Copy link
Neurofibromatosis
Last updated: 07/31/2025
Key Points
- Neurofibromatosis (NF) is a group of autosomal dominant disorders that present unique perioperative challenges due to their multi-system involvement.
- The two most common types, NF1 and NF2, differ significantly in genetics, clinical features, and anesthetic considerations.
- Anesthetic management focuses on airway abnormalities, cardiovascular issues, and potential nervous system complications. They may present difficult neuraxial anesthesia.
- Close coordination with a multidisciplinary team is essential to mitigate risks.
Introduction
- NF is a multisystem genetic disorder characterized by pigmentary changes and the development of benign tumors along nerves and in other tissues. The two main forms, NF1 and NF2, differ in clinical presentation and pathophysiology.
- NF1 (Von Recklinghausen’s disease) is more common and is associated with mutations in the NF1 gene. NF2 primarily affects the central nervous system (CNS) and is associated with mutations in the NF2 gene.1,2 Schwannomatosis (SWN) is considered a distinct but related condition to NF2.
- The overall incidence of NF1 is approximately 1 in 3,000 births, while NF2 occurs in approximately 1 in 25,000 births.3
- Patients with NF require specialized anesthetic care due to the diverse manifestations that affect the airway, cardiovascular, and nervous systems.
- This summary reviews the perioperative considerations for patients with NF to guide safe anesthetic practices.
Pathophysiology and Clinical Features
NF Type 1 (NF1)
- Genetics and Tumor Suppression: Mutation of the NF1 gene leads to dysfunction in the neurofibromin protein, a tumor suppressor involved in regulating the RAS/MAPK signaling pathway. This dysfunction results in uncontrolled cell proliferation and tumor formation.1,4
Clinical Features:
- The clinical manifestations of NF1 emerge over time.
- Cutaneous manifestations:
- Cafe-au-lait spots: These are hyperpigmented macular skin lesions that are often apparent early in childhood and increase in number over childhood. The presence of six or more café-au-lait spots is highly suggestive, but not diagnostic of NF1.
- Neurofibromas: Benign nerve sheath tumors that can be cutaneous, subcutaneous, or plexiform (involving multiple nerve branches and surrounding tissue)
- Skeletal abnormalities:
- Scoliosis, kyphoscoliosis, and bone dysplasia (e.g., sphenoid wing dysplasia, pseudarthrosis)
- Short stature and reduced bone mineral density in some patients
- Cardiovascular manifestations1,5
- Hypertension is often secondary to renal artery stenosis.
- Pheochromocytomas: Catecholamine-secreting tumors requiring careful preoperative management
- Aortic and other vascular anomalies
- Neurological manifestations1,4
- Optic pathway gliomas
- Lisch nodules are raised, tan-colored hamartomas of the iris. These are specific to NF1 and are uncommon before the age of six.
- Learning disabilities and attention deficit disorders
- Seizures and macrocephaly
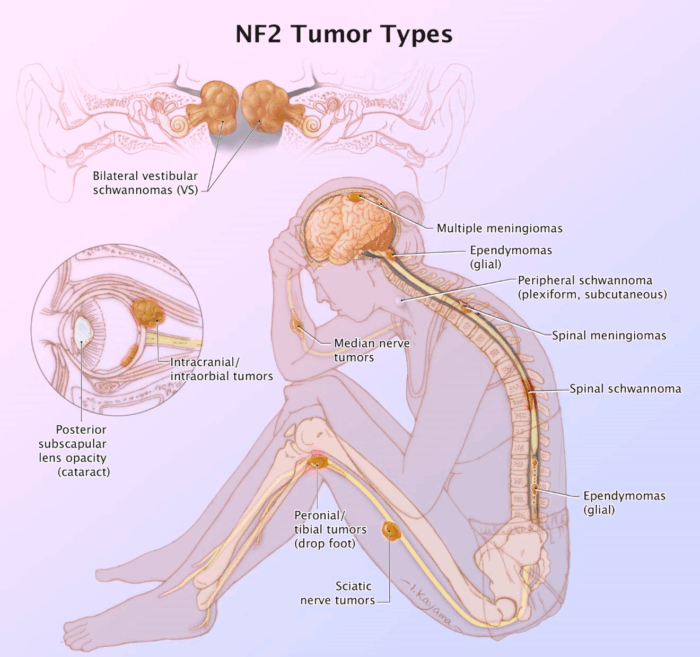
NF Type 2 (NF2)
- Genetics and Tumor Suppression: Mutation of the NF2 gene on chromosome 22 results in dysfunction of the merlin (schwannomin) protein, which regulates cell growth and contact inhibition.2,4
Clinical Features:
- Bilateral vestibular schwannomas leading to hearing loss, tinnitus, and balance issues
- Meningiomas, spinal ependymomas, and gliomas
- Peripheral neuropathy and mononeuropathy2,6
SWN
- Genetics and Tumor Suppression: This rare form of NF is characterized by mutations in the SMARCB1 or LZTR1 genes. It lacks hallmark features of NF1 or bilateral vestibular schwannomas of NF2.3,4
Clinical Features:
- Multiple painful peripheral schwannomas without vestibular tumors3
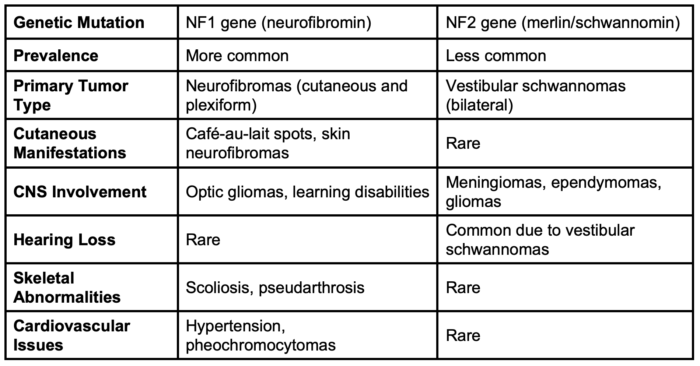
Table 1. Similarities and differences between NF1 and NF2
Treatment, Complications, and Prognosis
- Unfortunately, there is no definitive treatment for NF1, although mitogen-activated protein kinase inhibitors are being evaluated in clinical trials.
- Longitudinal care for patients with NF1 focuses on early detection through annual surveillance examinations and diagnostic studies, as well as the treatment of symptomatic complications as they arise.5
- NF1 patients may develop malignant peripheral nerve sheath tumors, which are the primary cause of decreased survival.6,7
- NF2 often leads to progressive hearing loss and neurologic deficits.7,8
- Chronic pain, deformities, or neurological impairments can significantly impact quality of life.2,6
- Lifespan in NF1 may be reduced by up to 10-15 years due to complications.5
Anesthetic Considerations
Preoperative Evaluation
- Airway assessment:
- Patients with NF1 may have airway obstruction due to neurofibromas and plexiform lesions in the oropharynx or larynx, or skeletal abnormalities, such as cervical spine deformities.
- Suspicion raised by history of dysphagia, stridor, or voice change.9
- Imaging studies (computed tomography, magnetic resonance imaging) are recommended for assessing airway anatomy in complex cases.5,9
- Cardiovascular assessment:
- Clinicians should evaluate for potential causes of hypertension, such as renal artery stenosis or pheochromocytomas.
- Pheochromocytoma management includes alpha-adrenergic blockade (e.g., phenoxybenzamine) followed by beta-blockade to stabilize hemodynamics.5,9
- Hypertrophic cardiomyopathy may occur.9
- Neurological assessment:
- Baseline neurological deficits should be identified, as these may impact intraoperative monitoring.
- Clinicians should evaluate for signs of increased intracranial pressure (ICP) or spinal cord compression.
- Clinicians should plan for neuromonitoring if surgery involves the nervous system.5,9
Intraoperative Management
- Airway management:
- Difficult airway management should be anticipated. Clinicians should prepare to use advanced airway devices, such as video laryngoscopy or fiberoptic bronchoscopy.
- Traumatic intubation should be avoided to prevent airway swelling or injury near neurofibromas.5,9
- Monitoring:
- Standard American Society of Anesthesiologists monitors should be used. Invasive arterial pressure monitoring should be used in cases with significant cardiovascular involvement.
- In surgeries involving CNS tumors, neuromonitoring (e.g., somatosensory and motor evoked potentials) should be used.5,9
- Anesthetic agents:
- Agents that increase ICP in patients with CNS tumors or hydrocephalus should be avoided.
- Clinicians should titrate anesthetic agents to maintain hemodynamic stability, particularly in pheochromocytoma cases.
- Regional anesthesia may be contraindicated or require modification due to neurofibromas or scoliosis.5,9
- Positioning and pressure injury prevention:
- Clinicians should position carefully to avoid compressing neurofibromas, which can be painful and prone to vascular compromise.
- Appropriate padding and positioning should be ensured to mitigate risks associated with skeletal deformities.5
Postoperative Management
- Airway complications:
- Clinicians should monitor closely for airway obstruction due to postoperative swelling or hematomas.
- A planned intensive care unit admission for high-risk cases should be considered.5
- Neurological and pain management:
- Clinicians should assess for neurological deterioration postoperatively, especially in NF2 patients with CNS involvement.
- A comprehensive pain management plan should be developed, as chronic pain is a common concern in NF patients.5,6
- Cardiovascular monitoring:
- Monitoring should be continued for hemodynamic instability, particularly in patients with pheochromocytomas or vascular anomalies.
- Clinicians should ensure that antihypertensive therapy is optimized.5,9
References
- Ferner RE, Gutmann DH. Neurofibromatosis type 1 (NF1): diagnosis and management. Handb Clin Neurol. 2013; 115:939-55. PubMed
- Evans DG. Neurofibromatosis type 2 (NF2): diagnosis and management. Handb Clin Neurol. 2013; 115:957-967. PubMed
- Plotkin SR, Messiaen L, Legius E et al. Updated diagnostic criteria and nomenclature for neurofibromatosis type 2 and schwannomatosis: An international consensus recommendation. Genet Med. 2022;24(9):1967-77. PubMed
- Tamura R. Current understanding of neurofibromatosis Type 1, 2, and schwannomatosis. Int J Mol Sci. 2021;22(11):5850. PubMed
- Korf BR, Lobbous M, Metrock LK. Neurofibromatosis type 1 (NF1): Pathogenesis, clinical features, and diagnosis. In: Post T(ed). UpToDate. 2024. Accessed April 6, 2025. Link
- Brown R. Management of central and peripheral nervous system tumors in patients with neurofibromatosis. Curr Oncol Rep. 2023;25(12):1409-17. PubMed
- Gross AM, Singh G, et al. Association of plexiform neurofibroma volume changes and development of clinical morbidities in neurofibromatosis 1. Neuro Oncol. 2018;20(12):1643-51. PubMed
- Zipfel J, Al-Hariri M, Gugel I, et al. Surgical management of peripheral nerve sheath tumours in children, with special consideration of neurofibromatoses. Childs Nerv Syst. 2020 ;36(10):2433-42. PubMed
- Hirsch NP, Murphy A, Radcliffe JJ. Neurofibromatosis: clinical presentations and anaesthetic implications. Br J Anaesth. 2001;86(4):555-64. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.