Copy link
Mucopolysaccharidoses
Last updated: 01/17/2023
Key Points
- Mucopolysaccharidoses (MPS) are rare, inherited lysosomal storage diseases with multisystem involvement.
- Both mask ventilation and laryngoscopy are often difficult in MPS patients. Patients with MPS I, II, and VI are more likely to present airway difficulties.
- Direct laryngoscopy attempts must be limited in patients with MPS, and alternative intubation techniques must be used early.
Introduction
- MPS are rare, inherited lysosomal storage diseases characterized by deficiencies in 11 different lysosomal enzymes involved in the metabolism of glycosaminoglycans (GAGs), previously known as mucopolysaccharides.1
- MPS are characterized by progressive, widespread accumulation of partially degraded GAGs in the lysosomes of various tissues and organs. The characteristic patterns of accumulation form the basis of MPS classification into seven types of progressive MPS diseases. MPS can be grouped into 4 categories based on their dominant clinical features.1
1. MPS I (Hurler), II (Hunter), and VII (Sly) affect soft tissue storage and the skeleton with or without brain disease.
2. MPS VI (Maroteaux – Lamy) affects both soft tissues and the skeleton.
3. MPS IVA, IVB (Morquio A, B) are primarily associated with skeletal disorders, and
4. MPS III A-D (Sanfilippo A-D) are primarily associated with progressive CNS disorders.
- MPS are inherited in an autosomal recessive pattern, meaning that only individuals inheriting the defective gene from both parents are affected. The only exception is MPS II or Hunter syndrome, which is inherited as X-linked recessive, where the mother passes along the defective gene to her son.
- MPS patients are frequently scheduled for surgical procedures with anesthesia1
- An MPS I registry (n=544) showed at least one surgical procedure in 75% of patients, with a median of three to four surgeries per patient.1
- The Hunter Outcome survey (n=527) reported that 83.7% of MPS II patients required surgical intervention at some point.1
Pathophysiology
- GAGs are long, linear polysaccharides consisting of repeating disaccharide units attached to a protein core (Figure 1). GAGs are hydrophilic, highly polar, and are present in lubricant fluid in joints and also help maintain tissue hydration. GAGs are also present as a surface coating on cells to help bind growth factors and as building blocks for bone, cartilage, connective tissue, etc.
- MPS patients either have a quantitative or qualitative defect in one of the 11 enzymes required to break down GAGs, resulting in the accumulation of the substrates in cells, blood, and connective tissues.1,2
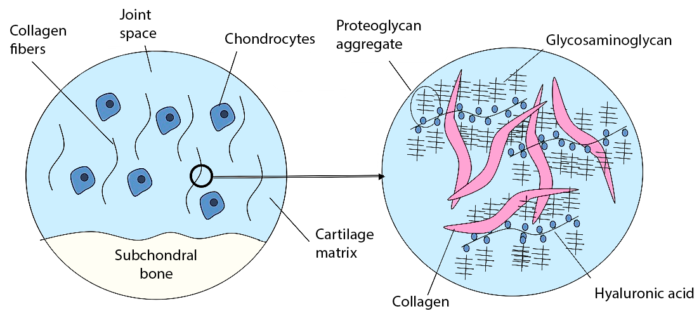
Figure 1. Glycosaminoglycans Source: Wikimedia Commons, Mfigueiredo, CC BY-SA 3.0
Clinical Presentation
Airway Abnormalities
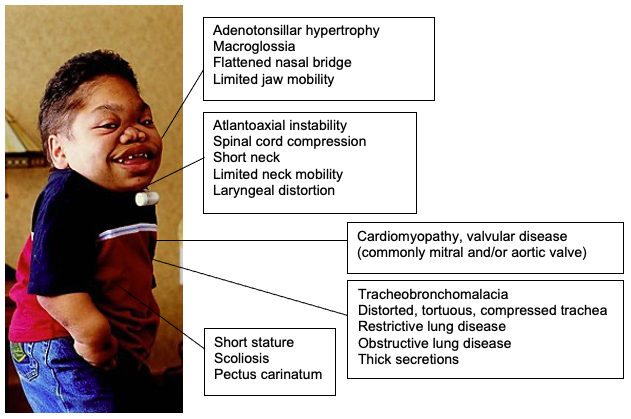
- GAG accumulation in the upper airways results in progressive hypertrophy of adenoids, tonsils, tongue, soft tissues of the larynx, and pharynx.1,2
- The trachea becomes knotty, tortuous, narrow and prone to tracheobronchomalacia.
- Skeletal abnormalities include (Figure 2)
- mandibular abnormalities
- limited jaw opening
- abnormal cervical vertebrae
- short neck
- atlantoaxial instability
- high anterior larynx
- flattened nasal bridge
- pectus carinatum
- scoliosis, etc.
- GAG accumulation in the larynx can impede the identification of the glottis.
- Excessively thick secretions throughout the upper and lower airways can worsen airway obstruction.2
- Obstructive sleep apnea (OSA) occurs in more than 80% of MPS patients.2 The degree of snoring or airway obstruction while sleeping must be evaluated preoperatively. MPS patients who have a history of severe OSA are at high risk of airway emergencies during anesthesia.
Pulmonary Abnormalities
- MPS patients often develop concomitant restrictive lung disease from thoracic scoliosis, decreased diaphragmatic excursion from hepatosplenomegaly, and decreased neuromuscular function.2
- Obstructive lung disease and recurrent lung infections are also common.
- Reactive airway disease is common, and even minor upper respiratory infections can trigger an exaggerated response resulting in severe respiratory failure and respiratory arrest.2
Spinal Cord Compression
- Spinal canal narrowing at the cervicocranial and thoracolumbar regions in patients with MPS I, II, IV, and VI can cause spinal cord compression.2
- Patients with MPS, I, IV (Morquio), and VI are at risk for atlantoaxial instability due to odontoid hypoplasia.2
- Therefore, preoperatively a detailed neurological examination should be performed. Results of imaging studies (flexion/extension plain films, CT scan or MRI) should be evaluated.
- Manual in-line stabilization of the head and neck should be used during airway management.
Cardiac Abnormalities
- Valvular heart disease from GAG accumulation can result in valvular regurgitation and/or stenosis. Mitral and aortic regurgitation are the most common lesions.2
- Systolic and diastolic dysfunction is common resulting in congestive heart failure and cardiomyopathy.2
- Arrhythmias and heart blocks in MPS patients have been described.
- Early onset, diffuse coronary artery disease has also been reported.
- MPS patients with untreated OSA may develop pulmonary hypertension from chronic hypoxemia.2
Neurologic Abnormalities
- Communicating hydrocephalus is a common feature of MPS I, II, III, VI, and VII. GAG accumulation can cause engorgement of arachnoid granulations, thereby limiting the absorption of cerebrospinal fluid, resulting in increased intracranial pressures.
- Cognitive impairment and developmental delays can impede cooperation with preoperative evaluation and diagnostic testing.
Age
- MPS patients become more difficult to intubate as they get older. In a single-center retrospective review of 128 anesthetics, patients older than 18 years were nearly 13 times more difficult to intubate than the controls.3 However, mask ventilation and supraglottic airways (SGA) placement did not get progressively more difficult in the older patients.
Treatment
- Enzyme replacement therapy (ERT) and/or hematopoietic stem cell transplant (HSCT) have the potential to decrease GAG deposition and accumulation. Patients who have undergone therapies may not have age-related progression of airway difficulty.
- HSCT initiated prior to 2 years of age in MPS I patients decreases the incidence of difficult mask ventilation and intubation.4
- ERT initiated late in the course of MPS II and VI patients improved upper airway patency but did not reduce the incidence of difficult mask ventilation and intubation.4
Characteristic clinical features and treatment options for the different types of MPS syndromes are listed in Table 1.
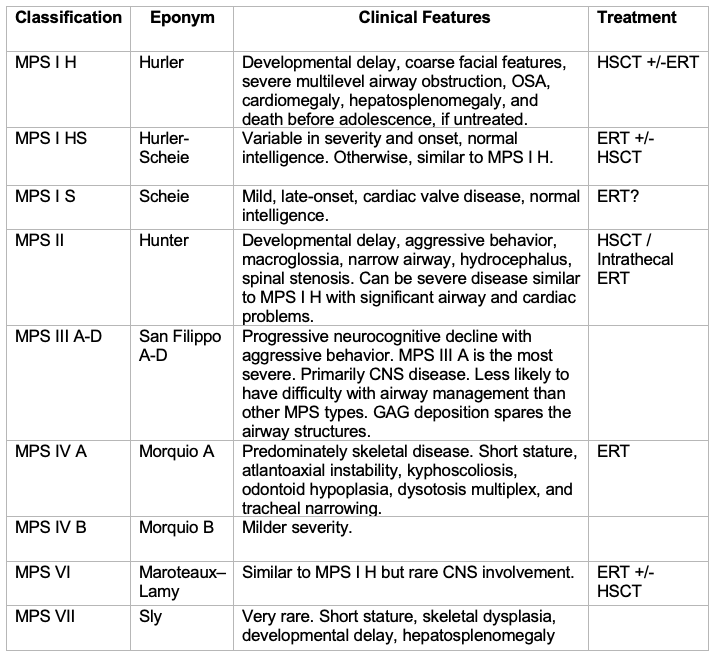
Table 1. Overview of MPS pathology and nomenclature including treatment options Abbreviations: MPS = Mucopolysaccharidoses, OSA = obstructive sleep apnea, CNS = central nervous system, GAG = glycosaminoglycans, ERT = enzyme replacement therapy, HSCT = hematopoietic stem cell therapy. Adapted from Walker R, et al. Anaesthesia and airway management in mucopolysaccharidosis. J Inherit Metab Dis. 2013;36(2):211-9.2
Anesthetic Considerations
- Surgical procedures in patients with MPS are associated with a high perioperative mortality rate. A study comprising 932 patients enrolled in the MPS I registry that underwent a total of 4,762 procedures showed a 30-day risk of death/procedure of 0.7% and a death/patient rate of 4.2%5
- Several serious anesthetic complications can occur in patients with MPS.2
- Inability to mask ventilate or intubate, necessitating a tracheostomy.
- Complete airway obstruction during induction or extubation can cause profound hypoxemia and cardiac arrest.
- Temporary airway obstruction can cause negative-pressure pulmonary edema.
- Postoperative problems include stridor and the need for reintubation or tracheostomy.
- MPS patients must be considered to have difficult airways. Both mask ventilation and intubation can be difficult. In two case series, difficulty with mask ventilation ranged from 7-14%.1
- The overall incidence of difficult tracheal intubation ranges widely. The incidence of difficult intubation in a review of 17 patients undergoing 141 anesthetics was the following.4
- 12% in MPS I
- 35% MPS II
- 86.7% in MPS VI
- 0% in MPS III and IV
- Patients with MPS I, II, and VI are more likely to present airway difficulties during anesthesia.4 The incidence of difficult intubation in children with MPS II is twenty times more frequent than in children of a similar age or weight.4
- An exception is MPS III patients, who are typically not difficult to intubate. GAG deposition spares the airway structures.
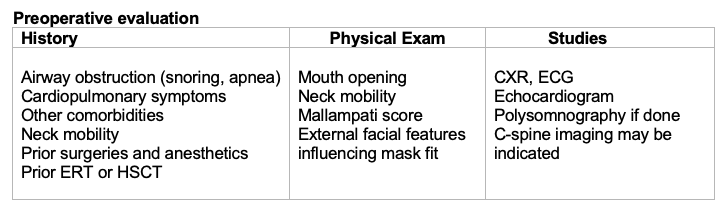
Table 2. Preoperative assessment of MPS patients.
Preoperative Set-Up
- Anticipate difficult mask ventilation due to multilevel upper airway obstruction
- Nasopharyngeal airways (NPA), oropharyngeal airways (OPA)
- SGAs
- Two experienced providers for bag-mask ventilation
- Anticipate difficult direct laryngoscopic view
- Fiberoptic bronchoscope
- Videolaryngoscope
- SGA designed to facilitate tracheal intubation (“intubating LMA”)
- Anticipate cannot-intubate, cannot-ventilate scenario
- Discuss with ENT surgeons as appropriate
- Confirm availability of emergency tracheostomy kit
- Ensure availability of sugammadex if rocuronium or vecuronium is used for paralysis
Induction/Airway Management
- Consider topicalization of the airway with a local anesthetic
- Consider preinduction peripheral intravenous line placement
- Awake placement of NPA can be a helpful adjunct
- Maintain spontaneous ventilation until ability to mask ventilate is confirmed
- Consider using SGA if mask ventilation is difficult
- If direct laryngoscopy is attempted for intubation, it should be done by the most experienced laryngoscopist, and it should be limited to one or two attempts.
- Consider using alternative intubation methods such as video laryngoscopy, flexible bronchoscopic intubation (FBI) or FBI through an SGA early.
- Use supplemental oxygen during intubation attempt
Special Considerations
- Manual in-line stabilization must be maintained in MPS patients with unstable necks.2
- Neurophysiologic monitoring with somatosensory evoked potentials and motor evoked potentials should be considered in MPS patients undergoing spinal surgery or at risk for spinal cord compression during longer surgeries or those requiring neck movement.2
References
- Clark BM, Sprung J, Weingarten TN, et al. Anesthesia for patients with mucopolysaccharidoses: Comprehensive review of the literature with emphasis on airway management. Bosn J Basic Med Sci. 2018;18(1):1-7. PubMed
- Walker R, Belani KG, Braunlin EA, et al. Anaesthesia and airway management in mucopolysaccharidosis. J Inherit Metab Dis. 2013;36(2):211-9. PubMed
- Madoff LU, Kordun A, Cravero JP. Airway management in patients with mucopolysaccharidoses: The progression toward difficult intubation. Paediatr Anaesth. 2019 ;29(6):620-7. PubMed
- Frawley G, Fuenzalida D, Donath S, et al. A retrospective audit of anesthetic techniques and complications in children with mucopolysaccharidoses. Paediatr Anaesth. 2012;22: 737-44. PubMed
- Arn P, Whitley C, Wraith JE, et al. High rate of postoperative mortality in patients with mucopolysaccharidosis I: findings from the MPS I Registry. J Pediatr Surg. 2012 Mar;47(3):477-84. PubMed
Other References
- Hylton JRE, Laochamroonvorapongse D. Mucopolysaccharidoses: Clinical features and considerations for anesthetic and perioperative care. SPA Newsletter. Society for Pediatric Anesthesia. Accessed February 6, 2023. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.