Copy link
Monitored Anesthesia Care
Last updated: 01/16/2024
Key Points
- Monitored anesthesia care (MAC) is a service in which a licensed anesthesia provider (physician anesthesiologist, anesthesiologist assistant, or certified registered nurse anesthetist) is continually focused on patient sedation, comfort, maintenance of vital signs, and safety before, during, and after the procedure.
- The continuum of sedation is a tool that delineates levels of consciousness on a scale defined by physiologic parameters attributable to the amount of sedation administered. The continuum is used to evaluate and maintain a desired level of sedation.
- To achieve the optimal levels of patient sedation, comfort, and safety seen in MAC, a licensed anesthesia provider must employ careful surveillance with various specialized monitors as well as a sensibly tailored combination of pharmaceutical agents.
The Continuum of Sedation
- The continuum of sedation delineates levels of consciousness on a stepwise scale as defined by physiologic parameters attributable to the amount of sedation used. The scale begins with the lightest level of sedation at minimal sedation anxiolysis and ends with the deepest level of sedation, general anesthesia (Figure 1).
- Each stage of the continuum is defined by a specific set of physiologic parameters related to the patient’s ability to respond to stimulus, protect their airway under their own power, breathe spontaneously, and maintain adequate cardiac perfusion.
- These parameters allow clinicians to evaluate and maintain the respective level of sedation required for a case and optimize safety, comfort, and operational efficiency.
- As sedation increases, the patient moves along the continuum and will require increasing amounts of support due to the physiologically depressive nature of the pharmaceutical agents used.
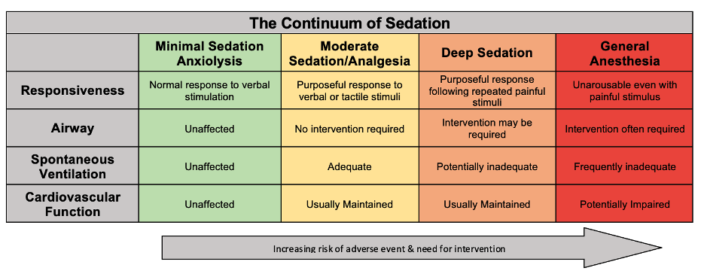
Figure 1. The continuum of sedation. Adapted from the Committee on Quality Management and Departmental Administration & the American Society of Anesthesiologists.1
- The Modified Observer Assessment of Alertness and Sedation (MOAA/S) scale and Ramsay sedation scale are other tools used to monitor sedation status through direct assessment of the patient’s level of responsiveness.2
- The MOAA/S (nor other tools used to evaluate sedation, such as the Ramsay scale) is not regularly used in clinical practice but more often as a tool to aid in research or track data for studies.3 The MOAA/S scale corresponds to the continuum of sedation as illustrated below (Figure 2).
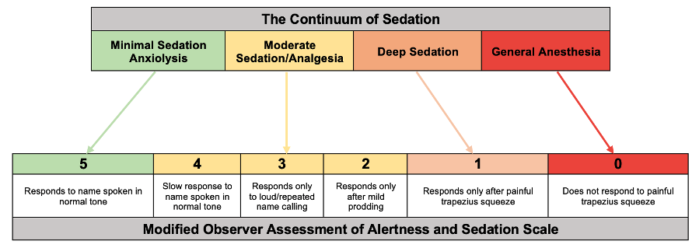
Figure 2. Modified observer assessment of alertness and sedation scale. Adapted from Kim H, et al. Reg Anesth Pain Med. 2023.2
Monitored Anesthesia Care Overview
- MAC is an anesthesia service in which a physician anesthesiologist or other licensed anesthesia provider (anesthesiologist assistant, anesthesiologist assistant, or certified registered nurse anesthetist) provides constant supervision to a patient while also focusing on patient anxiolysis, comfort, maintenance of vital signs, and safety. MAC can be performed under any depth of sedation, and the anesthesia provider must be prepared to convert to general anesthesia if necessary.
- The advantages of MAC over other forms of sedation – such as procedural sedation provided by nonanesthesia clinicians – are due to the advanced training of the anesthesia provider and continuous focused monitoring that allows for optimized patient safety and comfort.4
- The American Society of Anesthesiologists (ASA) emphasizes how MAC offers the ability to attend to a patient’s clinical and psychological needs beyond what can be provided by a proceduralist – who must split their attention between performing the case and sedating the patient – or other clinical personnel who lack the training of an anesthesiologist. Because of this, patients not undergoing MAC cannot be safely sedated past a point where they can no longer spontaneously breathe.5
- The ability to adjust sedation levels from full consciousness to general anesthesia during a procedure while maintaining cardiopulmonary function allows MAC the flexibility and control to achieve ideal procedural conditions.5
- Standard ASA monitors are required for all MAC cases – as for any administration of anesthesia – including noninvasive blood pressure, pulse oximetry, end-tidal CO2, electrocardiography, and temperature monitoring.6
- The bispectral index is an additional optional monitor that uses a processed electroencephalogram to measure brain activity and determine the patient’s level of consciousness and, thus, their depth of sedation.
- Continual evaluation of the patient’s response to external stimuli must be done to ensure patients are at the desired level of sedation per the MOAA/S scale. This includes responses to verbal and nonverbal stimuli.
Preprocedure Evaluation
- A standard preprocedure evaluation should be completed for every patient undergoing MAC, just as it would for any patient undergoing anesthesia.
- The preprocedure evaluation should focus on assessing the patient’s ability to remain still and maintain physiologic homeostasis during the procedure. The inability to remain still for a prolonged period is often due to anxiety or chronic cough secondary to orthopnea or obstructive pulmonary disorders.
- Other less common contraindications include, but are not limited to, structural airway abnormalities (congenital anomalies such as laryngomalacia or Pierre Robin syndrome), hemodynamic instability, altered sensorium, or simple refusal of consent.7
Technique & Pharmacology
- MAC can include the administration of medications to induce a combination of anxiolytic, hypnotic, analgesic, and amnestic effects in the patient. These are usually administered intravenously.
- An optimal combination of pharmaceutical agents will allow for the desired effects (anxiolysis, hypnosis, analgesia, and amnesia) to occur in the least amount of time required, with the lowest incidence of postoperative nausea and vomiting (PONV) or lingering cardiovascular and respiratory depression.
- Achieving an optimal level of sedation requires accurate dosing from a trained, licensed professional to achieve consistent sedation while minimizing negative side effects.
- Propofol
- Indication: sedation, hypnosis, mild amnesia
- Propofol enhances gamma-aminobutyric acid (GABA) activity and is a preferred agent for sedation and hypnosis due to its short half-life and low incidence of PONV. This results in a rapid onset and offset and makes for easy titration, even in ambulatory settings.
- While propofol does produce amnesia at subhypnotic doses, it is not a main indication for use, nor does it have analgesic properties.
- Fospropofol has the same properties as propofol, with the exception that it is a proform of propofol and thus has a longer half-life.
- Dexmedetomidine
- Indication: sedation, hypnosis, analgesia
- Dexmedetomidine induces sedation through alpha-2 agonism, decreasing sympathetic outflow and providing analgesia. It can also mitigate emergence agitation, making it a popular choice of sedative in pediatric populations.
- Dexmedetomidine alone does not provide amnestic effects.
- Benzodiazepines
- Indication: anxiolysis, amnesia, hypnosis
- Benzodiazepines, such as midazolam and diazepam, are mainly used for their anxiolytic and amnestic properties through their facilitation of GABA receptor binding. At high doses, these drugs can be used for hypnosis but are not as reliable as propofol or dexmedetomidine and can cause psychomotor impairment after sedation.
- Remimazolam is a short-acting benzodiazepine that is expanding use for MAC sedation, which relies on inactivation by nonspecific tissue esterase, enabling rapid onset/offset with a predictable duration of action.8
- Opioids
- Indication: analgesia
- Opioids, the most common MAC agents being fentanyl or remifentanil, act on Mu receptors to induce analgesia and are often used in combination with benzodiazepines to induce a blend of analgesia, anxiolysis, and amnesia.
- Ketamine
- Indication: analgesia, sedation, amnesia
- Ketamine produces a blockade of N-methyl D-aspartate receptors to induce powerful analgesia and a dissociative state of sedation and amnesia. Ketamine is frequently combined with benzodiazepines to reduce hallucinations but runs the risk of increasing oral secretions, making airway management difficult.
Complications
- The adverse outcomes of MAC are the same and can occur in any instance of sedation and depend on factors related to depth of sedation, drugs used, equipment available, and patient demographics.
- Common complications include hypoxemia and hypercarbia secondary to respiratory depression or hypotension and arrhythmias secondary to cardiac ischemia or compromise.
- Local anesthetic systemic toxicity (LAST) syndrome, while rare (estimated incidence of 0.03%), is a life-threatening complication secondary to the accidental systemic absorption of a local anesthetic used for a nerve block procedure.9
- The presentation of LAST is atypical, but most cases involve seizures that occur within minutes to hours of local anesthetic administration and can be accompanied by perioral paresthesia, dysgeusia, agitation, confusion, or altered levels of consciousness.9
- Some studies have shown MAC rates of complications to be higher than proceduralist driven sedation, especially regarding respiratory depression and the need for intubation.10
- Many patients who undergo MAC are older and sicker, and procedures are often performed in out-of-operating room settings. These populations require the expertise and continued surveillance of MAC but simultaneously possess a greater predisposition to complications and adverse outcomes.3
References
- Committee on Quality Management and Departmental Administration. Statement on continuum of depth of sedation: Definition of general anesthesia and Levels of sedation/analgesia. American Society of Anesthesiologists. Published, October 13, 1999. Updated, October 23, 2019. Accessed October 14, 2023. Link
- Kim H, Kim Y, Bae J, et al. Comparison of remimazolam and dexmedetomidine for intraoperative sedation in patients undergoing lower extremity surgery under spinal anesthesia: A randomized clinical trial. Reg Anesth Pain Med. 2023. PubMed
- Rosero, E.B., Monitored anesthesia care in adults. In: Post T, ed. UpToDate; 2023. December 12, 2023. Link
- Sohn H, Ryu J. Monitored anesthesia care in and outside the operating room. Korean Journal of Anesthesiology. 2016; 69(4): 319-26. PubMed
- Committee on Economics. Statement on Distinguishing Monitored Anesthesia Care (“MAC”) from Moderate Sedation/Analgesia (Conscious Sedation). American Society of Anesthesiologists. Published October 18, 2023. Updated October 18, 2023. Accessed December 12, 2023. Link
- Committee on Standards and Practice Parameters. Standards for Basic Anesthetic Monitoring. American Society of Anesthesiologists. Published October 21, 1986. Updated December 13, 2020. Accessed November 16, 2023. Link
- Green SM, Krauss B. Procedural sedation and analgesia. In: Baren JM, Rothrock SG, Brennan JA, Brown L. Pediatric Emergency Medicine. Elsevier; 2008:1119-3.
- Kim KM. Remimazolam: pharmacological characteristics and clinical applications in anesthesiology. Anesth Pain Med (Seoul). 2022;17(1):1-11. PubMed
- El-Boghdadly, K., Pawa, A., Chin, K.J. Local Anesthetic systemic toxicity: current perspectives. Local and Regional Anesthesia. 2018; 11: 35-44. PubMed
- Agostoni, M., Fanti, F., Gemma, M., Pasculli, N., Beretta, L., Testoni, P.A. Adverse events during monitored anesthesia care for GI endoscopy: An 8-year experience. Gastrointest Endosc 2011 Aug; 74(2):266-75. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.