Copy link
Pediatric Pulmonary Hypertension: Anesthetic Considerations
Last updated: 08/04/2025
Key Points
- The overall therapeutic goals are to dilate and reverse abnormal vascular beds, restore endothelial function, and prevent a pulmonary hypertension (PH) crisis.1
- Key anesthetic considerations include avoidance of increased intrathoracic pressures, hypoxia, hypercarbia, acidosis, catecholamine surges, airway obstruction, and hypotension.
- The anesthesiologist should always be prepared to manage a PH crisis, regardless of the procedure or anesthetic technique chosen. This may include the use of pressors and/or initiation of extracorporeal membrane oxygenation (ECMO).
Introduction
- Children with PH have increased perioperative risk:
- The most substantial risk factors include suprasystemic pulmonary artery (PA) pressures, decreased right ventricular (RV) function, young age, home use of supplemental oxygen, new PH diagnosis prior to initiation of therapy, and lack of a stable therapeutic regimen. Patients with idiopathic or heritable PH may also be at higher perioperative risk.1
- Those with RV hypertrophy (RVH) may be at risk for RV ischemia due to a decrease in coronary flow and lower systemic vascular resistance (SVR) with general anesthesia.2
- Comorbid conditions augment perioperative risk for children with PH. These conditions include sleep disordered breathing, reactive airway disease, chronic lung disease, chronic aspiration, obesity, sickle cell, neuromuscular disease, and congenital/acquired heart disease.1
- Emergent procedures, American Society of Anesthesiologists status III or IV, presence of difficult airway, prolonged procedure time, intraoperative hemodynamic variability, and major fluid shifts also increase perioperative risk.1
Medical Management
The overall therapeutic goals are to dilate and reverse abnormal vascular beds, restore endothelial function, and prevent a PH crisis.1
Inhaled Nitric Oxide (iNO)
- iNO is generally considered first line, especially in persistent pulmonary hypertension of the newborn. iNO diffuses into pulmonary vascular smooth muscle where it activates guanylate cyclase, increases cyclic guanosine monophosphate (cGMP), and increases calcium uptake by the sarcoplasmic reticulum. This results in muscle relaxation, reduced PA pressures, and decreased pulmonary vascular resistance (PVR).1
- iNO is beneficial only in precapillary constriction.
Phosphodiesterase Type 3 (PDE-3) Inhibitors
- PDE-3 inhibitors prevent the breakdown of cyclic adenosine monophosphate (cAMP) in cardiac and vascular smooth muscle. Milrinone is a commonly used PDE-3 inhibitor. It provides ventricular inotropy and lusitropy, in addition to pulmonary and systemic vasodilation. Milrinone can selectively dilate pulmonary vessels.1 It can be administered via either the inhaled or intravenous (IV) route.
Phosphodiesterase Type 5 (PDE-5) Inhibitors
- PDE-5 inhibitors reduce the degradation of cGMP, preserve intracellular cGMP, augment cGMP vasodilation, and suppress pulmonary vascular smooth muscle proliferation. Examples include sildenafil and tadalafil.1 Sildenafil is available both orally and IV. Otherwise, PDE-5 inhibitors are given orally.
Endothelin Receptor Antagonists
- Endothelin-1 mediates vasoconstriction and proliferation of smooth muscle cells. Bosentan (a nonselective endothelin receptor A and B antagonist) lowers PA pressure and PVR, and can increase exercise capacity in children with PH.1
- Of note, bosentan is not intended for acute use. It can be administered orally.
Prostacyclin Analogs
- Prostacyclin analogs are metabolites of arachidonic acid produced by pulmonary vascular endothelium, allowing for pulmonary and systemic vasodilation via increased cAMP. Examples include epoprostenol, treprostinil, and iloprost.1
- They can be administered IV, orally (treprostinil), or via inhalation.
- Importantly, the half-life of epoprostenol is extremely short and should not be discontinued, even temporarily.
- Orenitram (oral treprostinil) must be taken with a balanced meal.
Calcium Channel Blockers (CCBs)
- CCBs reduce calcium influx into vascular smooth muscle and cardiac myocytes. This class of drugs can be considered for patients who respond to acute vasoreactivity testing in the cardiac catheterization laboratory.
- CCBs are not recommended for children younger than one year due to their negative inotropic effects.1
- They can be given IV and orally.
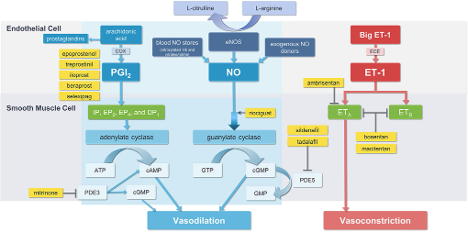
Figure 1. Pharmacologic management of pulmonary hypertension2. Abbreviations: ATP, adenosine triphosphate; cAMP, cyclic adenosine monophosphate; COX, cyclooxygenase; ECE, endothelin-converting enzyme; cGMP, cyclic guanosine monophosphate; DP1, prostaglandin D2 receptor 1; eNOS, endothelial nitric oxide synthase; EP2, prostaglandin E2 receptor; EP4, prostaglandin E4 receptor; ET-1, endothelin-1; ETA, endothelin type A receptor; ETB, endothelin type B receptor; IP, prostaglandin I2 receptor; GTP guanosine triphosphate; NO, nitric oxide; PDE3, phosphodiesterase type 3; PDE5, phosphodiesterase type 5; PGI2, prostaglandin I2. From Mandras S, et al. J Cardiovasc Pharmacol Ther. 2021;26(5):453-462. CC BY NC. Link
Interventional/Surgical Management
- Both balloon angioplasty and stent implantation can be used to treat PA narrowing, thereby improving the distribution of pulmonary blood flow.1
- Creation of an atrial-level communication via septostomy or septoplasty can be used to decompress the RV and increase left ventricular preload and cardiac output.2
- For a patient with suprasystemic pulmonary arterial pressure refractory to medical therapy, the creation of a Potts shunt (surgical anastomosis between the left PA and the descending aorta) leads to Eisenmenger physiology, allowing for decompression of the right heart. Oxygen saturation in the lower extremities will be markedly lower than in the upper extremities.
- Lung transplantation may be considered in PH otherwise refractory to treatment.
Anesthetic Considerations
General Considerations
- Patients with PH should be cared for at a pediatric PH center capable of providing cardiology, intensive care unit, and ECMO support. Care should be provided by a pediatric cardiac anesthesiologist or a pediatric anesthesiologist with expertise in managing patients with congenital heart disease.3
- It is critical to ensure that the patient’s PH status is optimized and that all PH medications are taken on schedule.
- Preoperative testing should include chest X-ray, electrocardiogram, and transthoracic echocardiogram within the last six months. Cardiac catheterization, including vasodilator testing results, should also be reviewed.
- Screening for acute comorbidities (e.g., infection, reactive airway exacerbation, and/or gastrointestinal illness with dehydration) that might worsen PH is crucial. Preoperative optimization or rescheduling may be necessary.
- Patients with chronic pulmonary arterial hypertension likely already have RVH. It is essential to be prepared for greater susceptibility to RV ischemia/failure and arrhythmias.
Intraoperative Management
Choice of anesthetic technique:
- Local anesthesia with light sedation should be used whenever possible.
- Although moderate and deep sedation avoid the risks associated with induction, intubation, and extubation, oversedation and/or airway obstruction can lead to hypercarbia and hypoxemia, resulting in increased PVR.
- General endotracheal anesthesia allows for control of oxygenation and ventilation.
- Regional: Epidural anesthesia has been used successfully in adults. Caution should be used with spinal anesthesia due to decreases in SVR. Infiltration of local anesthetic should be done whenever possible to minimize the need for sedation.
Anesthesia technique:4,5
- Preoperative hypovolemia should be minimized, and IV fluid bolus prior to induction should be considered.
- Clinicians should consider anxiolysis with a benzodiazepine to blunt the catecholamine surge.
- IV induction should be used and inhalational induction should be avoided.
- Hemodynamic goals:4,5
- Avoid increases in PVR – avoid hypoxia, hypercarbia, acidosis, hypothermia, high positive end-expiratory pressure, and pain
- Maintain systemic afterload to maintain coronary perfusion pressure and aim for normotension
- Maintain RV preload – avoid prolonged fasting and drugs that limit venous return or promote venous stasis; aim for euvolemia
- Preserve RV function – optimize coronary perfusion, maintain contractility with inotropes, and avoid myocardial depressants
- Maintain sinus rhythm — atrial kick is vital for adequate filling of the RV
- Recognize and manage pulmonary hypertensive crises (Table 1)
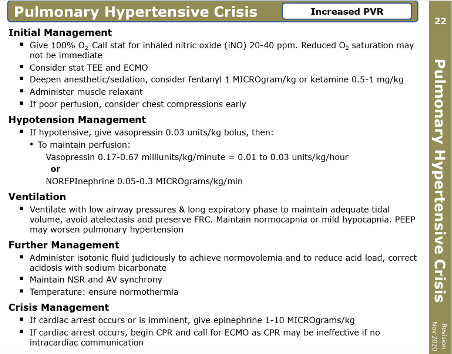
Table 1. Management of pulmonary hypertensive crisis. With permission from the Society for Pediatric Anesthesia Critical Events Checklist. Link
- Ventilation goals:
- Minimize apnea and optimize ventilation during induction and intubation
- Ventilate to functional residual capacity, avoiding atelectasis and overdistention
- Avoid abrupt increases in intrathoracic pressures (i.e., coughing/Valsalva)
- Optimize oxygenation and ventilation
- Specific anesthetic agents (Table 2):
- No specific anesthesia agent has been associated with an increased risk of cardiac arrest. Balanced anesthetics should be tailored to avoid myocardial depression, systemic hypotension, and catecholamine surges.
- In cases of hypotension with preserved function, vasopressin should be considered.
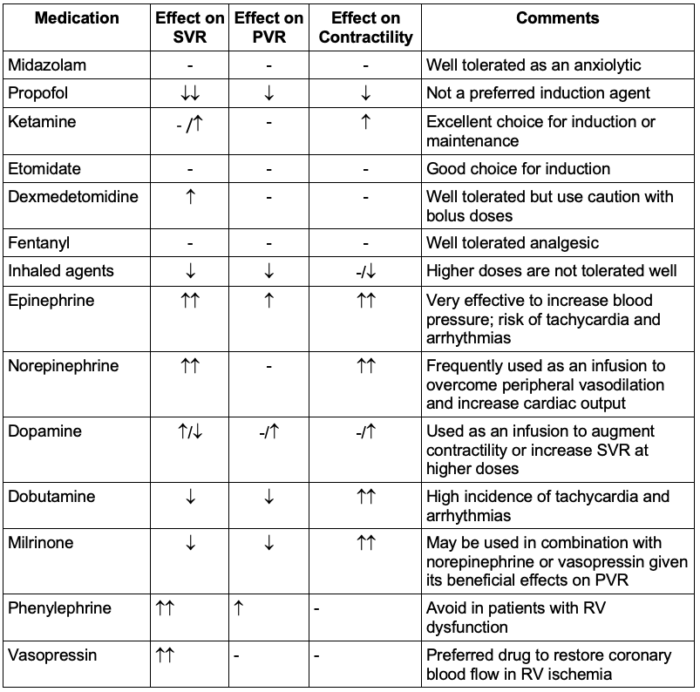
Table 2. Hemodynamic effects of common perioperative medications. -, no change; ↑, increase; ↓, decrease; PVR, pulmonary vascular resistance; SVR, systemic vascular resistance. Adapted from: Wadia, et al. J Cardiothorac Vasc Anesth. 2022;36(3):667-676. Link
- Special cardiopulmonary bypass (CPB) considerations:
- PH patients usually require inotropic and vasodilator support to wean from CPB (i.e., epinephrine and milrinone). Vasopressin may also be required for low SVR and/or decreased coronary perfusion.
- iNO is frequently necessary and is usually started prior to weaning from CPB.
- RVAD or ECMO may be necessary if weaning from CPB is challenging.
Postoperative Management
- Postoperative concerns: RV ischemia/failure, arrhythmias, pulmonary hemorrhage
- Postoperative management of PH patients closely resembles preoperative concerns: avoidance of hypoxia, hypercapnia, hypovolemia, hypothermia, or anything that might trigger a PH crisis.
References
- Wadia RS, Bernier ML, Diaz-Rodriguez NM, et al. Update on perioperative pediatric pulmonary hypertension management. J Cardiothorac Vasc Anesth. 2022;36(3):667-676. PubMed
- Mandras S, Kovacs G, Olschewski H, et al. Combination therapy in pulmonary arterial hypertension-Targeting the nitric oxide and prostacyclin pathways. J Cardiovasc Pharmacol Ther. 2021;26(5):453-62. PubMed
- Nasr VG, Markham LW, Clay M, et al. Perioperative considerations for pediatric patients with congenital heart disease presenting for noncardiac procedures: A scientific statement from the American Heart Association. Circ Cardiovasc Qual Outcomes. 2023;16(1):e000113. PubMed
- Smerling, AJ. Ch. 17, Pulmonary Hypertension. Houck, PJ, et al. Handbook of Pediatric Anesthesia. 1e. McGraw-Hill Education; 2015: 70-2.
- Fischer LG, Aken HV, Bürkle H. Management of pulmonary hypertension: physiological and pharmacological considerations for anesthesiologists. Anesth Analg. 2003;96(6):1603-16. PubMed
Other References
- Ross F. Pulmonary hypertension. OpenAnesthesia. OA-SPA Pediatric Podcast of the Month. Published January 1, 2019. Accessed August 4, 2025. Link
- Bechtel A, Chiao S. Pulmonary Hypertension. OpenAnesthesia. Keys to the Cart. Published June 11, 2018. Accessed August 4, 2025. Link
- Kleiman AM. Idiopathic pulmonary hypertension and TEE, part 1. OpenAnesthesia. Intraoperative TEE of the Month. Published May 1, 2016. Accessed August 4, 2025 Link
- Kleiman AM. Idiopathic pulmonary hypertension and TEE, part 2. OpenAnesthesia Intraoperative TEE of the Month. Published June 1, 2016. Accessed August 4, 2025. Link
- Reitman-Ivashkov E. Pulmonary hypertension in pregnancy: Has there been any progress made? OpenAnesthesia- SOAP Fellows Webinar Series. Published June 1, 2016. Accessed August 4, 2025. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.