Copy link
Rhabdomyolysis
Last updated: 09/09/2025
Key Points
- Rhabdomyolysis is the breakdown of skeletal muscle fibers, leading to the release of myoglobin and electrolytes into the bloodstream. Causes include trauma, exertion, drugs/toxins, infections, metabolic disorders, and perioperative triggers such as succinylcholine, volatile anesthetics, and malignant hyperthermia susceptibility.
- The classic triad of muscle pain, weakness, and dark urine is uncommon. More often, patients present with myalgias, fatigue, and tea-colored urine. Diagnosis is based on clinical suspicion and laboratory findings, particularly markedly elevated creatine kinase, electrolyte disturbances, and myoglobinuria.
- Management focuses on aggressive hydration, correction of electrolytes, and prevention of complications such as acute kidney injury, compartment syndrome, and cardiac dysrhythmias. In the perioperative setting, high-risk patients require avoidance of succinylcholine and volatile anesthetics, close monitoring of electrolytes and renal function, and early intervention for complications.
Introduction1,2,3
- Rhabdomyolysis is a serious and potentially life-threatening condition caused by the breakdown of skeletal muscle fibers, leading to the release of their intracellular contents, including myoglobin, electrolytes, and sarcoplasmic proteins, into the bloodstream. This cascade can precipitate metabolic derangements, acute kidney injury, and life-threatening complications if not recognized early.
- The condition arises from a wide variety of causes, including trauma, infections, medications and illicit drugs, extreme exertion, and inherited muscle disorders. Clinically, while the classic triad of muscle pain, weakness, and dark urine is often cited, it is present in only 1-10% of cases. Laboratory evaluation is central, with elevated creatine kinase serving as the most sensitive diagnostic marker.
- Management is mostly supportive and hinges on early and aggressive fluid resuscitation, correction of electrolyte abnormalities, and prevention of renal injury. Prognosis depends on the underlying etiology, the timeliness of diagnosis, and whether complications such as acute kidney injury develop.
- For the anesthesiologist, recognition of risk factors in the perioperative period is essential. Use of succinylcholine and volatile inhalational anesthetics, malignant hyperthermia, and underlying neuromuscular diseases all heighten the risk of rhabdomyolysis in surgical patients.
Etiology1,3
- Rhabdomyolysis can arise from a wide variety of causes. Trauma and ischemia are among the most common, including crush injuries, prolonged immobilization, vascular compression, compartment syndrome, and fractures of the lower extremities that cause arterial occlusion. Additional causes include prolonged tourniquet application, surgical clamping, high-voltage electrical injuries, extensive third-degree burns, and even prolonged physical restraint. Exertional causes such as extreme physical activity, particularly when compounded by hypokalemia or sickle cell trait, may also precipitate rhabdomyolysis, as can severe hyperthermia from heat stroke. Seizures represent another important trigger due to intense and sustained muscle contractions.
- Drugs and toxins are a frequent etiology, with statins, fibrates, antipsychotics, selective serotonin reuptake inhibitors, colchicine, alcohol, cocaine, heroin, amphetamines, and anesthetic agents such as succinylcholine all implicated.
- A broad range of inherited and metabolic disorders predispose patients to rhabdomyolysis, including disorders of glycogenolysis, glycolysis, purine metabolism, and lipid metabolism, as well as various inherited muscular disorders. Metabolic and electrolyte disturbances such as hypokalemia, hypophosphatemia, and diabetic ketoacidosis also contribute. Importantly, pathogenic variants in the RYR1 and CACNA1S genes confer susceptibility to malignant hyperthermia and perioperative rhabdomyolysis.
- Endocrinopathies, such as adrenal insufficiency, hypothyroidism, hyperaldosteronism, and diabetic ketoacidosis, have been implicated.
- Both bacterial (such as Gram-positive bacteria) and viral (including influenza A and B, and the human immunodeficiency virus) infections can also cause rhabdomyolysis. Organic toxins from stings and bites from snakes, bees, spiders, and scorpions have also been reported.
- In the anesthetic context, risk is heightened by exposure to succinylcholine, volatile inhalational anesthetics, prolonged tourniquet use, and reperfusion injury, especially in patients with underlying neuromuscular disorders or genetic susceptibility to malignant hyperthermia. Recognition of these triggers is critical for anesthesiologists to anticipate, prevent, and manage perioperative rhabdomyolysis.
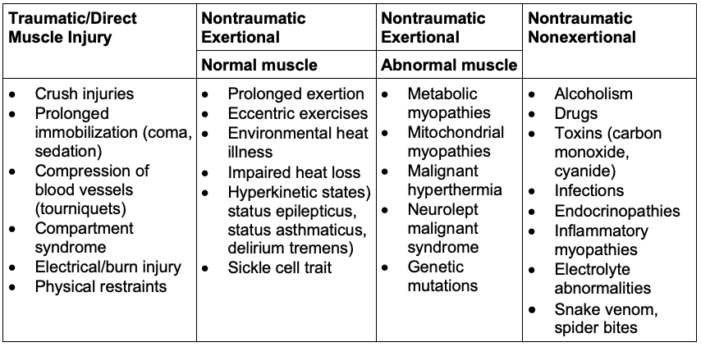
Table 1. Causes of rhabdomyolysis1
Pathophysiology4
- Regardless of the etiology of rhabdomyolysis, the pathophysiology of rhabdomyolysis follows a common pathway characterized by an increase in cytoplasmic ionized calcium. There is muscle cell breakdown, either through direct cell membrane destruction or energy depletion. Subsequently, the release of cytotoxic intracellular components causes capillary injury and third-spacing of fluids. Edema, ischemia, and cell necrosis cause metabolic acidosis and electrolyte abnormalities.
- The etiology of rhabdomyolysis-associated acute kidney injury is multifactorial, involving hypovolemia from third-spacing and edema, decreased renal blood flow, and direct myoglobin cytotoxicity to the kidneys (Figure 1). Myoglobin is the primary nephrotoxin in rhabdomyolysis.

Figure 1. Mechanism of acute kidney injury in rhabdomyolysis. Source: Chavez LO, et al. Crit Care Med. 2016. CC BY 4.0.4
Clinical Presentation2,3
- The classic triad of rhabdomyolysis consists of muscle pain, weakness, and dark urine. However, this combination is only observed in 1-10% of patients. More commonly, patients present with myalgias, localized muscle swelling or tenderness, and systemic symptoms such as fatigue, malaise, and low-grade fever. Urine discoloration, often described as “tea-colored” or “Coca-Cola-colored,” results from myoglobinuria. Signs of dehydration, such as decreased skin turgor or dry oral mucosa, may also be present. Muscle-related findings typically develop over the course of hours to days.
- Complications may manifest as acute kidney injury with oliguria and rising creatinine, as well as electrolyte abnormalities including hyperkalemia, hyperphosphatemia, early hypocalcemia, and hyperuricemia. Severe cases can progress to compartment syndrome, disseminated intravascular coagulation, or life-threatening cardiac dysrhythmias.
- The patient’s history often provides important clues to the underlying cause. Depending on the etiology, individuals may report traumatic accidents, recent surgical procedures, illicit drug use, insect bites, heat exertion, or changes in medication regimens, including increasing doses of prescribed drugs, newly initiated agents, or over-the-counter supplements.

Figure 2. “Tea-colored” urine from a patient with rhabdomyolysis. Source: James Hellman, MD. Wikipedia Commons. CC BY SA 3.0. Link
Diagnosis2,3,5
- The diagnosis of rhabdomyolysis is primarily based on both clinical and laboratory findings. Creatine kinase (CK) is the most sensitive and reliable marker, with levels typically exceeding 5,000 units/L in non-exertional cases and often greater than 10,000 units/L in exertional rhabdomyolysis, which is generally more than five times the upper limit of normal. Serum and urine myoglobin may also be elevated, though these are less reliable due to the rapid clearance of myoglobin. Laboratory evaluation frequently reveals electrolyte abnormalities, including hyperkalemia, hyperphosphatemia, early hypocalcemia, and hyperuricemia.
- Assessment should also include renal function tests, such as serum creatinine and blood urea nitrogen, to evaluate for acute kidney injury, as well as serum electrolytes to detect potential complications. Liver enzymes (aspartate aminotransferase) and alanine aminotransferase) may be elevated because of muscle injury. Urinalysis often demonstrates a positive dipstick for heme in the absence of red blood cells, reflecting myoglobinuria.
- Although imaging such as magnetic resonance imaging or ultrasound may reveal muscle edema, it is rarely necessary for diagnosis. The key principle is that diagnosis relies on the combination of clinical suspicion and laboratory abnormalities, and treatment should not be delayed while awaiting confirmatory myoglobin levels.
- The McMahon rhabdomyolysis score is a validated risk prediction tool to identify patients at risk for acute kidney injury requiring renal replacement therapy or in-house mortality. A score of less than 6 indicates a low risk for acute kidney injury or the need for renal replacement therapy5 (Table 2).
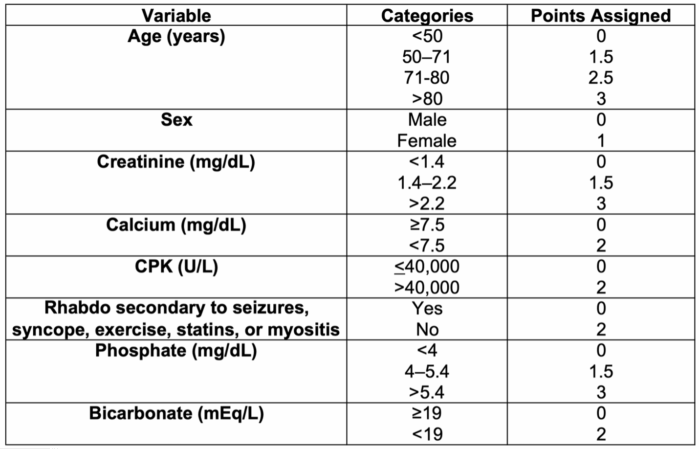
Table 2. McMahon rhabdomyolysis scoring. Source: McMahon GM, et al. A risk prediction score for kidney failure or mortality in rhabdomyolysis. JAMA Intern Med. 2013;173(19):1821–8. Link.5
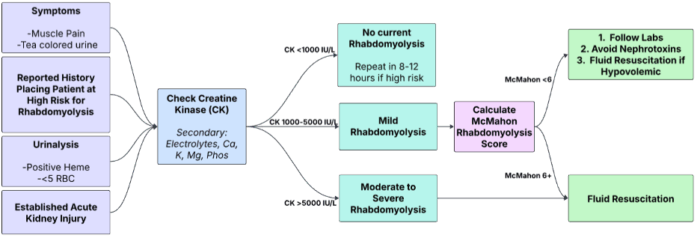
Figure 3. Diagnostic flowchart for rhabdomyolysis. Adapted from Farkas J. Rhabdomyolysis. EMCrit Project. Published June 25, 2021. Link.6
Management3
- The initial management of rhabdomyolysis focuses on aggressive intravenous hydration with isotonic saline to maintain a urine output of at least 200-300 mL per hour. Careful monitoring and correction of electrolyte abnormalities, particularly hyperkalemia, are essential to prevent life-threatening complications. Nephrotoxic agents such as non-steroidal anti-inflammatory drugs and intravenous contrast should be avoided to reduce the risk of renal injury.
- Adjunctive measures may be considered in select cases. Urinary alkalinization with sodium bicarbonate can be used to reduce myoglobin nephrotoxicity, particularly when creatine phosphokinase (CPK) levels exceed 30,000 U/L in the absence of oliguria, anuria, or established acute kidney injury. Mannitol may improve urine output in patients with crush injuries but should only be initiated after urine output is established at ≥20 mL/hr. It should be avoided in patients with acute kidney injury, oliguria, or anuria, due to risks of volume overload and hyperosmolality. Current literature does not support the routine use of combined mannitol and bicarbonate for preventing pigment-induced acute kidney injury.
- Management of complications is tailored to the underlying condition. Compartment syndrome requires emergent orthopedic consultation for potential fasciotomy. Disseminated intravascular coagulation is treated with supportive transfusion therapy, including fresh frozen plasma, cryoprecipitate, and platelet transfusions. Malignant hyperthermia should be treated promptly with dantrolene sodium. For sepsis, appropriate antibiotics and vasopressors are indicated. Inflammatory myopathies may benefit from corticosteroids.
- Ongoing monitoring should include serial measurements of CK, electrolytes, renal function, and urine output to assess disease progression and response to therapy.
Anesthetic Considerations7
- Anesthetic management in patients with rhabdomyolysis requires careful selection of agents to avoid exacerbating muscle injury or precipitating malignant hyperthermia. In particular, succinylcholine and volatile inhalational anesthetics should be avoided in at-risk individuals. Perioperative care must also focus on preventing acute kidney injury and managing life-threatening electrolyte disturbances, especially hyperkalemia and hypocalcemia.
- Preoperatively, it is important to identify high-risk patients, including those with neuromuscular disorders, a prior history of rhabdomyolysis, chronic statin therapy, or underlying metabolic disease. Baseline creatine kinase, electrolytes, and renal function should be obtained if clinical concern exists.
- Intraoperatively, succinylcholine should be strictly avoided in patients at risk. Aggressive intravenous hydration is a cornerstone of management to prevent renal complications. Potassium and acid–base status must be closely monitored, while steps should be taken to minimize tourniquet time and to maintain adequate tissue perfusion and oxygenation. Vigilance for compartment syndrome and metabolic derangements (hyperkalemia, hypocalcemia, and acidosis) is essential.
- Postoperatively, vigilant surveillance is required to detect early signs of recurrence or complications, such as dark urine, rising creatine kinase levels, or electrolyte abnormalities. Aggressive fluid resuscitation should be maintained, and early nephrology consultation is warranted in patients with evidence of renal dysfunction or electrolyte instability.
References
- Bhai S, Dimachkie MM, Rhabdomyolysis: Epidemiology and etiology. In: Targoff IN, Shefner JM, eds. UpToDate; 2025. Accessed August 25, 2025. Link Link
- Bhai S, Dimachkie MM, Rhabdomyolysis: Clinical manifestations and diagnosis. In: Targoff IN, Shefner JM, eds. UpToDate; 2025. Accessed August 25, 2025. Link
- Rout P, Chippa V, Adigun R. Rhabdomyolysis. In: StatPearls (Internet). Treasure Island, FL. StatPearls Publishing; 2025. Accessed August 25, 2025. Link
- Chavez LO, Leon M, Einav S, Varon J. Beyond muscle destruction: A systematic review of rhabdomyolysis for clinical practice. Crit Care Med. 2016;44(8):e809-e818. PubMed
- McMahon GM, Zeng X, Waikar SS. A risk prediction score for kidney failure or mortality in rhabdomyolysis. JAMA Intern Med. 2013;173(19):1821–8. Link
- Farkas J. Rhabdomyolysis. EMCrit Project. Published June 25, 2021. Link
- Zimmerman JL, Shen MC. Rhabdomyolysis. Chest. 2013;144(3):1058-1065. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.