Copy link
Radiation Safety for the Anesthesia Provider
Last updated: 10/08/2025
Key Points
- Anesthesia personnel are at risk of significant exposure to ionizing radiation in both operating room (OR) and non-OR anesthesia (NORA) settings, with the highest levels of exposure occurring during cardiac, endovascular, and neurointerventional procedures.1
- Ionizing radiation poses health risks, including cataracts and cancer, with the linear no-threshold model suggesting that any level of radiation exposure carries a risk.1
- Exposure risk is determined by time, total radiation intensity, distance, and the presence of shielding. The principal source of occupational exposure is scattered radiation, not direct exposure to the X-ray beam.1
- The eye is the most sensitive organ for radiation injury, and clinicians are strongly advised to use eye protection at all times.2
- Typical occupational doses for anesthesia personnel are low (<1 mSv/year). However, certain settings (e.g., electrophysiology and cardiac catheterization labs, neurointerventional suites) can significantly increase exposure to vulnerable organs, such as the lens.
Introduction
- X-rays are high-energy photons produced in X-ray tubes; they penetrate tissue and scatter in all directions. Scatter is the main source of anesthesia staff exposure.1
- Anesthesia personnel may be exposed to ionizing radiation through the use of X-ray machines, fluoroscopy units, O-arm computed tomography scanners, positron emission tomography scanners, or other radiation therapy modalities, such as the gamma knife.
- NORA has expanded significantly, placing anesthesia providers in procedural suites where radiation is used frequently (e.g., catheterization labs, electrophysiology suites, interventional radiology, hybrid ORs).
- Radiation intensity decreases with the square of the distance from the source (inverse square law). Doubling the distance from the source will reduce the radiation dose by a factor of four. Similarly, exposure at 4 feet is 1/16th of the exposure at 1 foot.
Radiation Terminology and Recommended Limits1,2
- Absorbed dose, measured in gray, indicates the amount of radiation absorbed by tissues.
- The equivalent dose, measured in sieverts (Sv), is calculated for individual organs by multiplying the mean absorbed dose in a tissue or organ by the radiation weighting factor.
- The effective dose, also measured in sieverts, is the sum of equivalent doses to all organs, each adjusted to account for the sensitivity of the organ to radiation, as determined by its tissue weighting factor (WT).
- Tissues such as red bone marrow, breast, colon, and lungs have a much higher WT than bone surface, brain, and skin.1,2
- The recommended dose limits for occupational exposure in medical imaging are listed in Table 1.
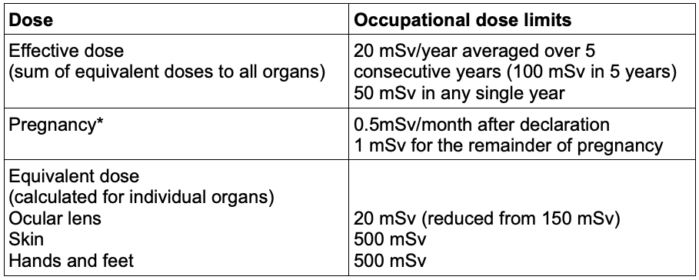
Table 1. Recommended dose limits for occupational exposure in medical imaging.3
Abbreviation: Sv, sieverts
Source: International Commission on Radiological Protection guidance for occupational exposure. Radiation Emergency Medical Management. U.S. Department of Health and Human Services. 2025. Link
*Pregnancy- In the United States, the NCRP recommends a 0.5 mSv equivalent dose monthly limit for the embryo/fetus once the pregnancy is declared. After a worker has declared her pregnancy, her working conditions should ensure that the additional radiation exposure does not exceed 1 mSv for the remainder of the pregnancy.
Documented Exposure Levels
- Exposure risk is determined by time, total radiation intensity, distance, and shielding.
- The average radiation exposure from medical and non-medical sources is listed in Table 1.
- The highest levels of exposure are during cardiac, endovascular, and neurointerventional procedures.1
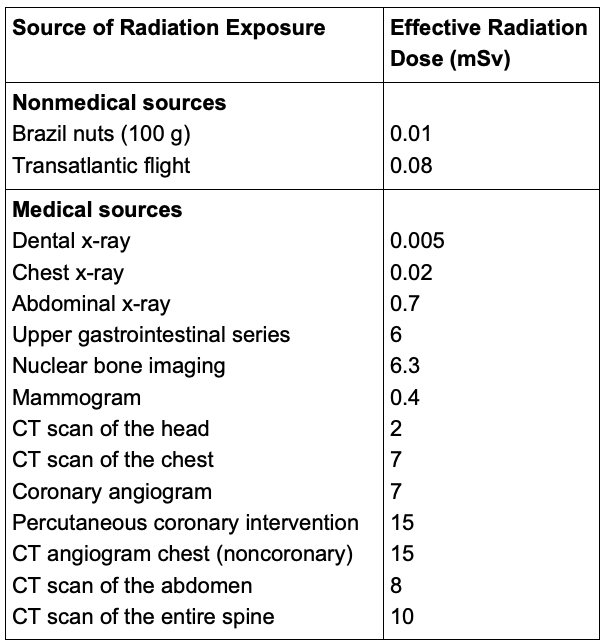
Table 2: Average radiation exposure from medical and nonmedical sources.
Abbreviation: CT, computed tomography.
Adapted from Lalabekyan B et al. Principles of radiation safety for anaesthetists. BJA Educ. 2025;5(5):181-190. Link and Fazel R, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med. 2009.
Sources of Radiation Exposure1
- The sources of radiation exposure for anesthesia providers are:
- Direct radiation (direct beam exposure)
- Scattered radiation
- Rarely, radiation exposure occurs from malfunctioning equipment.
- For anesthesia providers, the highest dose of radiation comes from scattered radiation (Figure 1), with the patient’s body being the primary source of this type of radiation.
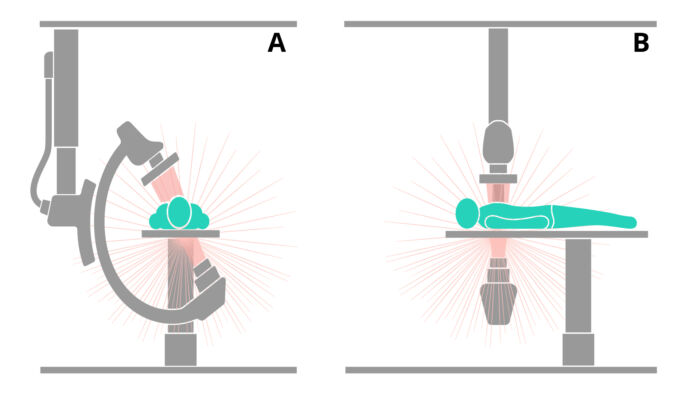
Figure 1. Scattered radiation from the patient’s body is highest on the side where the X-ray source is positioned. (A) Axial view, (B) sagittal view. Redrawn from Lalabekyan B, et al. Principles of radiation safety for anaesthetists. BJA Educ. 2025;5(5):181-190. Link
- Patient and technical factors influence the degree and amount of scattering.
- Patient factors include:
- Body thickness- obese patients tend to scatter more radiation since an increased radiation dose is required to achieve adequate tissue penetration.
- Complex procedures require higher radiation doses and result in more scattering.
- Technical factors include:
- Source of radiation: O-arm CT scanners generate twice as much radiation as C-arms.
- Position of the X-ray tube: The intensity of the radiation is higher on the side where the X-ray source is positioned. Certain C-arm views, such as the left anterior oblique view, the lateral view, and the caudal view, position the X-ray tubes close to the anesthesia provider.1
- Position of the image detector: Reducing the distance between the image detector and the patient’s body reduces the radiation exposure.
- Mode of exposure: Continuous fluoroscopy or digital subtraction angiography increases radiation exposure.
Effects of Ionizing Radiation1,2
- The effects of ionizing radiation can be categorized into two types: deterministic effects and stochastic effects.
- Deterministic effects occur when the absorbed dose exceeds a certain threshold, resulting in lens opacities, skin injuries (radiation burns), and infertility. Deterministic effects are proportional to the radiation energy delivered to the tissues.
- Tissues at the most significant risk include the ocular lens, thyroid, gonads, and bone marrow.
- The ocular lens is particularly susceptible to the effects of ionizing radiation, with increased rates of posterior subcapsular cataracts observed in survivors of the atomic bombs and individuals with occupational exposure.
- Stochastic effects refer to the development of cancer from direct DNA ionization or from the creation of hydroxyl radicals from X-ray interactions with water molecules.
- Stochastic effects can occur at any dose but are cumulative, where increasing the dose increases the risk of occurrence.
- There is no known “safe” dose below which an induced neoplasm does not occur.
- The lifetime risk of developing any form of cancer from radiation exposures (excluding bone and skin cancers) is 6.65% per sievert.1
- Radiation risks are higher during pregnancy. The risks are most significant during the first trimester, during organogenesis. The central nervous system is particularly sensitive to radiation within 8-25 weeks after conception.
- Ionizing radiation can cause infertility in both men and women of childbearing age.
Mitigating the Health Effects of Radiation Exposure1,2
- The anesthesia provider has little to no control over nonmodifiable factors such as the complexity or duration of the procedure, the dose of radiation required, and the type of radiation delivered to the patient.
- Factors that are modifiable and influence the occupational exposure can be broken down into 3 main categories:
- Distance: Because the intensity of scattered radiation is inversely proportional to the square of the distance from the source, the best protection is physical separation. A distance of at least 3 feet from the patient is recommended. Six feet of air provides protection equivalent to 9 inches of concrete or 2.5 mm of lead
- Time: Reduce the amount of time spent in close proximity to the source of radiation.
- Shielding: Personal protective equipment (PPE) should include protective aprons, thyroid shields, and lead glasses. Physical barriers (leaded glass shields) that shield from ionizing radiation may be used in cases with significant radiation exposure potential (cardiac catheterization and electrophysiology labs, neurointerventional suites, endovascular suites).
- Radiation physicists recommend the “as low as reasonably achievable” guiding principle for radiation exposure to both patients and practitioners. This includes the dose of radiation and the time of radiation exposure.1
- Personnel working frequently in high-risk fluoroscopy areas should wear personal dosimeters. Wear the device outside the apron on the collar.
Practical Recommendations
- Always wear a lead apron, thyroid collar, and leaded glasses. Lead aprons typically have a 0.5 mm lead equivalence. A thyroid collar of 0.5 mm lead equivalence can reduce the equivalent dose received by the thyroid by a factor of 12. Commercially available lead glasses with a lead equivalence of 0.75 mm can reduce the exposure by more than 85%.1
- Maintain a distance of ≥1-1.5 m from the radiation source when possible.
- Position yourself on the detector side (opposite the X-ray tube) and behind lead barriers.
- Declare if pregnant and use dosimetry consistently (two badges are required if pregnant). Wear a second device under the apron at the waist to measure deceleration.
Acute Radiation Exposure and Contamination
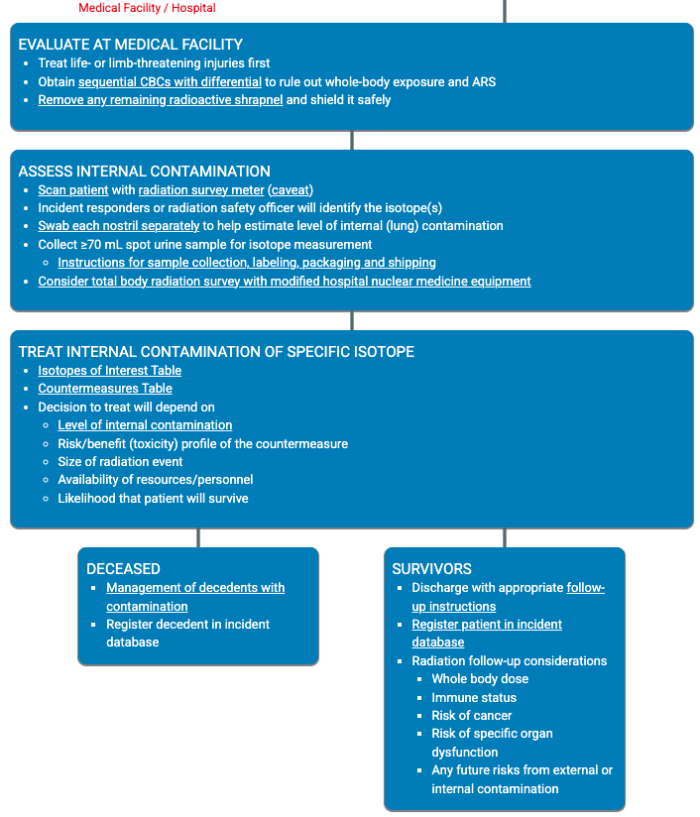
Figure 2. The management of Acute Radiation Exposure involves the following steps, as outlined specifically in Radiation Emergency Medical Management. Link
References
- Lalabekyan B, Rennie A, Luoma V. Principles of radiation safety for anaesthetists. BJA Educ. 2025;5(5):181-190. PubMed
- Dagal, A. Radiation safety for anesthesiologists. Current Opinion in Anaesthesiology. 2011;24(4):445-450. PubMed
- International Commission on Radiological Protection guidance for occupational exposure. Radiation Emergency Medical Management. U.S. Department of Health and Human Services. 2025. Link
- Treves ST, ed. Pediatric Nuclear Medicine and Molecular Imaging. 4th ed. New York, NY: Springer; 2014:645-658.
- Arii T, Uchino S, Kubo Y, et al. Radiation exposure to anaesthetists during endovascular procedures. Anaesthesia. 2014;70(1):47-50. PubMed
Other References
- International Commission on Radiological Protection (ICRP). The 2007 Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann ICRP. 2007;37(2-4):1-332 PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.