Copy link
Pediatric Pulmonary Hypertension: Classification, Pathophysiology, and Diagnosis
Last updated: 08/05/2025
Key Points
- Pediatric pulmonary hypertension (PH) is a complex disease with numerous etiologies, the most common of which are PH hypertension of the newborn (PPHN), PH secondary to complex congenital heart disease, and PH secondary to lung disease.
- The pathophysiology of PH involves a deficiency of vasodilator pathways as evidenced by reduced endogenous prostacyclin, decreased expression of nitric oxide synthase and vasoactive intestinal peptide in the lungs, and increased circulating endothelin-1 and serotonin.1
Introduction and Definitions
- PH is a broad term that refers to the presence of elevated mean pulmonary arterial pressures that are caused by various disease processes.1,2
- The estimated incidence of sustained PH is 4-10 cases per million children per year.1
- Historically, PH was defined as a resting mean pulmonary artery pressure (mPAP) of ≥ 25 mmHg, measured using right-sided heart catheterization. The 6th World Symposium on PH (WSPH) proposed modifying the definition of PH in adults to mPAP > 20 mmHg and included a pulmonary vascular resistance (PVR) ≥ 3 Woods units (WU) in precapillary PH.
- The Pediatric Task Force of the WSPH further refined the adult definition to include a time of more than 3 months of age, as infants have physiologically transient elevations in mPAP during the first 3 months of life. To standardize for patient size, PVR is indexed to body surface area in children.
- Therefore, a comprehensive definition of pediatric PH is a mPAP > 20 mmHg with a PVR index ≥ 3 WU x m2 in a child older than three months.
Types of Pulmonary Hypertension
• PH is classified into five groups based on its etiology (Table 1).
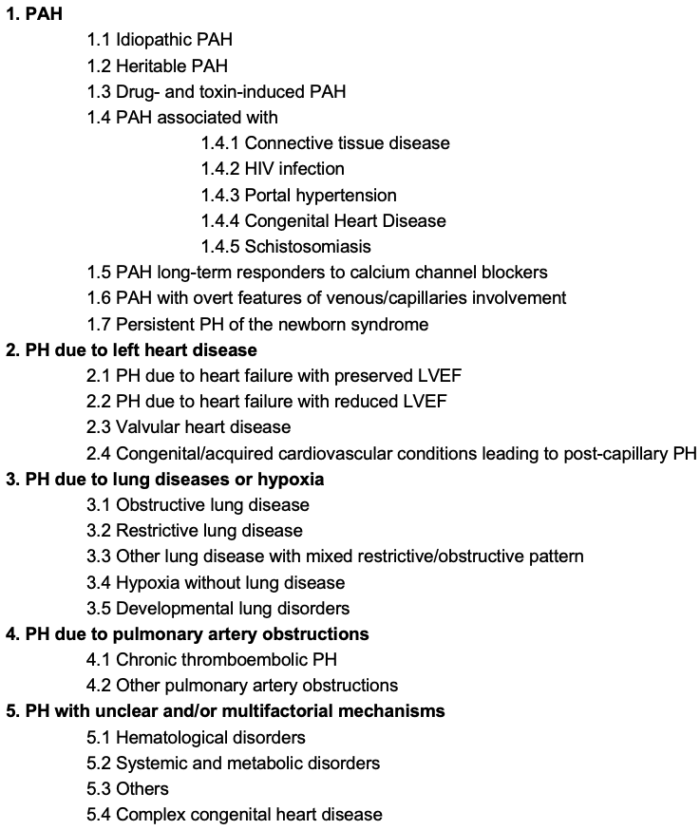
Table 1. Types of pulmonary hypertension. Abbreviations: HIV, human immunodeficiency virus; LVEF, left ventricular ejection fraction; PAH, pulmonary arterial hypertension; PH, pulmonary hypertension; Adapted from: Simonneau G et al. Eur Respir J. 2019;53(1):1801913. CC BY NC 4.0. PubMed
- Additionally, PH is further classified as precapillary PH, postcapillary PH, and combined pre- and postcapillary PH (Table 2).3
- Precapillary PH implies that the increase in PVR is due to the presence of pulmonary vascular disease, rather than elevated mPAPs resulting from increased pulmonary capillary wedge pressures (PCWPs) or increased cardiac output.
- Postcapillary PH implies that the PH is due to increased PCWPs, due to left-sided heart disease.
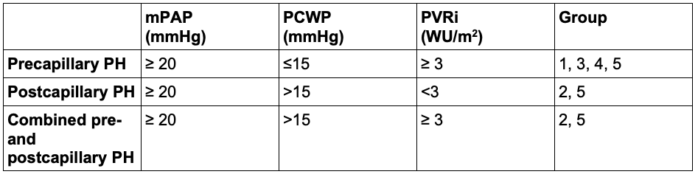
Table 2. Definitions of pulmonary hypertension based on hemodynamic data obtained during right heart catheterization. Abbreviations: mPAP, mean pulmonary artery pressure; PCWP, pulmonary capillary wedge pressure; PH, pulmonary hypertension; PVRi, indexed pulmonary vascular resistance. Adapted from Gelzinis TA. J Cardiothorac Vasc Anesth. 2022;36(6):1552-64. PubMed
Pathophysiology of PH
- The pathophysiology of PH is multifactorial, involving an increase in vascular stiffness, a reduction in the cross-sectional area of the pulmonary vasculature, and an imbalance between pulmonary vasodilators and vasoconstrictors, increasing both PVR and right ventricular (RV) afterload.3
- Pulmonary arterial hypertension (PAH) is a genetically heterogeneous disease characterized by vascular remodeling primarily in the small pulmonary arterioles (Figure 1).3
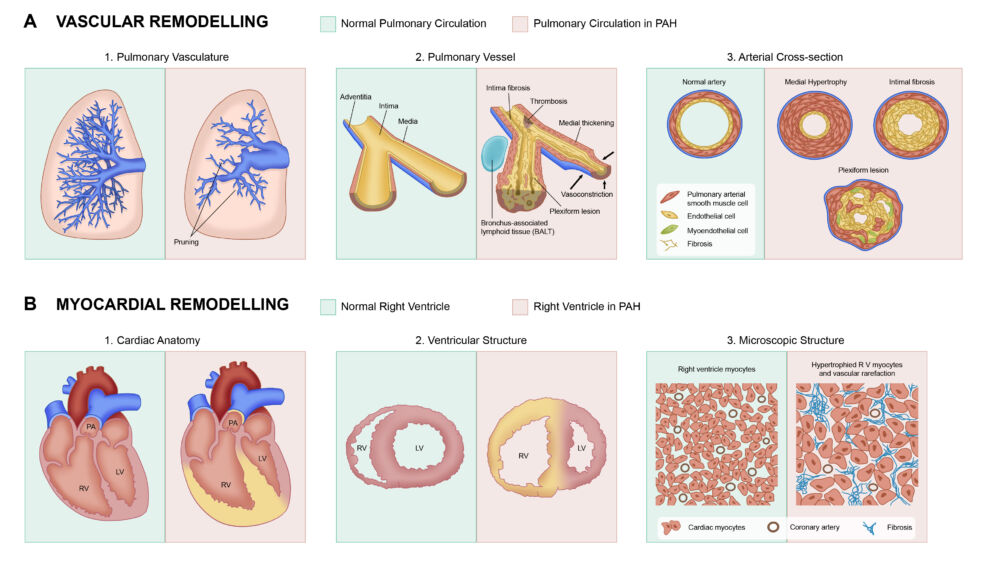
Figure 1. Pathophysiology of pulmonary arterial hypertension (PAH). Adapted from Ryan JJ, Can J Cardiol. 2015 Apr;31(4):391-406. PubMed
- Cellular changes in PAH lead to vessel narrowing, luminal occlusion, neovascularization, and plexiform lesion formation3:
- Adventitial layer: proliferation of fibroblasts and infiltration of immune cells
- Medial layer: proliferation and migration of pulmonary artery smooth muscle cells (PASMC) – a double-elastic lamina develops due to increased muscularization
- Intimal layer: PASMC infiltration
- Endothelial layer: transition of endothelial cells to either an aberrant proliferative and apoptosis-resistant phenotype or to a proinflammatory phenotype that releases excessive amounts of cytokines and growth factors.3
- There is a reduction in the cross-sectional area of the pulmonary vasculature, as well as an increase in vascular stiffness, which alters the transmission of both forward and reflected pulse waves, thereby increasing both the PVR and RV afterload.3
- Patients may have a deficiency of vasodilator pathways, as evidenced by reduced endogenous prostacyclin, decreased expression of nitric oxide synthase, and decreased levels of vasoactive intestinal peptide in the lungs, along with increased circulating endothelin-1 and serotonin.2
- To maintain RV-PA coupling in the setting of elevated PVR, the RV hypertrophies and contractility increases. Eventually, to maintain cardiac output, heart rate increases and the RV dilates, leading to increased metabolic demand, leftward septal bowing, and ultimately, RV-PA uncoupling and right heart failure.
Clinical Presentation
- The signs and symptoms of PH are nonspecific and depend on the etiology. PH is often not diagnosed until the patient becomes markedly symptomatic. Therefore, a high index of clinical suspicion is required for diagnosing PH.3
- Presenting symptoms depend on the etiology of PH and may include dyspnea on exertion, fatigue, weakness, chest pain, palpitations, etc. Symptoms of right heart failure include orthopnea or paroxysmal nocturnal dyspnea, syncope or near-syncope.
- Presenting signs include hypoxia, signs of venous congestion (pedal edema, abdominal distention, right upper quadrant abdominal pain from hepatic congestion, etc.)
- Signs of acute decompensated heart failure include altered mental status, tachycardia, hypotension, and diaphoresis.
- Physical exam often reveals hypotension, resting tachycardia (in patients with impending RV failure), and hypoxemia. Elevated jugular venous pressure is common.
- Other physical findings of RV failure include hepatomegaly, ascites, pleural effusions, mottled extremities, diminished peripheral pulses, and peripheral edema.
Pulmonary Hypertensive Crisis
- A PH crisis is a life-threatening emergency that should be treated aggressively. It is defined as two or more of the following changes occurring acutely over 10 minutes or less.2
- decline in systemic blood pressure >20% from baseline
- decline in oxygen saturation to <90% in an acyanotic patient or a decline of > 10% in a cyanotic patient in the absence of any other cause
- increase in central venous pressure by >20%
- increase or decrease in heart rate by 20%
- PH crisis is characterized by a sudden, rapid increase in PVR with PAP greater than systolic blood pressure (SBP). This is associated with acutely decreased RV function, which can progress to RV failure. The acute increase in RV pressure and volume causes a shift of the interventricular septum towards the left side, thereby reducing LV volume. Increased filling pressures in both ventricles, compensatory tachycardia, and decreased SBP compromise coronary perfusion pressure and flow, leading to low cardiac output and metabolic acidosis.4 Furthermore, decreased pulmonary blood flow causes V/Q mismatch and increased dead space ventilation, resulting in respiratory acidosis and hypoxia (Figure 2).
- The presence of intra-atrial communication (patent foramen ovale, atrial septal defect, etc.) is initially protective: right-to-left shunt augments LA filling and supports cardiac output. However, resultant hypoxia, hypercarbia, and acidosis can cause bradycardia and ischemic cardiac arrest. In the absence of intra-atrial communication, RV failure can rapidly progress to biventricular failure.
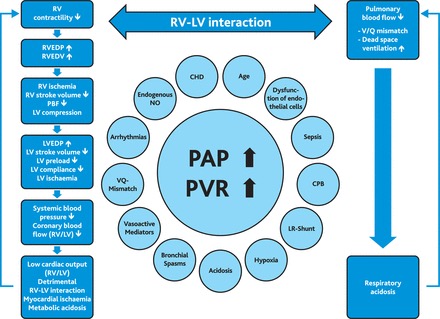
Figure 2. Pulmonary Hypertensive Crisis and Contributing Factors4. Abbreviations: PAH, pulmonary arterial hypertension; RVEDV, RV end-diastolic volume; RVEDP, RV end-diastolic pressure; LVEDP, LV end-diastolic pressure; V/Q, pulmonary ventilation and perfusion; PAH, pulmonary arterial hypertension; PAP, pulmonary artery pressure; PVR, pulmonary vascular resistance; CHD, congenital heart disease; NO, nitric oxide; CPB, cardiopulmonary bypass; LR-Shunt, left-to-right shunt; PBF, pulmonary blood flow. From Kaestner M, et al. Heart. 2016;102 Suppl 2:ii57-ii66. CC BY NC 4.0. PubMed
- Signs and symptoms of a PH crisis in an awake patient include syncope, dyspnea, cyanosis, pallor, bradycardia, RV heave, and bronchospasm. In an anesthetized patient, it usually manifests as decreased EtCO2, hypoxia, and hypotension.
- Treatment of PH crisis includes 100% oxygen, hyperventilation, deepening of anesthesia and/or administration of opioids, vasoconstrictors (phenylephrine, norepinephrine, vasopressin), inotropic support, treatment of bradycardia, institution of iNO therapy, correction of metabolic/respiratory acidosis, and treatment of hypothermia.
Eisenmenger Syndrome
- Large systemic-to-pulmonary shunts can cause progressive pulmonary vascular disease and PAH, leading to shunt reversal with cyanosis.
- Signs/symptoms include cyanosis, dizziness, syncope, arrhythmias, decreased exercise tolerance, dyspnea, fatigue, stroke, elevated hematocrit, coagulopathy, and hepatic and renal insufficiency.
- Increased mortality is associated with saturation < 85%, history of syncope, younger age at time of symptom onset, atrial arrhythmias, right heart failure, New York Heart Association (NYHA) class III-IV, pregnancy, and fixed and elevated PVR.
Prognosis:
- Idiopathic PAH has a median survival of 2-3 years, with 1-year, 3-year, and 5-year survival rates of 68%, 48%, and 34%, respectively.
- PAH patients with NYHA class IV symptoms have a median survival of 6 months.
Diagnosis
- Non-invasive diagnostic tests are used first to determine the etiology of the disease, quantify severity, and assess cardiac function.
- A transthoracic echocardiogram is a non-invasive tool that provides functional and structural assessments of the heart, as well as estimates of pulmonary dynamics.1
- RV size is best evaluated with three-dimensional RV volume measurements or the end-systolic RV/LV diameter ratio.2
- RV performance can be evaluated by the three-dimensional measurement of RV ejection fraction, RV fractional area of change, tricuspid annular planar systolic excursion, etc.2
- PA pressures can be estimated by the velocity of the tricuspid regurgitation jet.
- Right heart catheterization remains the gold standard for diagnosing PH. It can provide definitive information about hemodynamics, responsiveness to pulmonary vasodilators (such as 100% oxygen, inhaled nitric oxide, or intravenous prostacyclin analogs), and cardiovascular anatomy. Furthermore, it allows for interventions to be performed.2
- Cardiac MRI can also be used to assess lung parenchyma and pulmonary vasculature.
References
- Simonneau G, Montani D, Celermajer DS, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J. 2019;53(1):1801913. PubMed
- Wadia RS, Bernier ML, Diaz-Rodriguez NM, Goswami DK, Nyhan SM, Steppan J. Update on Perioperative Pediatric Pulmonary Hypertension Management. J Cardiothorac Vasc Anesth. 2022;36(3):667-676. PubMed
- Gelzinis TA. Pulmonary hypertension in 2021: Part I-Definition, classification, pathophysiology, and presentation. J Cardiothorac Vasc Anesth. 2022;36(6):1552-64. PubMed
- Kaestner M, Schranz D, Warnecke G, Apitz C, Hansmann G, Miera O. Pulmonary hypertension in the intensive care unit. Expert consensus statement on the diagnosis and treatment of paediatric pulmonary hypertension. The European Paediatric Pulmonary Vascular Disease Network, endorsed by ISHLT and DGPK. Heart. 2016;102 Suppl 2:ii57-ii66. PubMed
Other References
- Ross F. Pulmonary hypertension. OpenAnesthesia. OA-SPA Pediatric Podcast of the Month. Published January 1, 2019. Accessed August 5, 2025. Link
- Bechtel A, Chiao S. Pulmonary Hypertension. OpenAnesthesia. Keys to the Cart. Published June 11, 2018. Accessed August 5, 2025. Link
- Kleiman AM. Idiopathic pulmonary hypertension and TEE, part 1. OpenAnesthesia. Intraoperative TEE of the Month. Published May 1, 2016. Accessed August 5, 2025. Link
- Kleiman AM. Idiopathic pulmonary hypertension and TEE, part 2. OpenAnesthesia Intraoperative TEE of the Month. Published June 1, 2016. Accessed August 5, 2025. Link
- Reitman-Ivashkov E. Pulmonary hypertension in pregnancy: Has there been any progress made? OpenAnesthesia. OA-SOAP Fellows Webinar Series. Published June 1, 2016. Accessed August 5, 2025. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.