Copy link
Pulse Oximetry
Last updated: 10/08/2025
Key Points
- Pulse oximetry is a cornerstone of modern anesthetic monitoring, dramatically reducing perioperative morbidity and mortality by enabling continuous, non-invasive detection of hypoxemia.
- The pulse oximeter estimates oxygen saturation (SpO2) by spectrophotometry of pulsatile arterial blood, relying on differential absorption of red and infrared light by oxyhemoglobin and deoxyhemoglobin.
- Despite its ubiquity, several factors can limit the accuracy of pulse oximetry, including poor peripheral perfusion, the presence of abnormal hemoglobin, dark skin pigmentation, or interference from external factors (motion, nail polish, dyes, electrocautery).
Introduction
- The introduction of pulse oximetry into clinical practice represents one of the most transformative advances in perioperative patient safety. In the early 1980s, anesthesia-related mortality was estimated at approximately 1 in 10,000 anesthetics, but following the widespread implementation of standardized monitoring—most notably pulse oximetry and capnography—mortality declined to roughly 1 in 100,000 to 1 in 200,000 anesthetics, and in some series as low as 1 in 1,000,000.1
- The 1986 American Society of Anesthesiologists (ASA) monitoring standards, modeled on the Harvard Anesthesia Monitoring Standards, formally enshrined pulse oximetry as an essential component of safe anesthetic care.2 This change paralleled a marked reduction in adverse perioperative events and malpractice claims, underscoring the technology’s role as a “safety net” against unrecognized hypoxemia.1-3
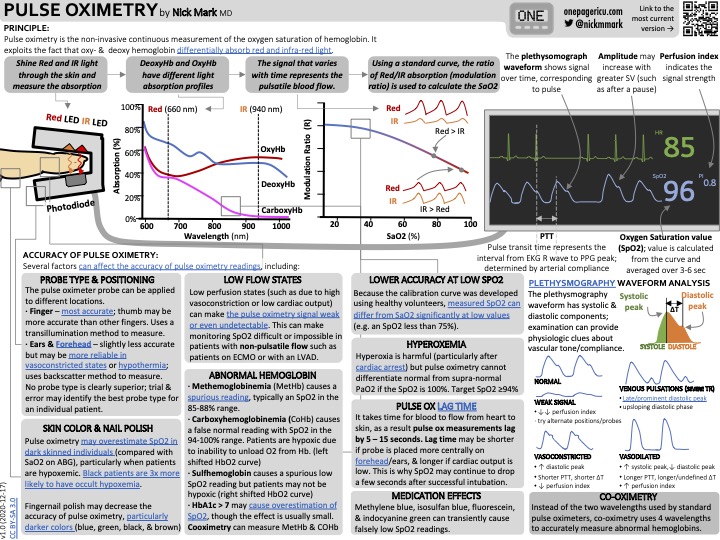
Operating Principles
- The pulse oximeter consists of two parts: 1) two light-emitting diodes of different wavelengths constantly emitting infrared and red light, and 2) the photodetector. The two parts are placed parallel to each other, with the sample site (such as the ear, finger, toe, etc.) positioned between them.4 This setup can be seen below in Figure 1.
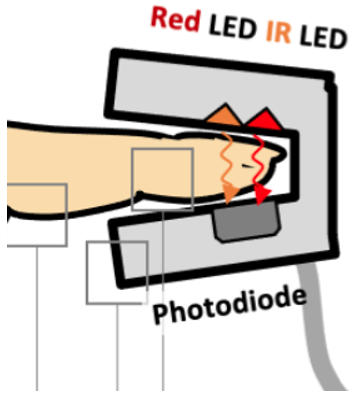
Figure 1. Pulse oximetry mechanics. Source: Mark N. Pulse Oximetry [infographic]. OnePager ICU. December 17, 2020. Link
- Hemoglobin is a protein present in erythrocytes. One hemoglobin molecule is made up of four polypeptide globin chains, each of which includes an iron ion. This iron molecule is the site of oxygen binding and unbinding. Thus, one hemoglobin molecule has the potential to bind and transport up to four oxygen molecules. The binding of oxygen to iron causes a change in molecular shape, altering how hemoglobin interacts with light. Hemoglobin bound with oxygen is brighter red in color; it absorbs more infrared light. Deoxyhemoglobin is darker red and absorbs more red light.
- Pulse oximetry works by spectrophotometry. The ratio of the two different light intensities sensed by the photodetector reflects the amount of infrared light absorbed compared to red light. This reflects the ratio of oxyhemoglobin to deoxyhemoglobin and is used to produce the SpO2 value.4
- Pulse oximeters continually estimate the arterial SpO2 of hemoglobin by using the predictable correlation that exists between the arterial SpO2 of hemoglobin as a percentage (SaO2) and the partial pressure of oxygen (PaO2). This predictable correlation corresponds with the steep part of the oxyhemoglobin dissociation curve, seen below in Figure 2. When the PaO2 is greater than 75mmHg, SaO2 values plateau, represented below in the curve. Thus, SpO2 is no longer a reliable indicator of PaO2.4
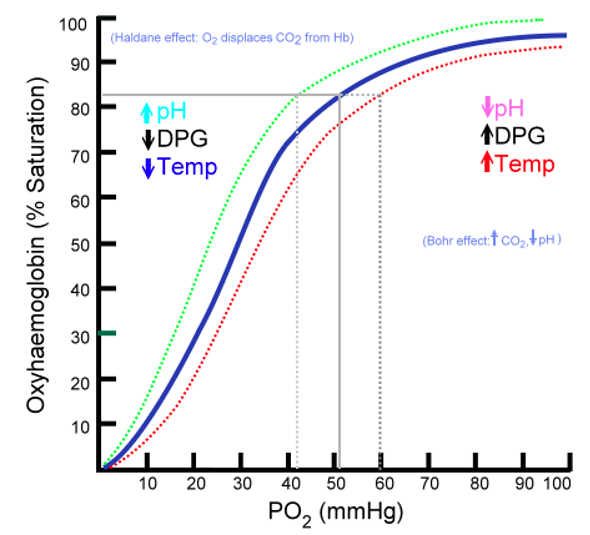
Figure 2. The oxyhaemoglobin dissociation curve. Source: Ratznium. Oxyhaemoglobin Dissociation Curve [graph]. Wikimedia Commons. 2006. Public domain. Link
- Pulse oximeters can detect variations in pulsatility to differentiate between arterial and venous signals.
Role in Anesthesia
- The ASA mandates the presence of a safety monitor that provides a quantitative assessment of arterial SpO2. Pulse oximetry fulfills this safety guideline in an accurate and continuous manner, and it is the standard of care throughout all anesthesia cases.4
- Pulse oximetry enables the non-invasive detection of hypoxemia. This is especially integral during anesthesia when clinical signs of hypoxemia may be masked.4
Role in Pediatric Anesthesia
- Pulse oximetry is particularly important in pediatric anesthesia. Infants have a high rate of oxygen consumption relative to their functional residual capacity, resulting in a much faster time to desaturation compared to the average-sized adult patient. Continuous oximetry shortens time-to-detection of hypoxemia during induction, airway instrumentation, and emergence.5
- Pulse oximetry better predicts endobronchial intubation than capnography in pediatric patients.6
- Given the non-invasive nature of pulse oximetry, most pediatric patients will tolerate the placement of the probe prior to the induction of anesthesia to monitor ventilation and oxygenation.4
Clinical Considerations
- When pulsations cannot be detected due to poor peripheral perfusion, such as in patients with hypothermia or hypotension, pulse oximeters may not accurately detect and calculate SpO2. This is also the case when patients are on cardiopulmonary bypass and blood flow is continuous instead of pulsatile.4
- Use of vasoconstricting medications may also cause a decrease in peripheral perfusion, resulting in decreased accuracy of SpO2 measurements.7
- The changes to the waveform produced by pulse oximetry during vasoconstriction are shown in Figure 3 below. When peripheral perfusion has dropped significantly or the probe is placed in a position that does not allow for the detection of arterial pulsations, the waveform may appear as a “Weak Signal” label, as shown below.

Figure 3. Pulse waveforms seen on pulse oximeters. Source: Pulse oximetry mechanics. Mark N. Pulse Oximetry [infographic]. OnePager ICU. December 17, 2020. Link
- In patients where there is concern about poor peripheral perfusion, placing the probe on the ear, specifically in the external auditory canal, may be more sensitive and yield more accurate measurements compared to the fingertip. The external ear canal experiences less vasoconstriction compared to the index finger during times of poor peripheral perfusion. Thus, SpO2 measurements maintain their accuracy, even with this decreased peripheral perfusion.7,8
- In patients with medium and dark skin pigmentation, categorized by Fitzpatrick skin tones III/VI and V/VII, respectively, there may be incidences of missed hypoxemia. This is further exaggerated when poor perfusion is present in patients of these skin tones.9 The Fitzpatrick scale is represented below in Figure 3.
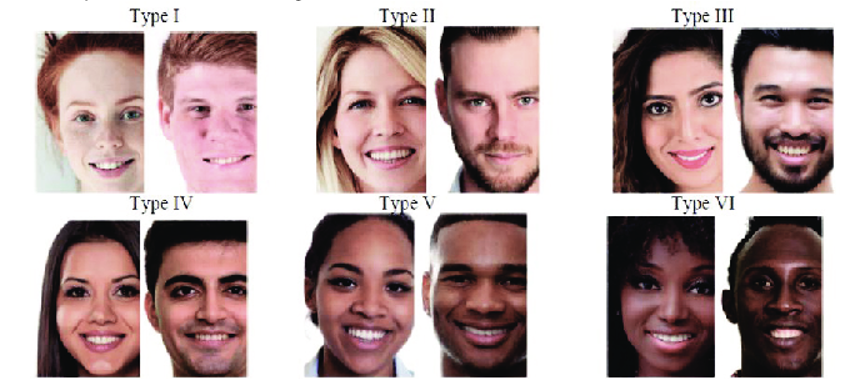
Figure 4. The Fitzpatrick scale. Source: Mathew, Joshua, Tian, et al. Fitzpatrick Skin Types [figure]. In: Description of the Six Skin Types Known as the Fitzpatrick Skin Type Classification. ResearchGate. Link
- Some case reports have documented burns caused by pulse oximetry cables conducting heat during magnetic resonance imaging (MRI) scans. The ASA requires the use of nonconductive, nonferromagnetic pulse oximeters, with special consideration given to the positioning of the cable in relation to the patient’s skin. This is especially applicable to the pediatric population, as many children require sedation with continuous SpO2 monitoring during MRI imaging.10
- Pulse oximeters cannot distinguish other types of hemoglobin. Thus, when other hemoglobin subtypes are present, such as carboxyhemoglobin and methemoglobin, the measured SpO2 may differ from the actual arterial saturation (SaO2), which is calculated using laboratory co-oximeters that use multiple wavelengths of light. Due to the optical properties of methemoglobin, pulse oximetry readings are falsely fixed near 85%, regardless of the true arterial SpO2. Arterial SpO2 are overestimated in the presence of carboxyhemoglobin, as it absorbs light very similarly to oxyhemoglobin.4 Please see the OA summary on methemoglobinemia for more details. Link
- Nail polish, motion artifact, some medications (such as methylene blue and indocyanine green), background noise, electrocautery, and stereotactic positioning systems are all factors that may be present during anesthesia care that may interfere with obtaining accurate SpO2 measurements.4
- SpO2 should not serve as a replacement for arterial blood gas measurements, and they should be considered when further information regarding oxygen supply and utilization is warranted.4
- SpO2 measurements do not necessarily reflect adequacy of ventilation. A substantial drop in PaO2 is necessary to cause a drop in SpO2 that is detectable by pulse oximeters. If a patient has been receiving supplemental oxygen, this SpO2 drop may not occur until the patient has been apneic for several minutes.
Other Sources
References
- Braz LG, Braz DG, Cruz DS, Fernandes LA, Módolo NS, Braz JR. Mortality in anesthesia: a systematic review. Clinics (Sao Paulo). 2009;64(10):999-1006. PubMed
- Eichhorn JH. ASA adopts basic monitoring standards. Anesthesia Patient Safety Foundation Newsletter. 1986;1(1):1-2. Link
- Taenzer AH, Pyke JB, McGrath SP, Blike GT. Impact of pulse oximetry surveillance on rescue events and intensive care unit transfers: a before-and-after concurrence study. Anesthesiology. 2010;112(2):282-287. PubMed
- Connor CW, Conley CM. Commonly Used Monitoring Techniques. In: Cullen BF, Stock MC, Ortega R, et al. Barash, Cullen, and Stoelting’s Clinical Anesthesia. 9th Edition. Place of publication not identified; Wolters Kluwer; 2023: 666-88.
- Kariuki E, Sutton C, Leone TA. Neonatal resuscitation: current evidence and guidelines. BJA Educ. 2021;21(12):479-485. PubMed
- Rolf, N. and Coté, C.J. Diagnosis of clinically unrecognized endobronchial intubation in paediatric anaesthesia: which is more sensitive, pulse oximetry or capnography? Pediatric Anesthesia; 2: 31-35. Link
- Poorzargar K, Pham C, Ariaratnam J, et al. Accuracy of pulse oximeters in measuring oxygen saturation in patients with poor peripheral perfusion: a systematic review. J Clin Monit Comput. 2022;36(4):961-973. PubMed
- Budidha K, Kyriacou PA. The human ear canal: investigation of its suitability for monitoring photoplethysmographs and arterial oxygen saturation. Physiol Meas. 2014;35(2):111-128. PubMed
- Gudelunas MK, Lipnick M, Hendrickson C, et al. Low Perfusion and Missed Diagnosis of Hypoxemia by Pulse Oximetry in Darkly Pigmented Skin: A Prospective Study. Anesth Analg. 2024;138(3):552-561. PubMed
- Practice advisory on anesthetic care for magnetic resonance imaging: an updated report by the American Society of Anesthesiologists task force on anesthetic care for magnetic resonance imaging. Anesthesiology. 2015;122(3):495-520. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.