Copy link
Pediatric Acute Pain Management
Last updated: 07/31/2023
Key Points
- Children experience pain, and untreated early pain experiences can lead to long-term adverse neurodevelopment effects.
- Appropriate pain assessment is the critical first step in effective pain management, but it can be challenging.
- Pediatric acute pain management is increasingly characterized by a multimodal approach that incorporates both nonpharmacologic and pharmacologic therapies and regional anesthesia to achieve the best results.
Introduction
- Pain is a subjective experience defined as an “unpleasant sensory and emotional experience associated with or resembling actual or potential tissue damage” that is influenced by biological, psychological, and social factors.1
- Effective treatment requires familiarity with appropriate pain assessment tools, the ability to address both pain severity and etiology, an understanding of the impact of patient-specific pathophysiology on treatment choices, and the management of therapy-related side effects.
Neurophysiology of Pain
- Sensory afferent neurons that respond to noxious stimuli (nociceptors) are located in the dorsal root ganglion and are characterized into three groups (A, B, and C) depending on diameter, degree of myelination, conduction speed, and distribution of fibers:
- Aδ fibers: large, myelinated fibers that mediate pain sensations
- Transmit “first pain” which is localized and sharp
- B fibers: medium-size myelinated fibers
- Postganglionic, sympathetic, and visceral afferents
- C fibers: slow-conducting unmyelinated fibers that modulate nociceptive stimuli
- Transmit “second pain” which is diffuse, persistent, burning, and slow to be perceived
- Aδ fibers: large, myelinated fibers that mediate pain sensations
Pain Assessment
- Multiple validated instruments are available to assess pain in children. Ideally, they should be combined with parental and nursing input and contextualizing pain scores (Table 1).
- Self-reporting is the “gold standard” for assessment, but may only be possible for older children or those with cognitive and communicative abilities.2
- For children unable to communicate pain due to young age, developmental delay, or medical therapy, objective scales that combine physiologic parameters and behavioral measures for pain can be utilized, but none are ideal.3
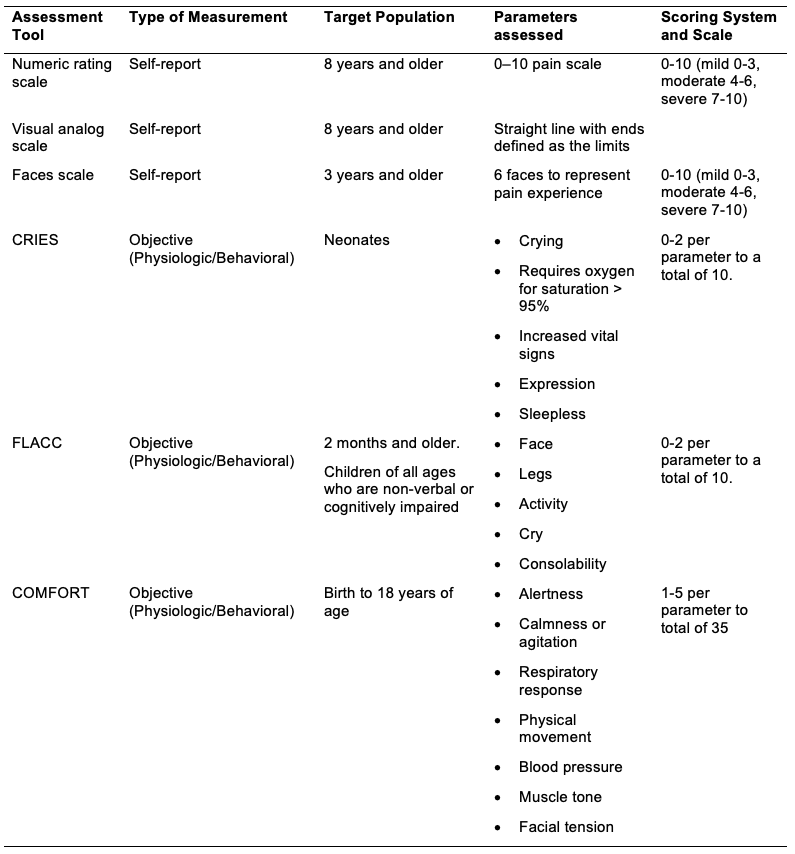
Table 1. Commonly used pediatric pain scales (Adapted from Vecchione TM, et al. Error traps in acute pain management in children. Pediatric Anesthesia. 2022;32(9):982-92.3
Treatment Modalities
Multimodal Analgesia
- It involves using various analgesic medications and techniques that target different mechanisms of action to have additive or synergistic effects to maximize pain control and minimize drug-induced side effects (Figure 1).
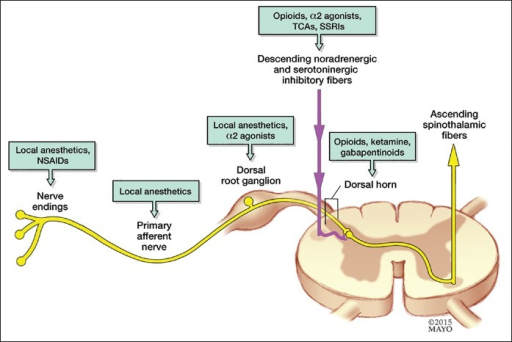
Figure 1. Various drugs act at different anatomic locations along the pain signaling pathway. Source: Gorlin AW, et al. Journal of Anesthesiology, Clinical Pharmacology. 2016. Open-i, Accessed on February 4, 2023. Link.
Pharmacologic Therapies
- Opioids
- It is helpful to consider pain intensity, patient age, coexisting comorbidities, potential drug interactions, treatment history, and route administrations when choosing the appropriate opioid analgesic.
- Patient-controlled analgesia (PCA) allows patients, parents, or nurses to administer small opioid doses and has been shown to improve pain scores and patient/parent satisfaction.
- Various systemic analgesic adjuncts can be used to optimize pain management (Table 2).
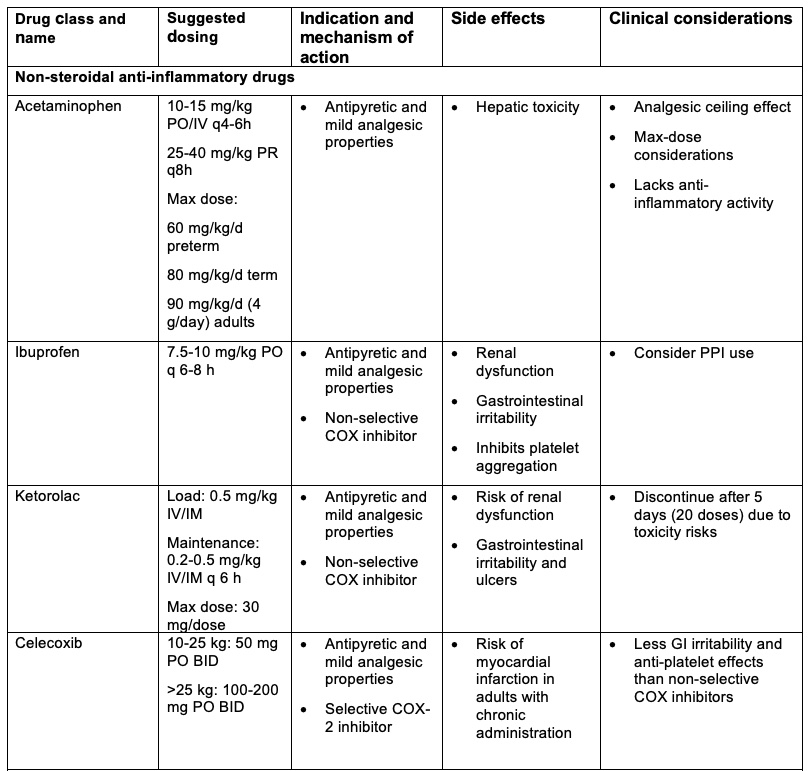
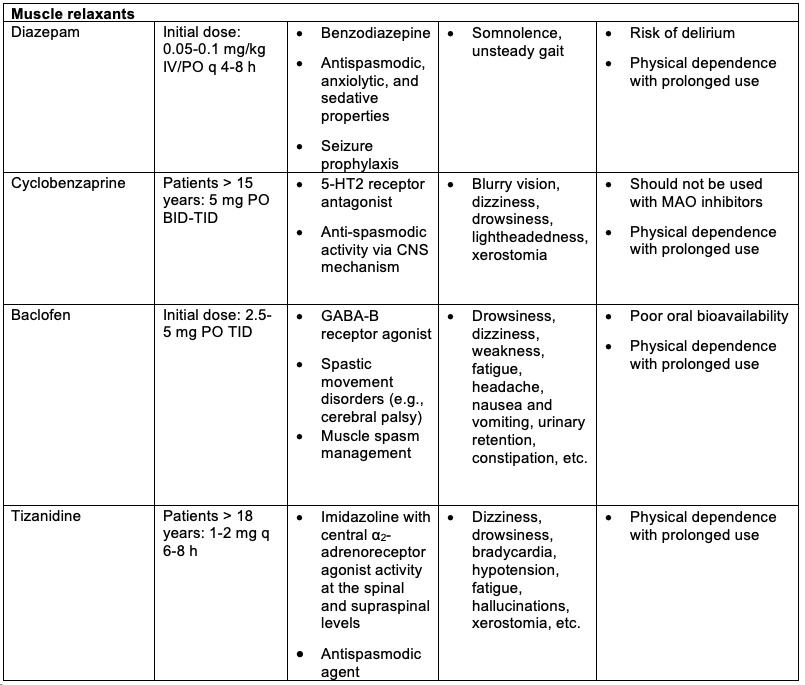
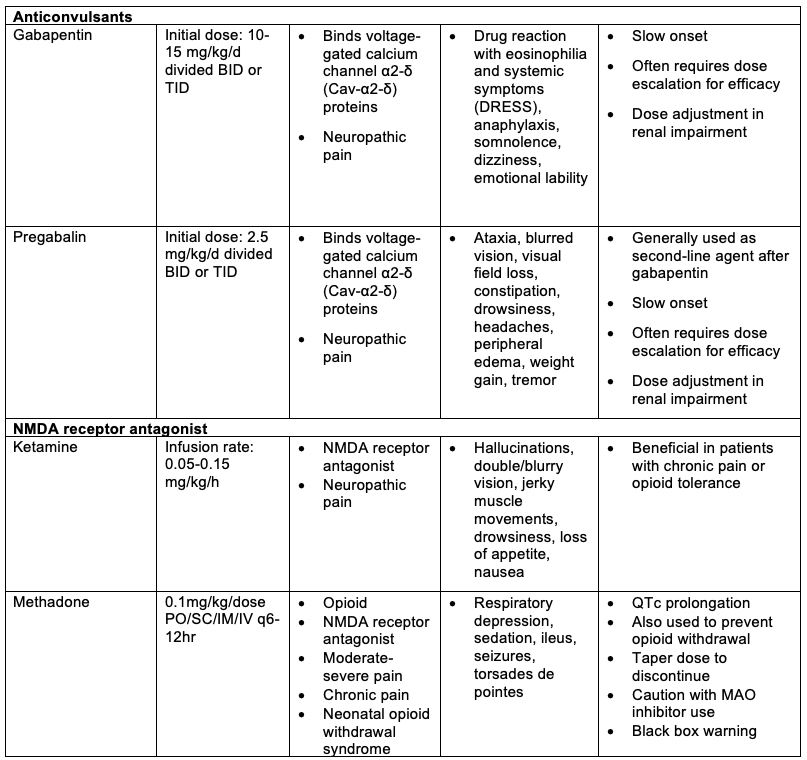
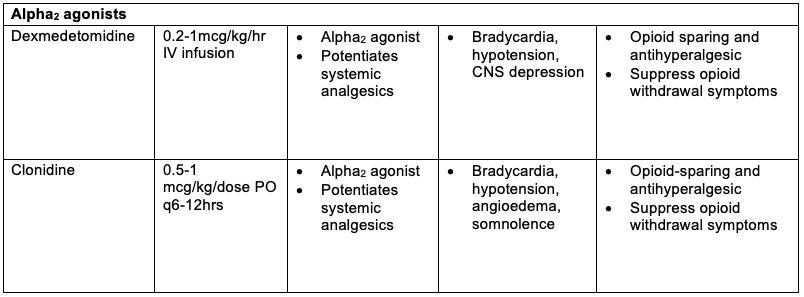
Table 2. Systemic analgesic adjuncts. PO = per oral, IV = intravenous, IM = intramuscular, SC = subcutaneous, NMDA = N-methyl D-aspartate, COX = cyclooxygenase, CNS = central nervous system, GABA = gamma aminobutyric acid, MAO = monoamine oxidase. Adapted from Vecchione TM, et al. Error traps in acute pain management in children. Pediatric Anesthesia. 2022;32(9):982-92.3
Regional Anesthesia
- Neuraxial blockade
- Spinal anesthesia: helpful in preterm infants to minimize the risk of apnea
- Epidural
- Peripheral nerve blockade
References
- Raja SN, Carr DB, Cohen M, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976-82. PubMed
- Verghese S, Hannallah RS. Acute Pain Management in Children. J Pain Res. 2010; 3:150-123. PubMed
- Vecchione TM, Agarwal R, Monitto CL. Error traps in acute pain management in children. Pediatric Anesthesia. 2022;32(9):982-92. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.