Copy link
Posttonsillectomy Hemorrhage
Last updated: 02/01/2023
Key Points
- Post tonsillectomy hemorrhage (PTH) is a surgical emergency following a tonsillectomy or adenotonsillectomy.
- Patients with PTH may be significantly hypovolemic and anemic and are at risk for hemodynamic instability under anesthesia.
- PTH increases the risk for difficult intubation, perioperative hypoxemia, and aspiration.
Introduction
- PTH is a surgical complication following a tonsillectomy with or without adenoidectomy with a mean incidence of 4.5%.1
- PTH may present as early “primary” hemorrhage or late “secondary” hemorrhage (Figure 1).
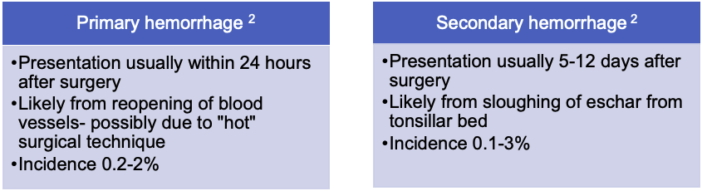
Figure 1. Primary vs. secondary PTH
- Risk factors for PTH include age older than 5 years, recurrent tonsillitis, certain surgical techniques.2,3 A “hot” electrosurgical, cautery dissection technique is more likely to cause PTH than “cold” ligation of vessels and use of a knife, scissors, or snare technique. There is evidence that an “intracapsular” tonsillectomy technique may reduce the incidence of PTH.3
- Most studies indicate no statistically significant increase in the risk of PTH with perioperative NSAIDs use (except for aspirin), although this remains a topic of ongoing research.2,3
Preoperative Diagnosis and Resuscitation
- Posttonsillectomy hemorrhage may present as frank bleeding or hematemesis from swallowed blood. It is hard to quantify the amount of bleeding as most of the blood is swallowed. Acute clinical decompensation will not present until 40% of blood volume is lost.1 Early hematocrit and BP may be stable due to clinical compensation.4
- A thorough preoperative evaluation is crucial to estimate the extent of a patient’s hypovolemia (Figure 2).
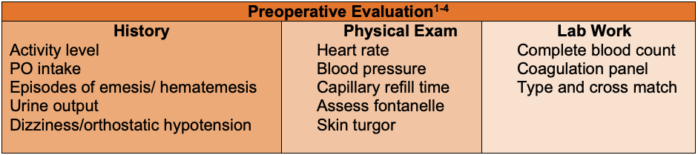
Figure 2. Preoperative work-up for PTH
- As PTH is more commonly a venous ooze and not an arterial bleed, it is important to resuscitate before rushing to the operating room (OR). Preoperative IV access may be challenging, so one should consider the use of ultrasound.1
- Preoperative management includes volume resuscitation with isotonic crystalloids (e.g., lactated Ringer’s, Plasmalyte, or normal saline) 10-20 mL/kg over 5 to 20 mins and then repeat as necessary. Colloid may also be indicated.4
- It is rare for PTH patients to require a blood transfusion, but it should be considered in hemorrhagic shock. Similarly, it is uncommon for patients to have a coagulation disorder, but evaluation and replacement with specific products should be considered.1-4
- Use of tranexamic acid, either nebulized preoperatively or given IV in the OR, is being evaluated in ongoing studies.1
Anesthetic Considerations and Management
- Most patients with PTH are taken to the OR to achieve surgical hemostasis. The anesthesia team needs to be prepared for the following risks:
- increased risk of difficult intubation secondary to postoperative swelling and blood in the oropharynx or airway;
- increased risk of pulmonary aspiration secondary to swallowed blood;
- hemodynamic instability: Patients initially have catecholamine driven vasoconstriction. After induction, drug-induced vasodilation can lead to significant hypotension if not adequately resuscitated.
- A single-center retrospective review of 475 children with posttonsillectomy hemorrhage reported the following incidence of adverse events (Table 1).2
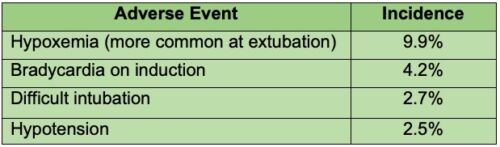
Table 1. Incidence of adverse events during anesthesia for PTH
Preoperative Set-Up1,4
- Availability should be ensured of 2 functioning laryngoscope handles and blades, cuffed ETTs in varying sizes with stylet, a McGill’s forceps for removal of large clots, and 2 working suctions.
- The presence of the ENT surgeon should be requested in the OR during induction.
Induction
- Preoxygenation should be considered in the left lateral decubitus position with the head down if the patient tolerates it.2,4
- A rapid sequence induction (RSI) should be performed with cricoid pressure using a reduced dose of an induction agent (propofol, ketamine, or etomidate) and succinylcholine or rocuronium; if rocuronium is used, ensure sugammadex is available in the event of a difficult airway situation.4
- Some studies have shown that a modified RSI with gentle ventilation using pressures less than 12 cmH2O may help to mitigate the hypoxemia during intubation. Similarly apneic oxygenation via nasal cannula may be helpful.1
- Induction drugs should be dosed judiciously to maintain hemodynamic instability.
Maintenance of Anesthesia1-4
- FiO2 should be reduced to decrease the risk of an airway fire during the use of electrocautery.
- This is usually a short surgical case; short-acting medications should be used and be prepared to facilitate early emergence.
- Multimodal analgesia should be considered with short-acting opioid (fentanyl) and acetaminophen.
Emergence from Anesthesia1-4
- The stomach should be emptied with a large bore orogastric tube; although this does not guarantee an empty stomach.
- Paralysis should be reversed and antiemetics administered.
- Patients should be extubated when they are fully awake and able to control their airway reflexes.
- Patients should be admitted for overnight monitoring and be provided analgesia with acetaminophen and low dose fentanyl.
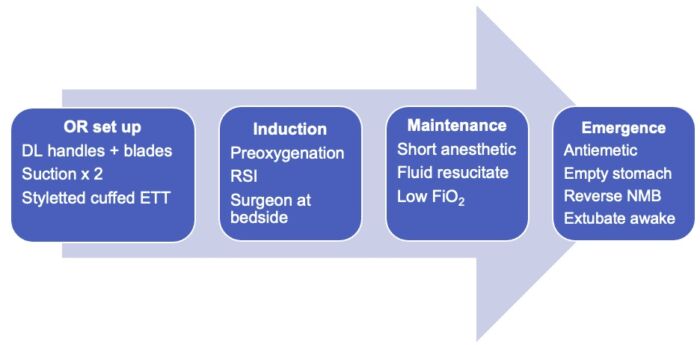
Figure 3. Summary of anesthesia set up and management for PTH
References
- Lee AC, Haché M. Pediatric Anesthesia Management for Post-Tonsillectomy Bleed: Current Status and Future Directions. Int J Gen Med. 2022; 15:63-69. PubMed
- Fields RG, Gencorelli FJ, Litman RS. Anesthetic management of the pediatric bleeding tonsil. Paediatr Anaesth. 2010;20(11):982-86. PubMed
- Oomen KP, Modi VK, Stewart MG. Evidence-based practice: pediatric tonsillectomy. Otolaryngol Clin North Am 2012 Oct;45(5):1071-81. PubMed
- Hannallah RS., Brown KA, Verghese ST. Otorhinolaryngologic Procedures. Cote, Lerman and Todres, editors. A Practice of Anesthesia for Infants and Children. 6th edition. Philadelphia. Elsevier. 2019: 772-774.
Other References
- Chatterjee D. Posttonsillectomy hemorrhage. OpenAnesthesia. Published May 2018. Accessed February 2, 2023. Posttonsillectomy Hemorrhage
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.