Copy link
Retinopathy of Prematurity
Last updated: 05/28/2025
Key Points
- Retinopathy of prematurity (ROP) is a vascular proliferative disorder that affects the retina of preterm infants, leading to incomplete and abnormal vascularization of the retina.
- The incidence and severity of ROP increase with decreasing gestational age and birth weight.
- Oxygen plays a crucial role in the development of ROP. Recent oxygen saturation targeting trials have shown an increase in mortality with lower target ranges (85-89%), and emerging evidence-based consensus suggests that the optimal saturation range is closer to 91-95%.
- Specific anesthetic considerations include maintaining optimal oxygenation, enhancing intubation conditions to maximize first-attempt success rates, ensuring thermal regulation, and the potential for postoperative apnea in premature infants.
Incidence and Risk Factors
- ROP is a leading cause of childhood blindness.
- Over 20,000 infants experience blindness annually from ROP, and an additional 12,000 suffer from visual impairment.1
- The incidence and severity of ROP increase with decreasing gestational age and birth weight. ROP is rarely diagnosed in infants more than 32 weeks’ gestational age.2 Other risk factors and conditions associated with ROP are listed in Table 1.
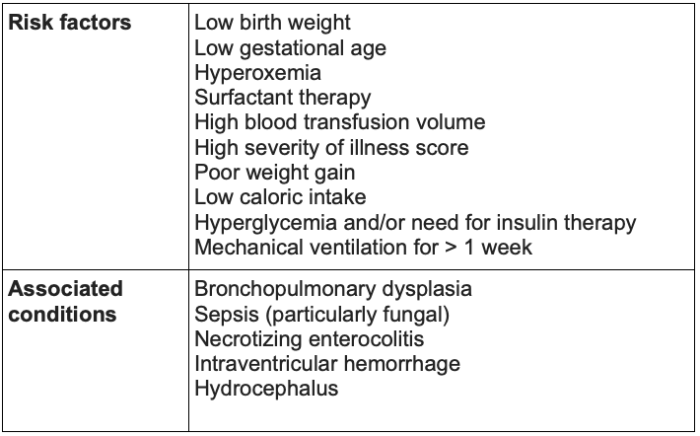
Table 1. Risk factors and conditions associated with ROP2
Pathogenesis of ROP
- Vascularization of the retina typically begins at 15 to 18 weeks of gestation. Retinal blood vessels originate at the optic disc and grow peripherally. The nasal retina is vascularized by week 36, and the temporal retina is complete by week 40.2
- The pathogenesis of ROP involves two stages. An initial injury, such as hypotension, hypoxia, or hyperoxia, interferes with the development of blood vessels, thereby affecting normal angiogenesis.2
- Subsequently, vessels either resume normal growth (no ROP) or aberrant neovascularization into the vitreous occurs (ROP). The increased permeability of these new vessels can lead to retinal edema and hemorrhage.
- This neovascularization can contribute to the formation of fibrovascular tissue, which contracts and places traction on the retina, ultimately leading to retinal distortion or detachment.
- Oxygen plays a critical role in the development of ROP.3
- The fetus in utero exists in a hypoxic state (PaO2 22-24 mmHg).
- Retinal vessels grow from the optic nerve to the peripheral avascular retina.
- The hypoxic environment of the fetus stimulates the production of vascular endothelial growth factor (VEGF), which leads to the growth of retinal vessels into the previously avascular retina.
- When premature infants have prolonged exposure to hyperoxic environments, VEGF is downregulated. This stunts retinal vessel growth and results in an avascular retina.
Classification4-6
- The International Classification of Retinopathy of Prematurity (ICROP3) is used to classify the disease based on zone, stage, and presence or absence of plus disease.
- Components of ICROP3:
- Zone
- Three retinal zones have been defined, centered on the optic disc.
- The most posterior area of retinal vascularization or ROP lesion is used for classification purposes.
- Stage (1-3) of acute disease
- Stage 1 occurs when a white demarcation line is present.
- Stage 2 occurs when the demarcation line progresses into a raised ridge.
- Stage 3 is characterized by extraretinal neovascular proliferation.
- Stages 4 and 5 involve retinal detachment
- Stage 4 is partial detachment of the retina.
- Stage 5 is defined by total detachment of the retina.
- Plus and pre-plus disease
- Plus disease is characterized by numerous tortuous and dilated retinal vessels.
- Pre-plus disease is a milder form in which there is abnormal tortuosity and dilation of vessels that do not meet the criteria for plus disease.
- Regression is the resolution of the disease, which can occur spontaneously, in response to anti-VEGF treatment, or after laser treatment.
- Reactivation occurs when findings of acute disease listed in stages 1-3 reappear following regression of the disease.
- Zone
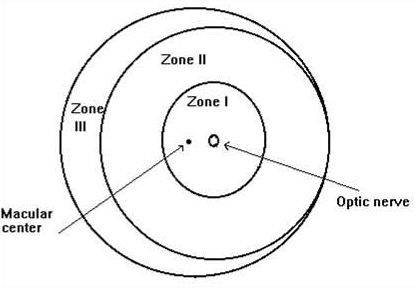
Figure 1. Zones of the retina in ROP. Source: Wikipedia. Public Domain. Accessed March 1, 2025. Link
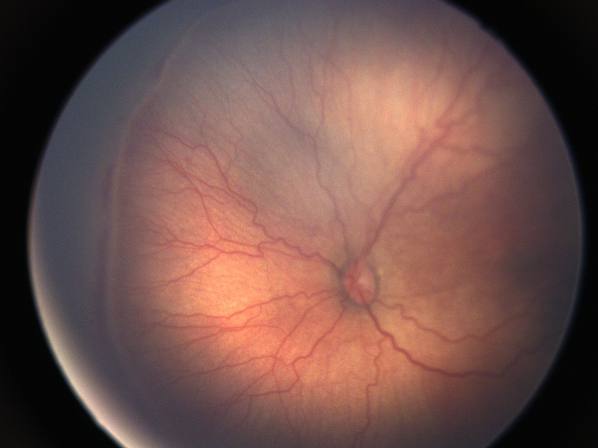
Figure 2. Color fundus photo of the left eye showing nasal Stage 3 ROP with Plus disease. Courtesy of James Bowsher, MD.
Long-Term Sequelae7
- ROP can regress without any significant long-term sequelae. However, it can also lead to permanent ocular disabilities. These may include:
- Retinal detachment
- Macular abnormalities
- These are often correlated with the severity of the acute phase of disease.
- The most common macular abnormalities resulting from ROP include a small foveal avascular zone and blunting of the foveal depression.
- Retinoschisis
- This is a disorder that occurs when the retina divides into two or more layers.
- This can occur from chronic traction from an involuted stage 3 ROP and can lead to significant visual disability.
- Retinal vascular changes
- Those affected may have persistent retinal vessel tortuosity, abnormal branching of vessels, and telangiectatic vessels, which can ultimately lead to vitreous hemorrhage.
- Angle-closure glaucoma
- Patients with a history of ROP are prone to the development of angle-closure glaucoma, which presents later in life.
- Persistent avascular retina
- This occurs when there is incomplete vascularization into the peripheral avascular retina. It can present following the spontaneous regression of disease or following treatment and may occur in the peripheral or posterior retina.
- These persistent avascular areas may undergo degenerative changes that can lead to complications such as retinal detachment later in life.
Treatment
- Treatment consists of retinal ablative therapy, including laser photocoagulation, or injection of anti-VEGF agent into the vitreous. The choice between the two therapies is typically made with shared decision-making between the treating provider and the patient’s caregiver.7
- Initiation of treatment, as well as the type of treatment offered, is based on the severity of the disease. Laser photocoagulation has long been recognized as the gold standard treatment for ROP, though both options have been shown to be effective. Long-term outcomes and side effects have been more clearly defined when compared with anti-VEGF therapy.7
- Laser photocoagulation utilizes a diode or argon laser aimed through the pupil to ablate the peripheral avascular retina, to prevent further growth of abnormal blood vessels. This helps minimize vision loss by preserving the central retina, which is responsible for vision.4,7
- Anti-VEGF monoclonal antibodies can be used as monotherapy or in combination with laser photocoagulation. This therapy can typically be administered under local anesthesia at the bedside, whereas laser photocoagulation is commonly administered under general anesthesia.7
- Involution of ROP occurs more quickly with anti-VEGF therapy than with laser photocoagulation. Efficacy has been shown to be similar, though laser therapy has a higher risk of structural eye problems and high myopia.7
Preoperative Evaluation
- A comprehensive preoperative assessment should focus on conditions that are commonly found in premature infants, as prematurity is the most common risk factor for ROP. These conditions can have significant implications on intraoperative and postoperative care.
- Please see the OA summary on “Prematurity” (Link) for more details.
Intraoperative Management
- Airway management
- Securing and managing the airway in infants with ROP may be challenging. One may encounter difficulties securing the airway due to low birth weight and anatomical changes. Subglottic stenosis may result as a consequence of prior prolonged intubation.
- Appropriately sized cuffed and uncuffed endotracheal tubes (ETTs) should be readily available when instrumenting the airway.
- When available, video laryngoscopy should be used to place an ETT, as this technique has been shown to have a higher first-attempt success rate with fewer complications compared to direct laryngoscopy.
- Medications to treat intraoperative bronchospasm should be available due to the high incidence of bronchopulmonary dysplasia in this patient population and propensity for bronchospasm.
- Please see the OA summary on “Optimizing Pediatric Intubation” (Link) for more details.
- Optimal intraoperative oxygenation
- It is imperative to perform continuous oxygen monitoring throughout the perioperative period on infants with ROP.
- Multiple clinical trials have investigated targeted oxygen saturation levels; however, these studies demonstrated an increased mortality rate among patients maintained within the lower saturation range of 85–89%. A clear range has not yet been identified that would minimize the rate of toxicity while also enhancing survival.8
- The American Academy of Pediatrics currently recommends targeting an oxygen saturation of greater than 85% to 89%, though emerging evidence-based consensus suggests that the optimal range is closer to 91% to 95%.8
- Temperature management
- Maintaining thermal stability in premature infants is crucial during the intraoperative period, as they are unable to regulate their own body temperature and are most susceptible to hypothermia.
- Hypothermia can increase oxygen consumption in neonates and lead to tissue hypoxia, metabolic acidosis, and increased respiratory distress. This is especially detrimental in patients who may already have compromised cardiorespiratory function.
- It is crucial to perform intraoperative core temperature monitoring using an esophageal, nasal, or rectal temperature probe.
- A combination of several warming strategies is employed, including warming the operating room, the use of forced-air warmers, and the administration of warmed fluids.
- The most effective means to prevent intraoperative hypothermia in this population is active prewarming, which should begin in the inpatient ward or ICU and continue during transport with a warmed incubator if possible.
Postoperative Management
- Postoperative apnea monitoring
- Focus should be placed on postoperative respiratory status and oxygenation monitoring as these patients are at risk for postoperative apneic episodes.
- Please see the OA summary on “Apnea of Prematurity and Postoperative Apnea” (Link) for more details.
- Postoperative admission criteria
- Recommendations regarding the admission or discharge of preterm infants from the postoperative care unit based on postconceptual age are listed as follows:
- Infants younger than 55 weeks postconceptual age, anemic (hematocrit <30%), and experiencing apnea should be admitted overnight.
- Formerly preterm infants, currently 55 to 60 weeks postconceptual age, who are not anemic and have not experienced apnea may be discharged after being monitored for twelve hours without any episodes of apnea or bradycardia in the recovery room.
- Recommendations regarding the admission or discharge of preterm infants from the postoperative care unit based on postconceptual age are listed as follows:
References
- Alselaimy R, Al Tawil L, Abouammoh MA. Anesthesia in retinopathy of prematurity. Saudi J Ophthalmol. 2022;36(3):251-259. PubMed
- Bhatt, A. Retinopathy of prematurity (ROP): Risk factors, classification, and screening. In: Post T, ed. UpToDate; 2024. Accessed March 1, 2025. Link
- Strube YNJ, Wright KW. Pathophysiology of retinopathy of prematurity. Saudi J Ophthalmol. 2022;36(3):239-242. PubMed
- Cayabyab R, Ramanathan R. Retinopathy of prematurity: Therapeutic strategies based on pathophysiology. Neonatology. 2016;109(4):369-376. PubMed
- Chiang MF, Quinn GE, Fielder AR, et al. International classification of retinopathy of prematurity, Third Edition. Ophthalmology. 2021;128(10):e51-e68. PubMed
- Dhannawat SS, van Zuuren EJ, Barron S. Retinopathy of prematurity (ROP). DynaMed. 2024. Accessed March 1, 2025. Link
- Bhatt A. Retinopathy of prematurity (ROP): Treatment and prognosis. In: Post T, ed. UpToDate; 2024. Accessed: March 1, 2025. Link
- Higgins RD. Oxygen Saturation and Retinopathy of Prematurity. Clinics in perinatology. 2019;46(3):593-99. PubMed
Other References
- Ambardekar A. Retinopathy of prematurity. OA-SPA Pediatric Podcast of the Month. 2019. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.