Airway difficulties can arise due to temporomandibular joint mobility, cervical spine subluxation, and cricoarytenoid involvement.
- Regional or neuraxial anesthesia is often preferred when applicable to avoid manipulation of a potentially difficult airway.
Introduction
- RA is a systemic autoimmune disorder primarily affecting the small, synovial joints of the hands and feet. However, the disease can extend to include axial joint involvement (notably the cervical spine), systemic inflammation, and extra-articular manifestations.1,2
- RA is more prevalent in Western and Northern Europe and North America, particularly in individuals of European descent. It is approximately twice as common in women, with a lifetime risk of 3.6% in females compared to 1.7% in males.2
- The pathogenesis involves genetic predisposition – particularly HLA-DRB1 polymorphisms – and environmental factors such as smoking and obesity.2
- RA can be seropositive (positive for rheumatoid factor [RF] or anti-cyclic citrullinated peptide antibodies [CCP]) or seronegative. About 10% of patients with clinical RA are seronegative.2
- RA heritability is 40-65% for seropositive and 20% for seronegative disease.2
- Patients with RA frequently undergo orthopedic procedures (hip, knee, hand, foot) due to joint damage.3
- RA is the most common rheumatoid disease in the intensive care unit and is associated with high mortality.3
Pathophysiology
- RA is thought to be triggered by environmental exposures (e.g., smoking) in genetically susceptible individuals, leading to the creation of citrullinated peptides and the development of autoantibodies like RF and anti-CCP. These may appear years before clinical symptoms.2
- The immune response targets the synovium, causing infiltration by innate immune cells, activation of the adaptive immune system (T and B cells), and eventual synovial hyperplasia. Osteoclast activation and fibroblast proliferation result in bony erosions and systemic inflammation.
- Although any synovial joint can be affected, RA predominantly targets peripheral joints. The cervical spine is an axial structure commonly involved due to the presence of synovial joints in this region.
- Notable comorbidities include cardiovascular disease, interstitial lung disease, and anemia of chronic disease2,3 (Table 1).
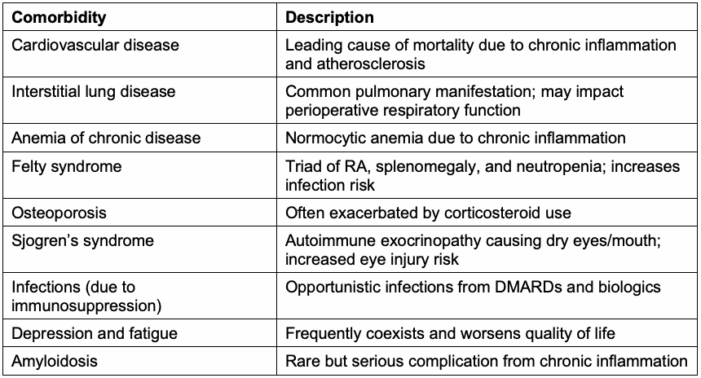
Table 1. Common comorbidities of rheumatoid arthritis
Clinical Course
- RA is a chronic and progressive disease with no known cure. Early initiation of treatment (within six months of symptom onset) is associated with better long-term outcomes.2
- By 10 years post-diagnosis, about 40% of patients experience significant disability impacting activities of daily living.2
- The primary cause of mortality is cardiovascular complications from systemic inflammation and accelerated atherosclerosis.2
Treatment
- The primary goal of RA treatment is early diagnosis and disease-modifying treatment to prevent irreversible joint and systemic damage.
- Treatment classes incude2-5:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Symptom relief; no effect on disease progression
- Corticosteroids: Bridging therapy to DMARDs and treatment of RA flares or complications (e.g., interstitial lung disease)
- Nonbiologic DMARDs: Methotrexate is first-line for disease control and management
- Biologic DMARDs (e.g., tumor necrosis factor inhibitors): Second-line; used when methotrexate fails
- Janus Kinases (JAK) inhibitors (e.g., tofacitinib, baricitinib): Reserved for specific cases
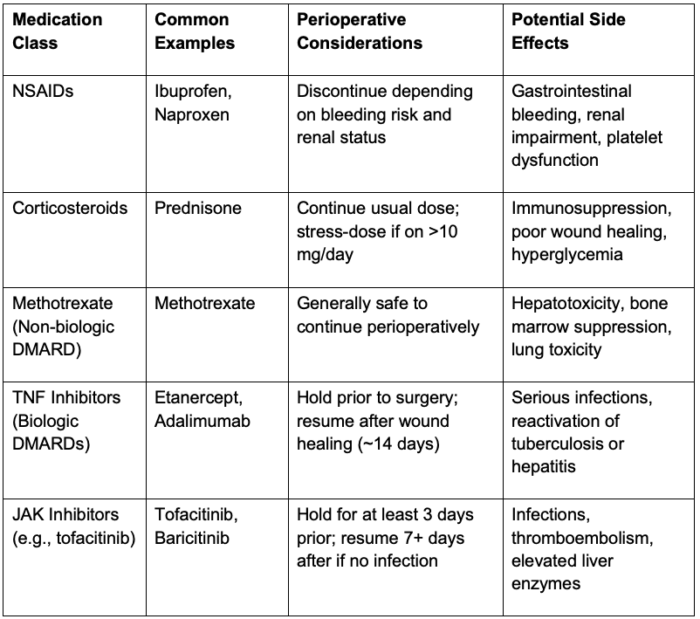
Table 2. Perioperative considerations of medications used for rheumatoid arthritis
Preoperative Considerations
- Airway and musculoskeletal evaluation
- TMJ dysfunction, cervical spine instability, and cricoarytenitis can complicate airway management.1,3
- Assess joint pain and range of motion for regional block placement and intraoperative positioning considerations.1
- Airway assessment, such as Mallampati score, mandibular protrusion, and mouth opening, is helpful; consider imaging (e.g., cervical spine X-rays) if instability is suspected.3
- Cardiac assessment
- RA-associated risks include pericarditis, cardiac amyloidosis, ischemic heart disease, valvular disease, and conduction abnormalities.1,4
- Preoperative electrocardiogram for all patients; echocardiography if indicated1,3
- Pulmonary assessment
- Pulmonary involvement may include interstitial lung disease or pleural effusions.
- Consider pulmonary function testing, arterial blood gas, and/or imaging if lung involvement is suspected.1
- Hematologic evaluation:
- RA may cause anemia of chronic disease or thrombocytosis.
- Felty syndrome may lead to severe neutropenia.1,2
- Baseline complete blood count for all patients; erythrocyte sedimentation rate and reactive C protein if indicated.3
- Skin assessment:
- Fragile skin and impaired wound healing are common.
- Close perioperative monitoring and gentle handling are required.1
- Medication review:
- Patients with RA should be evaluated by their rheumatologist prior to any planned surgery to ensure optimization.
- Corticosteroids: Continue usual dose; consider stress-dose steroids for patients on >10mg daily.1
- Nonbiologic DMARDs: Continue perioperatively6
- Biologic DMARDs: Hold prior to surgery and restart postoperatively once wound healing is complete or a minimum of 14 days6
- JAK inhibitors: Hold prior to surgery for at least 3 days and restart postoperatively for at least 7 days3
- NSAIDs: Discontinue perioperatively depending on bleeding risks and renal function7
- Cervical spine involvement:
- Atlantoaxial subluxation is potentially dangerous and may be asymptomatic.
- Cervical imaging should be obtained if symptoms or risk factors are present.4
- Risk factors include long-standing disease, female sex, glucocorticoid use, erosive disease, and high inflammatory markers.7
- Cricoarytenoid cartilage Involvement:
- Patients may present with hoarseness, stridor, or dyspnea.3
- Preoperative evaluation with laryngoscopy or computed tomography (CT) may be necessary.
- Airway strategies: Facemask or supraglottic airway to avoid intubation when feasible3,4
Intraoperative Considerations
- Airway management:
- Use video or fiberoptic laryngoscopy1
- Manual in-line stabilization is advised for all RA patients during intubation.
- Avoid sniffing position in cervical instability4
- Smaller endotracheal tubes may be required.
- Regional/neuraxial anesthesia:
- Preferred when possible to avoid airway manipulation1,3
- Careful positioning is necessary due to joint limitations.1,3
- Greater block extension should be expected in patients with RA.3
- Ocular protection:
- Eye protection is important to prevent damage to the cornea and mucous membranes.3
- RA is associated with Sjogren’s and keratoconjunctivitis.3
- Hemostasis:
- Tranexamic acid should be considered to minimize transfusion risk.3
Postoperative Considerations
- Respiratory:
- Monitor closely for airway obstruction or edema, particularly in patients with cricoarytenitis1
- Consider mechanical ventilation if needed
- Neurological:
- Clinicians should watch for delayed signs of cervical spine instability: myelopathy, brainstem compression, or vertebrobasilar insufficiency.
- Analgesia:
- Patient-controlled analgesia pumps may be difficult for RA patients with joint deformities.1
- Immunosuppression/Infection
- High suspicion for infection due to immunosuppression from RA or its treatments should be maintained.2,5
References
- Stasic AF, Heine CL, Fisher G, Choi SW, Smith J. Rare Coexisting Diseases. In: Barash, Cullen, and Stoeltings. Clinical Anesthesia. Ninth Edition. Philadelphia, PA, Lippincott Williams & Wilkins; 2023: 604-606
- Chauhan K, Jandu JS, Brent LH, Al-Dhahir MA. Rheumatoid arthritis. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2025. Accessed February 14, 2025. Link
- Radkowski P, Szewczyk M, Sztaba K, Kęska M. A review of the current status of anesthetic management of patients with rheumatoid arthritis. Med Sci Monit. 2024;30:e943829. PubMed
- Kim HR, Kim SH. Perioperative and anesthetic management of patients with rheumatoid arthritis. Korean J Intern Med. 2022;37(4):732-739. PubMed
- Goodman SM, Springer B, Guyatt G, et al. 2017 American College of Rheumatology/American Association of Hip and Knee Surgeons guideline for the perioperative management of antirheumatic medication in patients with rheumatic diseases undergoing elective total hip or total knee arthroplasty. Arthritis Rheumatol. 2017;69(8):1538-1551. PubMed
- Axford JS. Preoperative evaluation and perioperative management of patients with rheumatic diseases. In: Post TW, ed. UpToDate. 2025. Accessed February 11, 2025. Link
- Currier BL, Coblyn J. Cervical subluxation in rheumatoid arthritis. In: Post TW, ed. UpToDate. 2025. Accessed February 11, 2025. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.