Copy link
Resuscitative Endovascular Balloon Occlusion of the Aorta
Last updated: 02/09/2023
Key Points
- Resuscitative endovascular balloon occlusion of the aorta (REBOA) is a tool to temporarily halt exsanguination in trauma patients with noncompressible torso or pelvic injuries.
- While the utilization of REBOA may improve mean arterial pressure and cerebral perfusion in the hemorrhaging patient, it does not correct the underlying condition and the source of bleeding.
- Anesthesiologists may play a critical role during the deflation phase of the REBOA balloon. Thus, a thorough understanding of the significant and often negative physiologic changes during this phase is critical.
Introduction
- REBOA is a novel approach to temporarily stop exsanguination in trauma patients from noncompressible torso or pelvic injuries.1-3 It offers an alternative to resuscitative thoracotomy for clamping of the descending aortic to gain distal hemorrhage control.
- REBOA involves inserting a balloon catheter through the femoral artery and advancing it to the aorta, where the balloon is typically inflated under fluoroscopic guidance in specific zones (see below) depending on the type of injury (Figure 1 and Table 1).
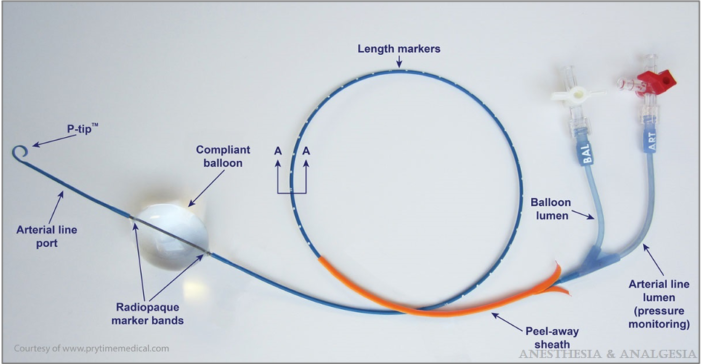
Figure 1. REBOA catheter. Reproduced with permission from Sridhar S, et al. Resuscitative endovascular balloon occlusion of the aorta. Anesth Analg. 2017;125(3):884-90.3
- The balloon partially or completely occludes the aorta.3-4 This facilitates preservation of myocardial and cerebral perfusion while the source of bleeding is identified and fixed, and the patient’s volume status and coagulopathy are corrected.5
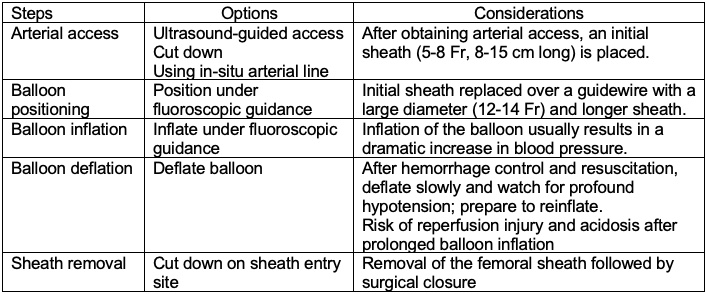
Table 1. Steps in REBOA deployment. Adapted from Stannard A, et al. Resuscitative endovascular balloon occlusion of the aorta (REBOA) as an adjunct for hemorrhagic shock. J Trauma. 2011;71(6):1869-72.2
Anatomical Zones of REBOA Deployment
The aortic zones of REBOA deployment are as follows (Figure 2).2,3
Zone I – Descending thoracic aorta (left subclavian artery to celiac arteries)
- Balloon occlusion in zone I physiologically resembles the application of an aortic cross-clamp during a resuscitative thoracotomy.
- Zone I deployment will occlude perfusion to visceral organs and should be performed only if able to expeditiously proceed with rapid control of hemorrhage.
Zone II- Paravisceral aorta (celiac artery to most distal renal artery)
- Zone II is thought to be a zone of no occlusion, and currently, there is no cited indication for zone II deployment.
Zone III- Infrarenal aorta (most distal renal artery to aortic bifurcation)
- Zone III deployment is suggested for pelvic trauma with uncontrollable hemorrhage or more distal (lower extremity) hemorrhage. Outcomes are optimized if zone III occlusion times are 30-60 minutes or less.4
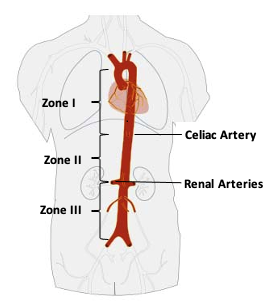
Figure 2. Aortic zones of REBOA deployment
Indications and Contraindications of REBOA
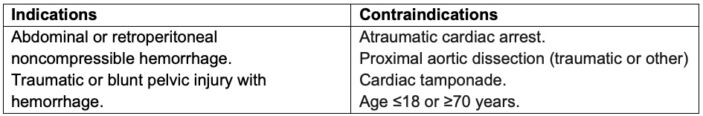
Table 2.
Efficacy of REBOA
- The American Association for the Surgery of Trauma’s Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) registry recently compared the effectiveness of REBOA to open aortic occlusion (AO) in 114 patients across 8 trauma centers.5
- Hemodynamic improvement was noted in about 63% of the patients, and the overall survival rate was about 21%.
- There was no difference in time to successful AO between REBOA and open AO.
- There was no significant difference in mortality rates between the two techniques.
- However, there is no high-grade evidence demonstrating that REBOA improves outcomes or survival compared with the standard treatment of severe traumatic hemorrhage.4
- REBOA is not a definitive hemorrhage device, and it may be used to temporize patients at high risk of mortality from noncompressible torso hemorrhage.4 REBOA should only be used as part of a larger system of damage control resuscitation and definitive hemorrhage control. Most trauma centers use REBOA infrequently or not at all.4
Implications of REBOA for Anesthesiologists
Anesthesiologists may encounter trauma patients on or being considered for REBOA.3
Predeployment Phase
- Femoral arterial access (18 or 20G catheter) should be obtained as soon as possible.
- An upper extremity arterial line must be inserted as soon as possible to help monitor hemodynamics associated with balloon inflation.
- For zone I deployment, transesophageal echocardiography may aid in balloon placement.3
Hemodynamic Changes with REBOA Deployment
- Inflation of the balloon may result in a dramatic increase in mean arterial pressures. A sudden increase in afterload may cause left ventricular dilation, increased pulmonary artery pressures, and myocardial ischemia, especially in patients with coronary artery disease.3
- Notably, these responses are most apparent with more proximal zone I occlusion vs. zone III occlusion.
- Central hypertension may also lead to cerebral hyperperfusion, which is not ideal in the setting of head injuries.
- To avoid overresuscitation, systolic blood pressures must be maintained <100 mm Hg.3
REBOA Deflation and Management of Reperfusion
- Anticipated derangements while deflating the balloon include:3,4
- sudden decrease in circulating volume and left ventricular afterload;
- increase in lactic acid levels with resultant metabolic acidosis;
- release of inflammatory mediators, compliment, and reactive oxygen species;
- release of emboli into circulation;
- myocardial rhythm and contractility changes from electrolyte abnormalities, temperature changes, and acidosis; and
- ongoing hemorrhage.
- The negative effects of REBOA deflation are directly proportional to the duration of balloon inflation.5 Although the exact safe duration of inflation is not known, most studies recommend no more than 15-30 minutes of zone I ischemic time.4
- If the patient becomes critically unstable on balloon deflation, the balloon can be reinflated to allow for further optimization before deflation is reattempted. Additionally, partial deflation methods can be performed to allow for some perfusion. This could potentially lessen the consequences of prolonged ischemic time.
Complications of REBOA
- Ischemia from prolonged aortic occlusion may lead to fatal complications or spinal cord injury.4,6 Ischemia-reperfusion injury may lead to acute kidney injury and multisystem organ failure.
- Arterial access complications include arterial disruption, dissection, pseudoaneurysms, hematoma, and extremity ischemia.5
- Overinflation of the balloon may cause balloon rupture and iatrogenic aortic injury.4,6
- Unintentional inflation of the balloon in the iliac vessels can cause rupture or thrombosis.4,6
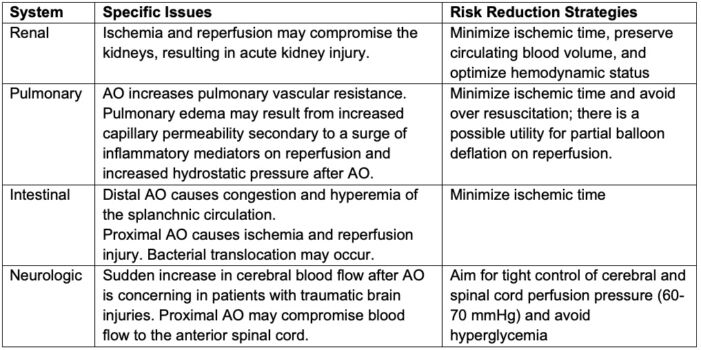
Table 3. Mitigation of Complications3
References
- Biffl WL, Fox CJ, Moore EE. The role of REBOA in the control of exsanguinating torso hemorrhage. J Trauma Acute Care Surg. 2015;78(5):1054-58. PubMed
- Stannard A, Eliason JL, Rasmussen TE. Resuscitative endovascular balloon occlusion of the aorta (REBOA) as an adjunct for hemorrhagic shock. J Trauma. 2011;71(6):1869-72. PubMed
- Sridhar S, Gumbert SD, Stephens C, et al. Resuscitative endovascular balloon occlusion of the aorta. Anesth Analg. 2017;125(3):884-90. PubMed
- Bulger EM, Perina DG, Qasim Z, et al. Clinical use of resuscitative endovascular balloon occlusion of the aorta (REBOA) in civilian trauma systems in the USA, 2019: a joint statement from the American College of Surgeons Committee on Trauma, the American College of Emergency Physicians, the National Association of Emergency Medical Services Physicians and the National Association of Emergency Medical Technicians. Trauma Surg Acute Care Open. 2019;4(1): e000376. PubMed
- DuBose JJ, Scalea TM, Brenner M, et al. The AAST prospective Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) registry. J Trauma Acute Care Surg. 2016;81(3):409-19. PubMed
- Ribeiro Jr MAF, Feng CYD, Nguyen ATM, et al. The complications associated with resuscitative endovascular balloon occlusion of the aorta (REBOA). World J Emerg Surg. 2018; 13:20. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.