Copy link
Perioperative Culture of Safety
Last updated: 10/23/2025
Key Points
- A culture of safety in healthcare is a shared commitment by leadership, management, and health professionals to prioritize safety in all care delivery aspects.
- It emphasizes psychological safety, teamwork/leadership, continuous learning, accountability, a non-punitive approach to errors, and patient/family involvement.
- Modern safety culture recognizes inclusion, interprofessional trust, power dynamics, and respect as central to patient outcomes and workforce sustainability.
Introduction
- A culture of safety refers to the shared values, norms, attitudes, and behaviors across an organization that prioritize safety above all.
- In high-risk, complex perioperative care, it shapes staff perceptions of safety, reporting behaviors, and protocol adherence.
- The core components of an inclusive safe culture are detailed in Table 1.
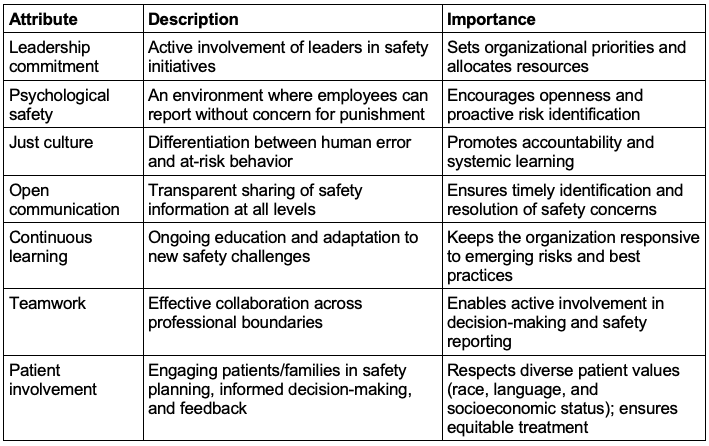
Table 1. Core components of a culture of safety.1-2
- The importance of a culture of safety is manifold:1-2
- Reduces harm and preventable errors like wrong-site surgeries and infections
- Improves team performance and trust, critical in OR and ICU settings
- Enhances patient trust, satisfaction, and adherence to treatment
- Strengthens staff engagement, resilience, and retention by valuing safety over productivity
- A modern safety culture focuses on patients and staff and emphasizes the following:1-2
- Establishing an inclusive safety culture
- Building interprofessional trust
- Demonstrating respect
- Deconstructing hierarchies and power dynamics
Establishing an Inclusive Safety Culture
- In addition to the core components, an inclusive safety culture:2,4-5
- prevents physical, psychological, and moral harm to patients and staff;
- equitably learns from errors and near misses without blame (Just Culture);
- includes all voices, especially marginalized ones, in decisions that affect care and work;
- fosters cultural competence;
- applies human factors and high-reliability principles; and
- measures and acts on disparities to close equity gaps in outcomes and experiences.
- Why it matters:2,4-5
- Patients: Safer care, fewer adverse events, reduced inequities, better adherence, and satisfaction
- Colleagues: Lower burnout, higher retention, earlier escalation of concerns, improved teamwork
- Organization: Greater reliability, compliance, reputation, efficient resource use, resilient learning
- Barriers to an inclusive safety culture and strategies to mitigate them are discussed in Tables 2 and 3, respectively.
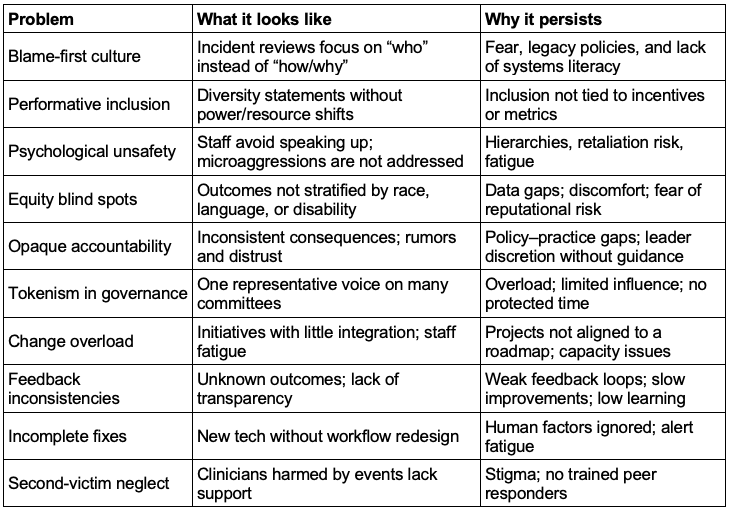
Table 2. Barriers to an inclusive safety culture2,4-5
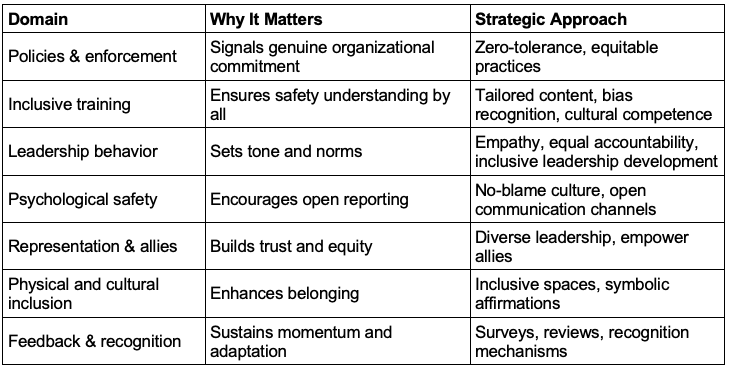
Table 3. Creating an inclusive safety culture2,4-5
Building Interprofessional Trust
- Interprofessional trust is defined as confidence and mutual respect among healthcare professionals, ensuring competent, open communication and patient safety prioritization.1-2
- The significance of interprofessional trust includes the following:1,2,6
- Enhanced error prevention and response – “stop the line” mindset
- Improved communication, teamwork, and care coordination
- Better clinical outcomes, morale, and patient satisfaction
- Barriers to interprofessional trust and strategies for improving that trust are discussed in Table 4.
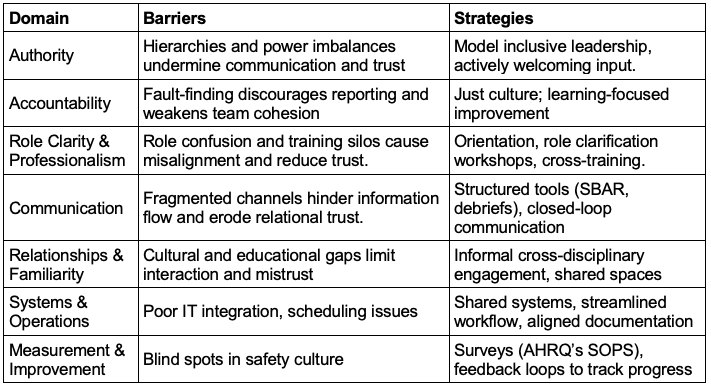
Table 4. Building trust – Barriers and solution1-2,6
Demonstrating Respect
- Respect within a safety culture involves treating every individual (patients, colleagues, and staff) with dignity, civility, and consideration, regardless of their role or status.1-2,7-8
- It is demonstrated through active listening, transparent communication, acknowledging concerns, and upholding a formal code of conduct.
- The significance of respect is as follows:1-2
- Fosters safety and performance
- Promotes open communication
- Improves team morale and retention
- Enhances patient satisfaction and experience
- Challenges to demonstrating respect and the strategies to cultivate respect are listed in Table 5.
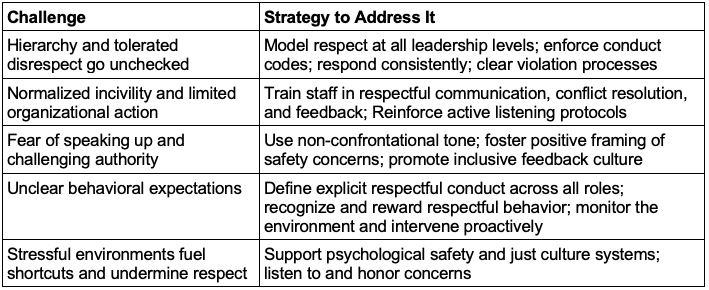
Table 5. Demonstrating respect – Challenges and strategies to overcome them.1-2,7-8
Deconstructing Hierarchies and Power Dynamics
- Deconstructing hierarchy consists of the following:1-2,8
- Actively lowering steep chains of command and rigid authority gradients that hinder open communication, error reporting, and mutual accountability
- Valuing input from everyone on the team, regardless of rank, and encouraging shared responsibility for patient safety
- The significance of deconstructing hierarchy is as follows:1-2,8
- Improves patient outcomes: lowers mortality; heightens patient satisfaction
- Mitigates siloed thinking: improves interdisciplinary collaboration; reduces compromised care
- Builds psychological safety: bolsters early detection and response to deterioration
- Flattens communication channels: encourages open dialogue across levels
- Empower frontline workers: their proximity to risk gives them critical insight
- Model humility and vulnerability: leaders admitting mistakes foster trust
- Barriers to deconstructing hierarchies and strategies to mitigate them are addressed in Table 6.
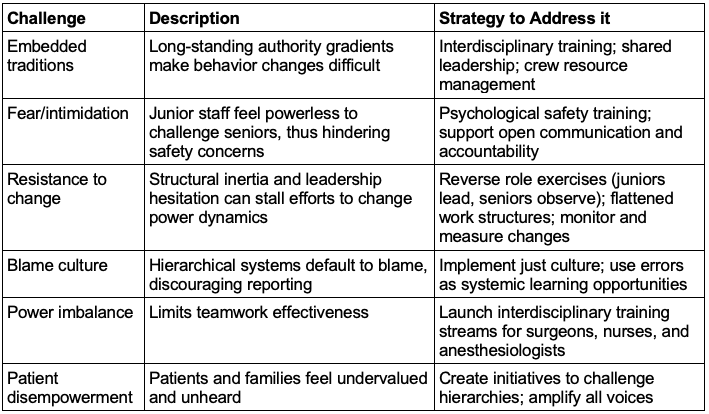
Table 6. Barriers and strategies associated with deconstructing hierarchies.1-2,8
References
- Frankel A, Haraden C, Federico F, Lenoci-Edwards J. A framework for safe, reliable, and effective care. Cambridge, MA: Institute for Healthcare Improvement and Safe & Reliable Healthcare; 2017. Link
- American College of Healthcare Executives, IHI/NPSF Lucian Leape Institute. Leading a culture of safety: A blueprint for success. Boston, MA: American College of Healthcare Executives and Institute for Healthcare Improvement; 2017. Link
- Bass EJ, Bat-Zion H. Perioperative environment safety culture: A scoping review addressing safety culture, climate, enacting behaviors, and enabling factors. Anesthesiology clinics 2023; 41(4): 75573. Link
- Rosenkranz, Kari M., et al. Diversity, equity and inclusion in medicine: why it matters and how do we achieve it?. Journal of Surgical Education 2021; 78(4): 1058-65. Link
- Gill GK, McNally MJ, Berman V. Effective diversity, equity, and inclusion practices. Healthcare Management Forum. 2018; 31(5):196-9. PubMed
- Sillero A, Buil N. Enhancing interprofessional collaboration in perioperative setting from the qualitative perspectives of physicians and nurses. Int J Environ Res Public Health. 2021;18(20):10775. PubMed
- Leape, Lucian L., et al. Perspective: a culture of respect, part 2: creating a culture of respect. Academic Medicine 2012; 87(7): 853-58. Link
- Pattni N, Arzola C, Malavade A, et al. Challenging authority and speaking up in the operating room environment: a narrative synthesis. Br J Anaesth. 2019;122(2): 233-44. PubMed
Other References
- National Steering Committee for Patient Safety. Safer Together: A National Action Plan to Advance Patient Safety. Boston, MA: Institute for Healthcare Improvement; 2020. Accessed July 21, 2025. Link
- Statement on Safety Culture American Society of Anesthesiologists. Committee on Patient Safety and Education. Oct 26, 2022. Updated Oct 18, 2023. Link
- APSF. Domino KB: Racial and Ethnic Disparities in Perioperative Patient Safety” Created 2022. Accessed October 23, 2025 Link
- APSF. Cooper JB: Respectful, Trusting Relationships Are Essential for Patient Safety, Especially the Surgeon-Anesthesiologist Dyad. Created 2019. Accessed October 23, 2025 Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.