Copy link
Opioids: Basics
Last updated: 01/30/2024
Key Points
- Opioids have been utilized medicinally for thousands of years.
- Opioids may be classified by analgesic potency, origin of the substance, or action at different receptors.
- Opioids have differential effects based on the receptor at which they are acting.
- The primary mechanism of action for opioid analgesia is located within the central nervous system.
Introduction
- Opium has been utilized by civilizations dating back to 30,000 BC. The first medicinal use of opioids was documented around 4,000 BC in a Sumerian text. Morphine was isolated in 1804, after which it became a popular treatment for pain, cough, and diarrhea. The first fatal morphine overdose from respiratory depression occurred in 1853. The structure of morphine was discovered in the 1920s, which led to the creation of synthetic opioids using chemical principles.1,2
- Opioids are now widely utilized for managing acute and chronic pain. Given the availability of numerous compounds, it is imperative to understand pharmacological properties when choosing an opioid for clinical use to ensure safety and efficacy.
Definitions and Terminology
- Opium is a mixture of alkaloids extracted from the poppy plant (Papaver somniferum). The term “opioid” refers to naturally occurring, synthetic, or semisynthetic compounds that bind to specific opioid receptors. The term opiate refers to naturally occurring compounds derived from the poppy plant, and morphine is the prototype opiate.3 Often, the terms opioid and opiates are used interchangeably.1,2
- The term narcotic is derived from the Greek word for stupor and refers to any medication that causes dependence and, therefore, includes nonopioid medications.
- The following are important terms to understand regarding opioids:
- Tolerance: diminished effect with repeated administration or an increased dose requirement to achieve the same effect
- Withdrawal: symptoms that appear when opioid administration is stopped in a subject with opioid tolerance
- Dependence: the capacity to experience withdrawal when opioids are tapered or when an opioid reversal agent is given
- Addiction: condition of compulsive drug seeking (craving, compulsive drug-seeking)
Classification
- Several classifications of opioids have been proposed.3
- Traditional classification: based on analgesic potency
- Strong: morphine, fentanyl, remifentanil, alfentanil, sufentanil, meperidine
- Intermediate: buprenorphine, pentazocine, butorphanol, nalbuphine
- Weak: codeine
- Origin of opioid
- Naturally occurring: morphine, codeine, papaverine, thebaine
- Semisynthetic: diamorphine, dihydrocodeine, buprenorphine
- Synthetic:
- Phenylpiperidines: meperidine, fentanyl, alfentanil, sufentanil
- Diphenylpropylamines: methadone, dextropropoxyphene
- Morphinians: butorphanol, levorphanol
- Benzomorphans: pentazocine.
- Action at opioid receptor
- Pure agonists: morphine, fentanyl, alfentanil, remifentanil, sufentanil
- Partial agonist: buprenorphine
- Agonist-antagonists: pentazocine, nalbuphine, nalorphine
- Pure antagonists: naloxone, naltrexone
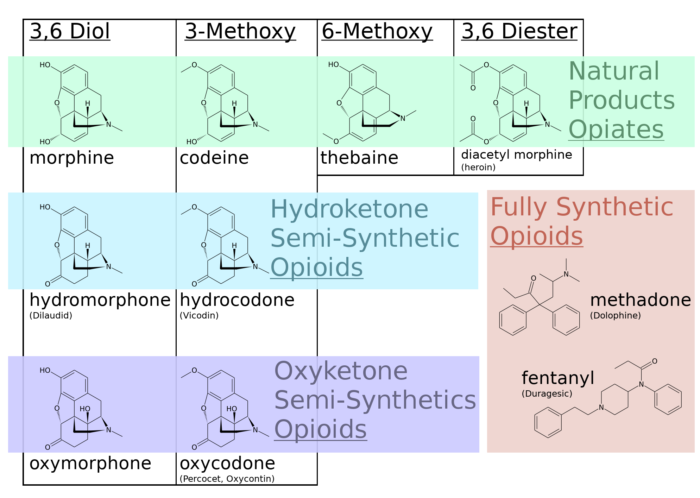
Structure
- Opioids have common structural characteristics, as shown in Figure 1. Morphine is a benzylisoquinoline alkaloid. Note that codeine is a simple modification of morphine. Semisynthetic opioids are also created by simple modifications of morphine. Fentanyl and its congeners are more complex modifications of meperidine, a phenylpiperidine derivative.
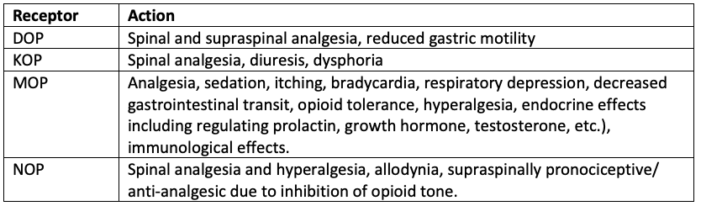
Table 1. Action of opioids at different opioid receptors. Source: Chong WS, Johnson DS. Update on opioid pharmacology. Anaesthesia Tutorial of the Week 64. WFSA. CC BY NC ND 4.0. Link
- MOP, DOP, and KOP receptors are widely expressed in the central nervous system, where they mediate the analgesic and mood-altering actions of opioids. Opioid receptors are also located at peripheral sites, including the vas deferens, knee joint, gastrointestinal tract, heart, and immune system.4
- MOP receptors in the brain and spinal cord are primarily responsible for opioid-induced analgesic effects.
- MOP receptors are highly concentrated in the dorsal horn of the spinal cord.
- MOP receptors in peripheral terminals modulate the perception of pain.
- MOP receptors in the small intestine modulate gut motility.
- Once an opioid ligand binds an opioid receptor, the intracellular cascade commences, as seen in Figure 2. Current data suggests that the interplay between the two sides of the pathway demonstrated in the figure may alter the balance between analgesia (i.e., cell response) and side effects, as mediated by β-arrestin.4
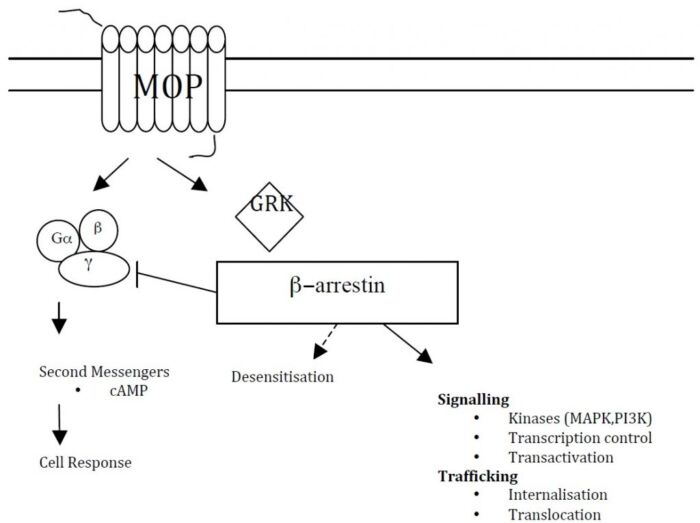
Figure 2. Intracellular opioid receptor activation. Source: Chong WS, Johnson DS. Update on opioid pharmacology. Anaesthesia Tutorial of the Week 64. WFSA. CC BY NC ND 4.0. Link
- Opioid-induced side effects include respiratory depression, pruritus, sedation, nausea, vomiting, constipation, physical dependence, tolerance, and neuroendocrinological changes such as increased antidiuretic hormone (ADH) secretion and inhibition of gonadotropin-releasing hormone (GRH) and corticotropin-releasing hormone (CRH).
Mechanism of Action
- Nociceptive pain is transmitted via C-fibers (slow, unmyelinated) and Aδ-fibers (fast, myelinated). Fibers enter the dorsal horn of the spinal cord to ascend via the spinothalamic tract. Once in the thalamus, this information is passed to the periaqueductal gray, amygdala, and somatosensory cortex to facilitate pain perception.
- Opioids act on the central nervous system to:
- stimulate descending serotonergic and noradrenergic inhibitory pathways; and
- inhibit ascending excitatory nociceptive neuronal pathways.
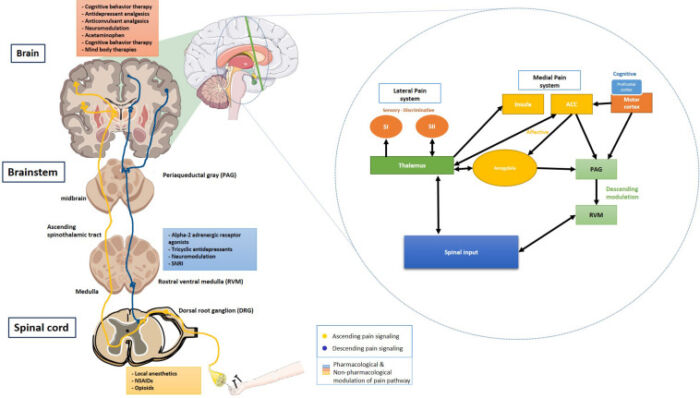
Figure 3. Simplified diagram of activated descending inhibitory pathways (yellow lines) in response to afferent nociceptive input (blue lines). The inset shows a schematic of cortical modulation of pain. Source: Khera T, et al. Cognition and Pain: A Review. Front Psychol. 2021; 21:12:673962. CC BY.
References
- Dahan A, Niesters M, Smith T, Overdyk F. Opioids. In: Barash PG, et al. Clinical Anesthesia. 8th ed., Philadelphia, PA; Wolters Kluwer; 2017: 505-527
- Jacob A, Kopp S, Bacon D, Smith H. The history of anesthesia. In: Barash PG, et al. Clinical Anesthesia. 8th ed., Philadelphia, PA; Wolters Kluwer; 2017: 1-25
- Trivedi M, Shaik S, Gwinnutt C. Pharmacology of opioids-part 1. Anaesthesia Tutorial of the Week 64. World Federation of Societies of Anaesthesiologists. Link
- Chong WS, Johnson DS. Update on opioid pharmacology. Anaesthesia Tutorial of the Week 64. World Federation of Societies of Anaesthesiologists. Link
- Khera T, Rangasamy V. Cognition and Pain: A Review. Front Psychol. 2021; 21:12:673962. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.