Copy link
Pulmonary Ventilation: Physiology
Last updated: 08/07/2025
Key Points
- Ventilation is defined as the physiologic movement of air through the respiratory tract to facilitate gas exchange, which is essential for maintaining normal arterial oxygen, carbon dioxide, and pH levels.
- Central neural circuits in the brainstem automatically adjust ventilation to meet metabolic demands, with modulation from chemoreceptors that detect changes in arterial CO2, O2, and H+ concentration.
- The major factor that stimulates the medulla oblongata and pons to stimulate respiration is not oxygen concentration, but rather the concentration of CO2 in the blood.
- During general anesthesia, ventilatory control is significantly altered due to the depressant effects of most anesthetic agents on the central respiratory centers and chemoreceptor responsiveness, thus impairing spontaneous ventilation and blunting the normal ventilatory response to hypercapnia and hypoxemia.
Inspiration and Expiration
- Pulmonary ventilation includes two major steps: inspiration (air entering the lungs) and expiration (air leaving the lungs). A respiratory cycle is one sequence of inspiration and expiration.1
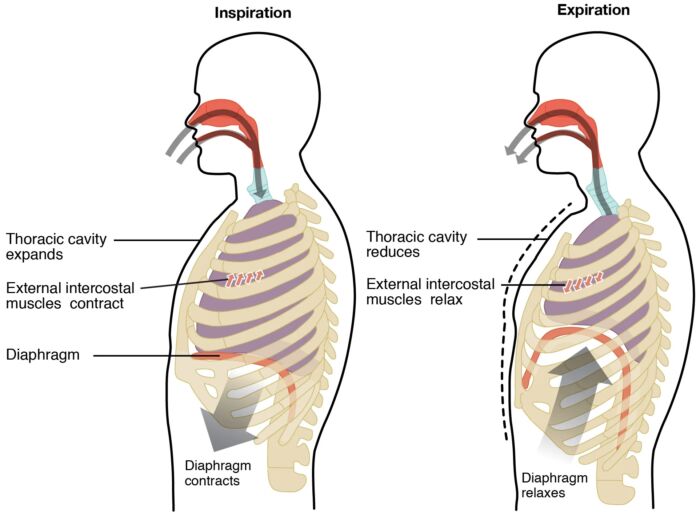
- Two muscle groups are used during inspiration: the diaphragm and the external intercostal muscles. When the diaphragm contracts, it moves inferiorly towards the abdominal cavity, creating more space in the thoracic cavity (Figure 1). Contraction of the external intercostal muscles moves the ribs upwards and outwards, causing the rib cage to expand.1
- Expansion of the thoracic cavity forces the lungs to stretch and expand as well. This increase in lung volume decreases intra-alveolar pressure, creating a pressure lower than the atmospheric pressure. This pressure gradient drives air into the lungs.
- While inspiration is an active process, expiration is passive. As the diaphragm and external intercostal muscles relax following inspiration, the elasticity of the lungs causes the lungs to recoil. As a result, the intrapulmonary pressure rises above atmospheric pressure, creating a pressure gradient that causes air to leave the lungs.
Types of Breathing
- Quiet breathing, also known as eupnea, occurs at rest and does not require the cognitive thought of the individual.1
- Deep breathing or diaphragmatic breathing requires the diaphragm to contract. Shallow breathing or costal breathing requires the intercostal muscles to contract.
- During forced breathing, also known as hyperpnea, other accessory muscles also contract in addition to the diaphragm and intercostal muscles.1
- During forced inspiration, neck muscles, including the scalene muscles, contract and lift the thoracic wall, increasing the lung volume.
- During forced expiration, the accessory muscles of the abdomen, including the obliques, contract, forcing abdominal organs upwards into the diaphragm.
Control of Ventilation
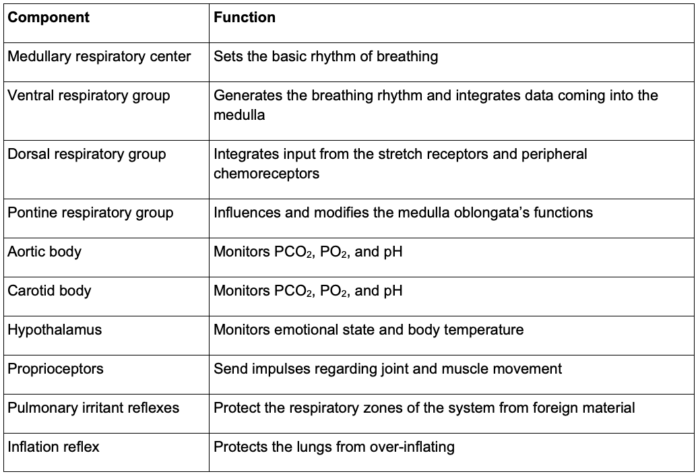
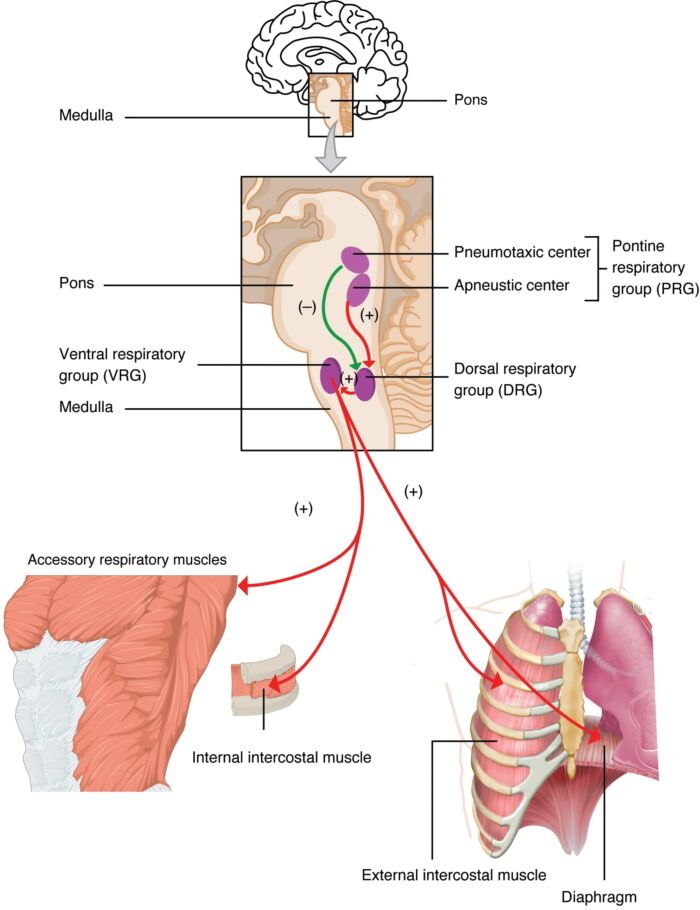
- The control of ventilation is a complex interplay of multiple regions of the brain that signal the muscles used in pulmonary ventilation (Table 1).1-3
Central Neural Respiratory Centers
- Ventilation is primarily controlled by neural mechanisms located in the medulla oblongata and the pons, which coordinate respiratory rhythm and integrate feedback from chemoreceptors and mechanoreceptors.2
- The medulla oblongata contains the dorsal respiratory group and the ventral respiratory group. The dorsal respiratory group is primarily active during inspiration and integrates sensory input from peripheral chemoreceptors and mechanoreceptors to modulate the basic inspiratory rhythm.2
- The ventral respiratory group contains both inspiratory and expiratory neurons and is utilized during forced breathing, contributing to both inspiration and forced expiration.2
- The pontine respiratory centers, which include the pneumotaxic and apneustic centers, modulate the medullary respiratory centers to adjust the rhythm and transition between inspiration and expiration.2
- The pneumotaxic center in the upper pons modulates the switch-off of inspiration, thereby limiting inspiratory duration and preventing overinflation of alveoli.2
Central Chemoreceptors
- Central chemoreceptors, located on the ventral surface of the medulla oblongata, primarily control the respiratory drive. They sense pH changes in the central nervous system caused by alterations in arterial CO2 levels.1-3 Carbon dioxide freely diffuses across the blood-brain barrier and forms hydrogen ions within the cerebrospinal fluid (CSF).
- Activated central chemoreceptors lead to activation of the medullary respiratory centers, including both the dorsal and ventral respiratory groups, leading to an increased rate and depth of ventilation, allowing for rapid homeostatic regulation of arterial carbon dioxide and pH.3 Therefore, arterial CO2 is the primary determinant of the respiratory drive.
- Increases in PaCO2 elevate CSF H+ concentration and activate the chemoreceptors. Conversely, decreases in CSH H+ concentration secondary to a reduction in PaCO2 reduce alveolar ventilation. This relationship between PaCO2 and minute ventilation is nearly linear. The PaCO2 at which ventilation is zero is known as the apneic threshold.3
Peripheral Chemoreceptors
- Peripheral chemoreceptors have a more rapid response to acute changes in blood gases and hypoxemia. They are located in the carotid bodies at the carotid bifurcation and the aortic bodies near the aortic arch, the former signaling the cranial nerve IX and the latter signaling cranial nerve X.3
- Peripheral chemoreceptors respond to decreased arterial oxygen partial pressure, increased arterial carbon dioxide partial pressure, and decreased arterial pH.3
- Activated peripheral chemoreceptors cause increased ventilation in response to significant drops in arterial oxygen partial pressure.3
Lung Receptors
- Lung stretch receptors are distributed in the smooth muscles of the airways. They are responsible for the inhibition of inspiration when the lung is inflated to excessive volumes (Hering-Breuer inflation reflex) and shortening of exhalation when the lung is deflated (deflation reflex).3 The impulses from these receptors are carried centrally by the vagus nerve.3
- Irritant receptors located in the airway epithelium respond to toxic stimuli by triggering bronchoconstriction, coughing, and an increase in respiration.
- Juxtapulmonary-capillary receptors are located within the alveolar walls and innervated by vagal fibers, which, when they are stimulated by increases in pulmonary interstitial pressure, such as those caused by pulmonary edema, embolism, or increased capillary blood volume, lead to reflex tachypnea characterized by rapid, shallow breathing.
Effects of Anesthesia on the Control of Ventilation
- Volatile anesthetics cause dose-dependent suppression of peripheral chemoreceptor responses to hypoxia and hypercapnia, abolishing these reflexes entirely at ≥1 minimum alveolar concentration, leaving breathing reliant on central chemoreceptors and brainstem control.3
- Volatile agents shift the CO₂ response curve rightward, raising the apneic threshold; therefore, if PaCO₂ falls, it leads to spontaneous ventilation ceasing during anesthesia.
- In spontaneously breathing patients, the additive suppression of respiratory drive increases the risk of postoperative hypoventilation and hypercarbia.
- Please see the OA summary Effects of Anesthesia on the Respiratory System for more details. Link
References
- Openstax. 22.3 The Process of Breathing - Anatomy and Physiology 2e | OpenStax. openstax.org. Link
- Brinkman JE, Toro F, Sharma S. Physiology, respiratory drive. In: StatPearls (Internet). Treasure Island, FL. StatPearls Publishing. 2025.
- Respiratory Physiology & Anesthesia. In: Butterworth IV JF, Mackey DC, Wasnick JD. eds. Morgan & Mikhail’s Clinical Anesthesiology, 7e. McGraw-Hill Education; 2022.
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.