Copy link
Pediatric Video Laryngoscopy
Last updated: 01/27/2023
Key Points
- Video laryngoscopy (VL) is associated with higher first-pass success rates and lower complication rates when used for tracheal intubation in infants.1
- In children who are difficult to intubate, VL has much higher success rates than direct laryngoscopy (DL).2
- VL also has other benefits that are harder to measure, such as allowing trainers to see where the blade is positioned, identify anatomical structures that a trainee may not recognize, and have an objective view of the tube passing through the cords.
Introduction
DL has been the standard technique used to intubate infants and children for decades. It is a safe and efficient technique, but in about 1% of children (possibly more in infants), tracheal intubation using DL is difficult. In approximately 20% of cases that are difficult to intubate, the problems were not anticipated.
Complications associated with difficulties performing tracheal intubation can be life-threatening. Data from the Pediatric Difficult Intubation Registry (PeDIR) shows that hypoxemia occurred in nearly 9% of cases, with hypoxic cardiac arrest occurring in nearly 2%.3 Complications during intubation are associated with the number of attempts at intubation.
It should be noted that there are multiple different designs of video laryngoscopes and that they are often grouped together and inappropriately treated as a single group of devices within the medical literature. One way of categorizing them is to group them into devices with traditional DL blades combined with a video camera at the tip of the blade (standard blade VL) and blades that are curved at an acute angle that allow the device to follow the natural curve of the airway (often called hyperangulated blades) (Table 1 and Figure 1). The technique for using each of these devices is different, and they should not be considered as a single entity.
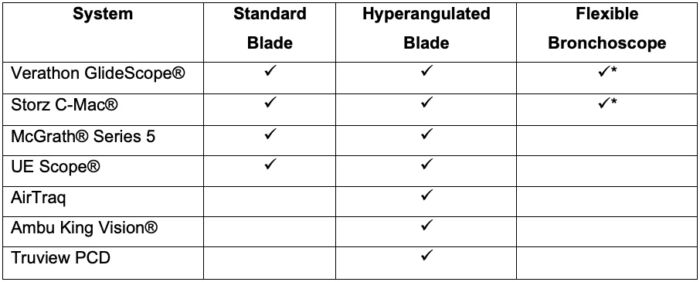
Table 1. Common pediatric VL systems (not a comprehensive list). * Flexible bronchoscope can be used simultaneously with the VL device.

Figure 1. Common direct laryngoscopy and video laryngoscopy blades. From left to right: Miller 1 DL blade, Storz C-Mac® Miller 1 VL blade, Truview EVO, McGrath® series 5 Mac 3 blade, King Vision® VL blade, Storz C-Mac® Pedi-D blade, GlideScope® Cobalt AVL sheath, GlideScope® Spectrum blade. Reproduced with permission from: Peyton J, et al. A comparison of videolaryngoscopy using standard blades or non-standard blades in children in the Paediatric Difficult Intubation Registry. Br J Anaesth. 2021;126(1):331-9.4
The use of VL systems that have standard blades allows DL to be performed with modern equipment. With these devices, DL can be performed as it would be using a traditional device, but there is also the advantage of being able to use the video view to aid the intubation (video-assisted DL) or switch entirely to the indirect view seen on the video screen and intubate using VL alone. These three techniques can be used in a single laryngoscopy attempt. Some manufacturers also make flexible bronchoscopes that can be used with the VL systems, which enable users to switch between advanced airway techniques rapidly or use them in combination if needed
Data Supporting VL
- The Video Laryngoscopy in Small Infants (VISI) trial showed that when standard blade (Miller) VL was used in children weighing ≤ 6.5 kg, there were higher success rates and fewer complications (Figure 2).1
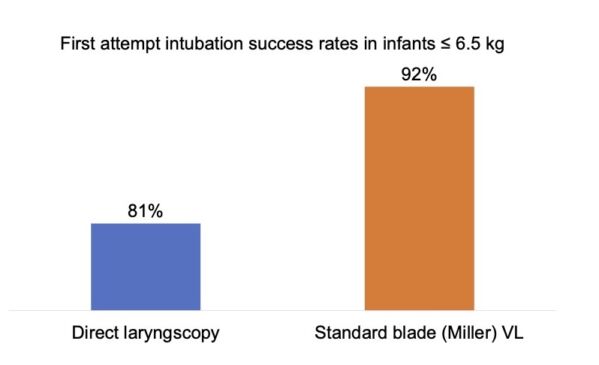
Figure 2. First attempt intubation success rates in infants ≤ 6.5 kg in the VISI trial.1
- Data from the PeDIR showed that GlideScope® VL is associated with a much higher success rate than DL in children who are difficult to intubate (Figure 3).2
- PeDIR data also showed a difference in success rates when VL is used in small infants who are difficult to intubate, with higher success rates seen with standard blade VL.4
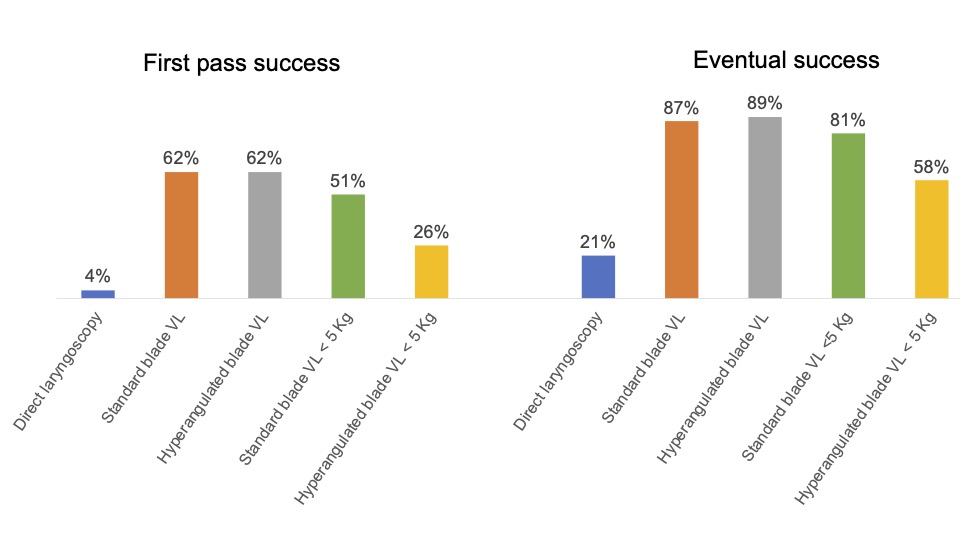
Figure 3. First pass and eventual success rates of direct laryngoscopy vs. standard blade VL vs. hyperangulated blade VL in the Pediatric Difficult Intubation Registry.2,4
Problems with VL and How to Avoid Them
Trauma to Oropharynx or Larynx
- The clinician should watch the blade as it is inserted, not the screen, and switch to looking at the screen only when the tip of the blade can no longer be seen.
- The clinician should watch the tracheal tube as it is inserted and switch to looking at the screen only when the tip of the tube cannot be seen. It should appear on the screen immediately.
Poor View of the Glottis
- Positioning the head in a neutral position may help
- Insert the blade into the midline over the base of the tongue
- Identify midline anatomical structures and aim to place the tip of the blade into the vallecula
- Lift the jaw upwards with the blade and keep the epiglottis and vocal cords in view
- External laryngeal manipulation may help
- If the tongue is blocking the video camera, sweeping it to the left with the blade may help (analogous to performing traditional DL).
- If blood or secretions are blocking the camera, placing a suction catheter to allow continuous suction may help.
View/tube discrepancy is when a good view is available but the patient cannot be intubated. This is more common with hyperangulated blades.
- Use a stylet to create a curve similar to that of the blade
- Assess why there is difficulty; usually this is due to the angle the tube is approaching the glottis which means its tip is hitting the superior anterior portion of the larynx.
- In patients with small mouths, or neonates and infants, the physician should consider moving the blade over to the left side of the mouth once a view of the larynx is available to create more space for the tube to be manipulated.
- The physician should ensure that the tip of the blade is not too close to the larynx to create space for tube manipulation. They should slowly pull the blade backwards while maintaining a view of the glottis. The blade should not be placed under the epiglottis as this can limit the space required for directing the tube.
- The styleted tube should be inserted from the right side of the mouth at an angle to the laryngoscope and slowly rotated to the midline once in the mouth.
- If the styleted tube is abutting the larynx and not going through it, the physician should try to pull back the stylet. Bending the tube against its natural curve when placing the stylet or creating a spiral shape may encourage the tip of the tube to move forward in a straight line or slightly downwards when the stylet is removed, which can help it drop into the larynx.
- A combination technique should be used with a flexible bronchoscope as a steerable stylet that can be manipulated in multiple directions.
Summary
When compared to DL, the use of VL for tracheal intubation in pediatric patients is associated with higher success rates and fewer complications in infants with normal airways and in infants and children who are difficult to intubate.
References
- Garcia-Marcinkiewicz AG, Kovatsis PG, Hunyady AI, et al. First-attempt success rate of video laryngoscopy in small infants (VISI): a multicentre, randomised controlled trial. Lancet. 2020;396(10266):1905-13. PubMed
- Park R, Peyton JM, Fiadjoe JE, et al. The efficacy of GlideScope® videolaryngoscopy compared with direct laryngoscopy in children who are difficult to intubate: an analysis from the paediatric difficult intubation registry. Br J Anaesth. 2017;119(5):984-92. PubMed
- Fiadjoe JE, Nishisaki A, Jagannathan N, et al. Airway management complications in children with difficult tracheal intubation from the Pediatric Difficult Intubation (PeDI) registry: a prospective cohort analysis. Lancet Respir Med. 2016;4(1):37-48. PubMed
- Peyton J, Park R, Staffa SJ, et al. A comparison of videolaryngoscopy using standard blades or non-standard blades in children in the Paediatric Difficult Intubation Registry. Br J Anaesth. 2021;126(1):331-9. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.