Copy link
Pressure Support Ventilation
Last updated: 10/24/2025
Key Points
- Pressure support ventilation (PSV) delivers patient-triggered, flow-cycled pressure breaths that reduce respiratory muscle workload.
- PSV is particularly advantageous for weaning, with higher extubation success rates.
- PSV is contraindicated in patients with suppressed respiratory drive or obstructive lung disease.
Introduction
- PSV is a spontaneous mode of mechanical ventilation where each breath is initiated by the patient and assisted by a preset positive pressure delivered during inspiration. PSV can be used both invasively (via endotracheal tube) and non-invasively (via mask). Because patients control both the timing and volume of breaths, PSV provides a more physiologic and comfortable breathing pattern, compared to other ventilator modes, and is considered the ideal mode for weaning patients from mechanical ventilation once they have regained sufficient respiratory drive.1,2
- Unlike more traditional volume-controlled ventilation (VCV) or pressure-controlled ventilation (Figure 1), PSV does not deliver mandatory breaths or ensure a minimum minute ventilation. Instead, the patient controls the timing and rate of breaths, while the ventilator assists by delivering a fixed driving pressure.
- Several factors determine the inspiratory flow delivered by the ventilator:
- Driving pressure (set by a clinician)
- Airway resistance
- Lung compliance
- Patient’s inspiratory effort
- In PSV, breaths are flow-cycled, so the ventilator ends inspiratory support when the inspiratory flow decreases to a preset threshold (typically 25% of the peak inspiratory flow).3 During expiration, positive end-expiratory pressure (PEEP) is typically added to maintain alveolar recruitment, improve V/Q matching, and enhance oxygenation.4
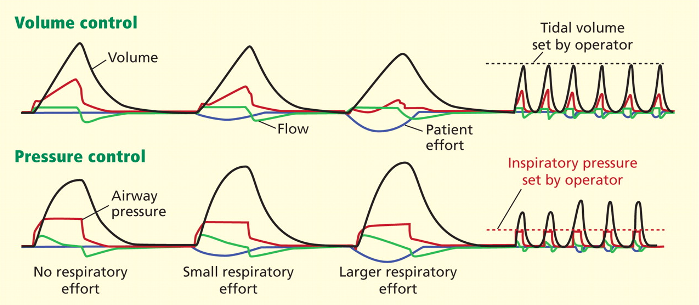
Figure 1. Volume control versus pressure control ventilation. The x-axis represents time. In pressure support ventilation, tidal volume is determined by the patient's inspiratory effort.5
Benefits of PSV
Benefits of PSV include:6,7,8
- Improves patient comfort and reduces the work of breathing
- Provides respiratory muscle reconditioning during weaning
- Reduces sedative requirements compared to controlled modes
- Facilitates synchrony and reduces dyssynchrony events such as double triggering
Uses and Contraindications
PSV is used in several scenarios:
- Delivers oxygen (O2) and ventilatory support in patients with hypoxemic, hypercapnic, or mixed respiratory failure
- Weaning and spontaneous breathing trials (SBTs): PSV supports spontaneous breathing while assessing readiness for extubation.
- Enhances carbon dioxide (CO2) elimination by increasing minute ventilation when necessary
- Improves ventilation-perfusion matching with PEEP, reduces shunt, and maintains alveolar patency during expiration
- Reduces the work of breathing and O2 consumption by assisting the respiratory muscles during inspiration
PSV is not appropriate for:
- Patients with depressed respiratory drive (e.g., sedative use, neurologic impairment) because PSV does not deliver mandatory breaths
- Conditions with elevated airway resistance (e.g., chronic obstructive pulmonary disease or asthma), where intrinsic PEEP and airway obstruction reduce the tidal volume delivery
- Central apnea or critical illness encephalopathy, where mandatory ventilation is required4,6,7
- Patients in shock or with low cardiac output states requiring full ventilatory support4
- These limitations occur primarily because PSV does not guarantee a minimum minute ventilation, placing the responsibility for adequate ventilation on the patient’s respiratory drive and mechanics.4,6,7
Advantages and Disadvantages
Advantages of PSV
- Earlier liberation from mechanical ventilation compared to VCV by delivering lower peak airway pressures, reducing the risk of barotrauma2
- The patient’s spontaneous breathing effort is supported, improving patient-ventilator synchrony (Figure 2).7
- Facilitates respiratory muscle reconditioning by allowing patients to sustain spontaneous breathing efforts with supportive assistance7
- The flow-cycled breath termination, tailored to patient effort, minimizes dyssynchrony events such as delayed cycling or double triggering.3
- Automatic tube compensation can offset additional resistance imposed by the endotracheal tube.4
Disadvantages of PSV
- PSV does not guarantee consistent tidal volumes or minute ventilation (Figure 2), so it is unsuitable for patients lacking adequate respiratory drive (apnea, sedation).4
- It is associated with poorer sleep quality than assist-control ventilation modes due to increased sleep fragmentation.3,4
- Increased risk of ventilator-induced lung injury and atelectasis at high pressure support levels (>20 cm H2O)1
- Requires close monitoring to detect patient dyssynchrony and inadequate ventilation8
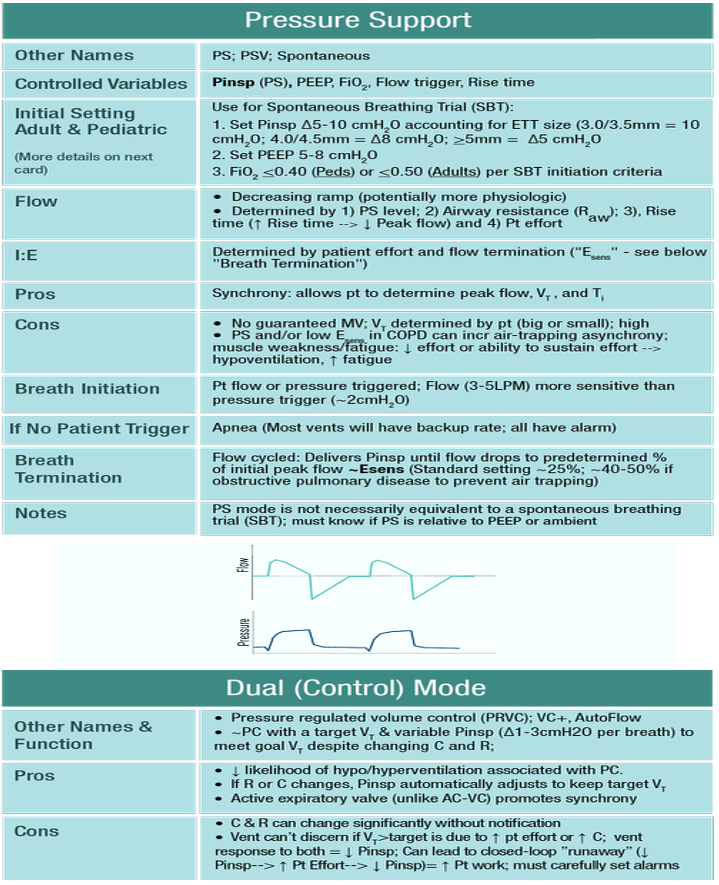
Figure 2. Overview, advantages, and disadvantages of PSV.9
Weaning Strategy
PSV is important in weaning due to its ability to provide graduated support, allowing patients to gradually regain respiratory muscle strength.
- Readiness Testing for weaning is assessed through clinical criteria:10
- Improved underlying disease, stable hemodynamics
- Adequate oxygenation (FiO2 ≤ 0.4, PEEP ≤ 5 cm H2O)
- Intact respiratory drive
- SBTs at preferred low-level PSV (5–8 cm H2O, with PEEP 5 cm H2O)
- PSV offsets the work of breathing imposed by the endotracheal tube and circuit, improving accurate assessment of respiratory ability.3,7,10
- Categories:
- Simple wean: Pass first SBT
- Difficult wean: Fail initially, succeed in 3-7 days
- Prolonged wean: Require more than 7 days and multiple SBTs
- Automated Weaning
- Automated, computer-driven PSV weaning protocols have emerged, dynamically adjusting pressure support based on respiratory rate, tidal volume, and exhaled CO2.10
- Evidence shows similar MV duration compared to clinician-driven weaning, but adoption is limited by variability in systems10
- PSV vs. Other Methods
- Randomized trials show PSV improves weaning success compared to T-piece and synchronized intermittent mandatory ventilation trials.6
- Meta-analyses suggest no clear superiority between SBT-based protocols and gradual PSV, though both outperform usual care.10
- PSV-SBTs are likely superior to continuous positive airway pressure (CPAP)-SBTs, especially in obstructive lung disease, as CPAP may cause mask fatigue.10
- PSV’s patient-driven support promotes better synchrony and reduces respiratory muscle fatigue, key to successful weaning.4
References
- Jubran A. Weaning from mechanical ventilation: What have we learned? Respir Care. 2017;62(9):1386-94. PubMed
- MacIntyre NR. Respiratory function during pressure support ventilation. Chest. 1986;89(5):677-83. PubMed
- Tobin MJ, Laghi F, Jubran A. Ventilatory failure, ventilator support, and ventilator weaning. Compr Physiol. 2012;2(4):2871-2921. PubMed
- Abramovitz A, Sung S. Pressure support ventilation. In: StatPearls (Internet). Treasure Island, FL: StatPearls Publishing; 2023. Accessed September 23, 2025. PubMed
- Pressure-regulated volume control graphic.jpg. (2025, May 1). Wikimedia Commons. Retrieved October 10, 2025, from Wikimedia Link
- Brochard L, Pluskwa F, Lemaire F. Weaning from mechanical ventilation. Eur Respir J. 1994;7(2):395-401. PubMed
- Brochard L, Rauss A, Benito S, et al. Comparison of three methods of gradual withdrawal from ventilatory support during weaning from mechanical ventilation. Am J Respir Crit Care Med. 1994;150(4):896-903. PubMed
- Parthasarathy S, Tobin MJ. Effect of ventilator mode on sleep quality in critically ill patients. Am J Respir Crit Care Med. 2002;166(11):1423-1429. PubMed
- OpenCriticalCare. (n.d.). Pressure support (PS) ventilation mode [Image]. In OpenCriticalCare. Retrieved October 14, 2025, from OpenCriticalCare Link
- Epstein S, Walkey A. In: UptoDate. Initial weaning strategy in mechanically ventilated adults: Post T, ed. UpToDate; 2025. Accessed September 23, 2025. Link
- Rose L, Presneill JJ, Johnston L, Cade JF, Fraser JF. Automated versus non-automated weaning for reducing the duration of mechanical ventilation for critically ill adults and children. Cochrane Database Syst Rev. 2015;2015(6):CD009235. PubMed
- Ely EW, Baker AM, Dunagan DP, et al. Effect on the duration of mechanical ventilation of identifying patients capable of breathing spontaneously. N Engl J Med. 1996;335(25):1864-69. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.