Copy link
PACU Discharge Criteria
Last updated: 08/20/2025
Key Points
- Prior to the discharge from the postanesthesia care unit (PACU), the patient should have stable vital signs, a patent airway, and return to baseline consciousness.1
- Scoring systems and standardized protocols aid in evaluation, but clinical judgment is critical.2
- Pediatric discharge emphasizes airway stability, hydration status, behavioral normalization, and pain control.3
- High-risk populations (obstructive sleep apnea, cardiac disease, prolonged surgeries) often require extended monitoring.4
- Ongoing advances in technology, anesthetic techniques, and quality improvement initiatives are expected to enhance patient safety further and improve PACU efficiency.
Introduction
- The PACU is a critical recovery area where patients are monitored following anesthesia and surgery.1
- Safe discharge from PACU requires structured assessment of vital signs, airway patency, neurologic status, pain control, and surgical site integrity.1
- Scoring systems such as the Modified Aldrete Score and Postanesthesia Discharge Scoring System (PADSS) improve standardization and patient safety.2
- Pediatric and special patient populations require additional criteria for safe discharge planning.3,4
- Clinical judgment complements structured tools to ensure individualized patient-centered care.2
Summary Checklist Before PACU Discharge
- Vital signs are stable and within 20% of baseline.2
- A patent airway is maintained independently.2
- SpO₂ is greater than 92% or at preop baseline.1
- The patient has returned to baseline alertness and orientation.2
- Pain is controlled to a tolerable level.2
- Minimal postoperative nausea and vomiting persists.2
- No significant bleeding is noted.2
PACU Discharge Scoring Systems
- Several scoring systems have been devised to assess readiness for discharge from the PACU.
- The Modified Aldrete Score evaluates activity, respiration, circulation, consciousness, and oxygen saturation.1 (Table 1)
- Each domain is scored 0–2 points; a total score of 9 or greater indicates readiness for phase I PACU discharge.1
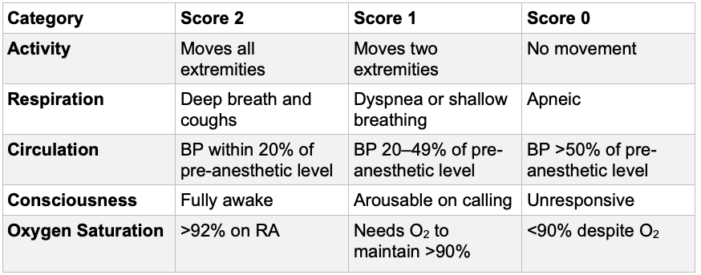
Table 1. Modified Aldrete score. BP = blood pressure, RA = room air
- PADSS adds evaluation of ambulation, nausea/vomiting, pain, and bleeding2 (Table 2).
- The Aldrete score can be used to evaluate initial patient recovery after surgery, and PADSS can be used to assess home-readiness.2
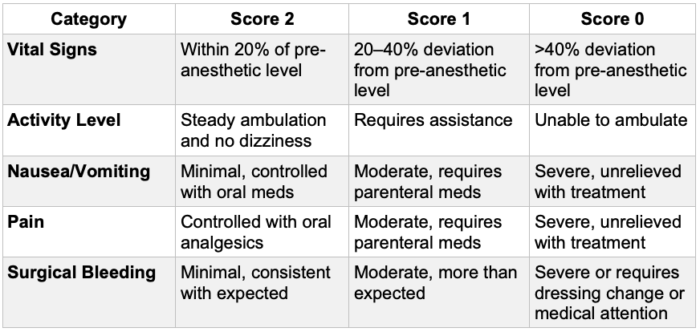
Table 2. Postanesthetic Discharge Scoring System
Pediatric-Specific Considerations
- Emergence from anesthesia in children differs significantly when compared with adults. Suggested PACU discharge criteria in children to an inpatient setting include the following.3
- Adequate recovery of airway and respiratory reflexes to support gas exchange and protect against pulmonary aspiration
- Stable hemodynamics and control of any surgical bleeding
- Reasonable control of pain and vomiting
- Return to baseline level of consciousness unless the patient is being transferred to an intensive care unit (ICU)
- Appropriate duration of observation after opioid, naloxone, or flumazenil administration
- Pediatric PACU discharge criteria for outpatients include all the items listed above plus the following.3
- Stable cardiovascular function and airway patency
- The child is easily aroused.
- The child can talk (if age-appropriate and able to do so preoperatively).
- The child can sit up unaided (if age-appropriate and able to do so preoperatively).
- The state of hydration is adequate.
- Adequate analgesia to permit the use of oral analgesics
- Adequate control of nausea and vomiting to allow oral hydration
- Unless there is a high risk for urinary retention (urethral surgery, history of urinary retention), children should not be required to void before discharge.3
PACU Bypass
- The PACU is traditionally divided into phases 1 and 2. Phase 1 PACU has monitoring and staffing ratios equivalent to the ICU.
- Phase 2 is a transitional period between intense observation and either the surgical ward or home.
- The concept of bypassing or “fast-tracking” phase 1 is becoming more common as fast-offset anesthetic agents and practices are emerging.
- PACU bypass is typically appropriate for patients who have received either monitored anesthesia care or peripheral regional anesthesia.
- Phase I PACU monitoring is typically required for patients receiving general anesthesia or neuraxial regional techniques.
- Ultimately, patient comorbidities, surgical techniques/complications, and pharmacological choices determine the appropriate level of postoperative care on an individual basis.
Risk Stratification and Special Populations
- Patients with obstructive sleep apnea require extended monitoring due to airway collapse risk, especially after the administration of opioids.4
- The presence of hypertension increases the odds of extended PACU stay in the morbidly obese population.4
- Patients undergoing cardiac procedures must have stable hemodynamics and no ischemia.4
- Elderly patients are at increased risk for postoperative complications and should be monitored for return to cognitive baseline. Baseline cognitive function should be documented preoperatively.4
- Longer case duration is associated with extended PACU stay, likely related to more complex surgeries and increased administration of anesthetic medications.4
- Patients who receive a general anesthetic have a higher rate of PACU complications than those receiving regional or monitored anesthesia care.6
- Patients with behavioral disorders should return to their individualized baseline.3
Postoperative Complications in the PACU
- The overall PACU complication rate is estimated at around 23.7%.6
- The most common PACU complications include hypoxia, hypotension, nausea/vomiting, and agitation.2,6
- The incidence of dysrhythmias and hypertension in the PACU is low (1.4% and 1.0% respectively), but these are the most common reasons for unplanned ICU admission.6
- Hypothermia in the PACU can prolong the effect of anesthetic medications and cause shivering.6
- Rapid identification and management of problems reduce unplanned admissions.6
- Airway obstruction is more common in patients with OSA or sedative use.4
- Hemodynamic issues may stem from surgical complications or medications.6
Discharge Barriers and Management
- Uncontrolled pain requires multimodal analgesia, including regional techniques, nonsteroidal anti-inflammatory drugs, and other nonopioid analgesics when possible.5
- Persistent nausea/vomiting should be treated, as discharge can be delayed until it improves.5 Prophylactic antiemetic drugs should be used and tailored to specific patients’ risk profiles.5
- Hypothermia should be corrected as it has been shown to increase PACU length of stay significantly.6
- Patients should be medically optimized before elective procedures, which includes education about which medications to take and hold leading up to their surgeries. Mismanagement can delay PACU discharge and lead to adverse outcomes.5
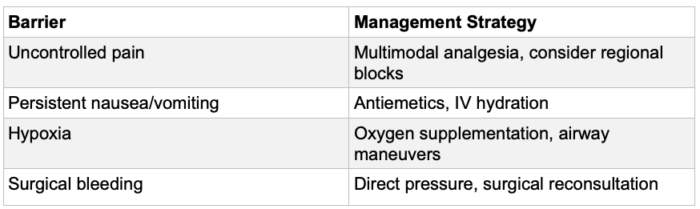
Table 3. Common PACU discharge barriers and management
Patient Education Prior to Discharge
- Verbal and written discharge information is essential for avoiding problems after discharge.2,5
- Instructions should cover medications, activity, follow-up, and warning signs.5
- Family and patient understanding should be confirmed.5
- The team of educators includes anesthesia providers, PACU nurses, and surgeons.5
- Coordination ensures safe discharge planning.5
Quality Improvement and PACU Metrics
- Tracking metrics such as average PACU length of stay and unplanned admissions helps improve the quality of care.7
- Data from electronic health records can be used to monitor trends in PACU utilization.7
- Interdisciplinary debriefings after adverse PACU events may identify process improvements.7
- Benchmarking institutional performance with national standards helps maintain quality.7
Future Directions in PACU Management
- Enhanced recovery after surgery protocols are being extended into the PACU to expedite recovery.7
- Outcome detection strategies to monitor for adverse events are expected to become more sophisticated, allowing for more targeted quality improvement.7
- Increased use of nonopioid analgesics and regional anesthesia is expected to continue to reduce PACU length of stay.5
- Advances in computing and artificial intelligence may enable automated patient communication that can enhance anesthesiologists’ ability to deliver personalized education and procedure-specific messaging.7
References
- Aldrete JA. The post-anesthesia recovery score revisited. J Clin Anesth. 1995;7(1):89-91. doi:10.1016/0952-8180(94)00001-k PubMed
- Chung F. Discharge criteria--a new trend. Can J Anaesth. 1995;42(11):1056-1058. doi:10.1007/BF03011083 PubMed
- Earley TM, Havidich JE, Taenzer AH. In: Côté CJ, Lerman J, Anderson BJ (eds). A Practice of Anesthesia for Infants and Children. 7th ed., Elsevier, 2025.
- Dexter F, Wachtel RE, Epstein RH. Decreasing the Hours That Anesthesiologists and Nurse Anesthetists Work Late by Making Decisions to Reduce the Hours of Over-Utilized Operating Room Time. Anesth Analg. 2016;122(3):831-842. doi:10.1213/ANE.0000000000001136 PubMed
- White PF. Ambulatory anesthesia advances into the new millennium. Anesth Analg. 2000;90(5):1234-1235. doi:10.1097/00000539-200005000-00047 PubMed
- Hines R, Barash PG, Watrous G, O'Connor T. Complications occurring in the postanesthesia care unit: a survey. Anesth Analg. 1992;74(4):503-509. doi:10.1213/00000539-199204000-00006 PubMed
- Tung A, Dutton RP. Anesthesia Quality Improvement: Current State and Future Opportunities. Anesthesiology. 2025;142(1):217-228. doi:10.1097/ALN.0000000000005252 PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.