Copy link
Mitral Stenosis: Hemodynamic Management, Comorbidities, and Treatment
Last updated: 10/15/2025
Key Points
- Intraoperative hemodynamic management of patients with mitral stenosis (MS) involves maintaining a normal sinus rhythm, ensuring adequate preload/euvolemia, avoiding tachycardia (maintaining a low normal heart rate), increasing contractility, and keeping afterload within normal limits.
- MS may be associated with rheumatic heart disease or senile calcific degeneration.
- Patients with MS are at an increased risk for atrial fibrillation (AF), congestive heart failure (CHF), pulmonary hypertension, and embolic events.
- Management of MS includes percutaneous mitral balloon commissurotomy (PMBC), surgical commissurotomy (open or closed), as well as mitral valve replacement (MVR).
- Medical management involves preventing embolic events and atrial dysrhythmias through anticoagulation therapy (typically vitamin K antagonists) and rate- and/or rhythm-control medications.
Hemodynamic Management
- MS is defined as a reduction in the mitral valve (MV) orifice area from pathologic leaflet changes secondary to congenital MS (rare), rheumatic heart disease, from streptococcal infection (most common), or degenerative disease (annular calcification).
- MS prevents normal left atrial (LA) emptying into the left ventricle (LV), resulting in reduced stroke volume and a fixed cardiac output due to limited LV filling.
- Over time, MS can lead to pulmonary hypertension and right heart dysfunction. MS → ↑ LA pressures → ↑ pulmonary venous pressures → pulmonary arterial hypertension → right ventricular dysfunction.1,2
- Patients may also develop LV dysfunction as a result of reduced preload from limited filling and increased afterload from reflex vasoconstriction. However, in patients with severe rheumatic heart disease, inflammation may also contribute to contractile impairment.3
- Please refer to the OA summary “Mitral Stenosis: Etiology, Pathophysiology, and Symptomatology” for more detailed information. Link
- Table 1 highlights the hemodynamic goals in patients with MS.
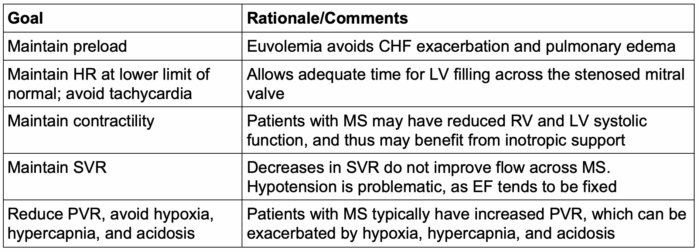
Table 1. Hemodynamic goals in MS. Abbreviations: CHF, congestive heart failure; HR, heart rate; SVR, systemic vascular resistance; EF, ejection fraction; PVR, pulmonary vascular resistance; RV, right ventricular; LV, left ventricular.
Associated Comorbidities
- MS leads to left atrial dilation, which puts patients at increased risk of developing atrial dysrhythmias, particularly AF. More than 40% of patients with MS develop AF.
- Patients who develop AF are also at a higher risk of forming a left atrial appendage thrombus and, hence, embolic events.
- Other conditions to consider in patients with MS-like symptoms include congenital valvular diseases as well as carcinoid tumors and atrial myxomas.
Medical Treatment of MS
- Patients who present with CHF from MS are likely to present with signs of volume overload and should be treated with diuretics.
- In patients with rheumatic MS and AF, there is an increased risk of arterial embolic events from left atrial thrombus formation; anticoagulation decreases the incidence of these thromboembolic events, including in patients with a history of prior embolic events or visualized LA thrombus.
- The American College of Cardiology, American Heart Association, and Heart Rhythm Society recommend vitamin K antagonists for anticoagulation in patients with MS and AF.4
- There is limited data on the efficacy of direct oral anticoagulants in patients with AF and moderate to severe MS.
- The INVICTUS trial found that compared to rivaroxaban, vitamin K antagonists had a lower rate of cardiovascular events and death.5
- In symptomatic patients with MS who are in normal sinus rhythm and have tachycardia, heart rate control with beta blockers, calcium channel blockers, or ivabradine will lengthen the diastolic filling period and lower LA pressure.
- Routine use of heart rate control and anticoagulation medications for patients with rheumatic MS in normal sinus rhythm is controversial.
- AF with rapid ventricular response limits diastolic filling time and increases LA pressures, leading to LA dilation. Hence, timely management of AF with anticoagulation, heart rate response control with negative dromotropic agents or cardioversion may be necessary to improve hemodynamics.
Surgical Treatment of MS
- For some patients, medical management does not improve symptoms. Some patients with the appropriate valve morphology can qualify for surgical options including PMBC, MV commissurotomy or MVR.
- PMBC is performed by advancing one or more balloon catheters across the MV and inflating them, thereby splitting the commissures (Figure 1). It is performed in patients with symptomatic moderate to severe MS, New York Heart Association class 2 to 4, and a lack of commissural calcification. Contraindications for the procedure include mitral regurgitation, left atrial thrombus, concomitant tricuspid stenosis or regurgitation, or severe coronary artery disease.6
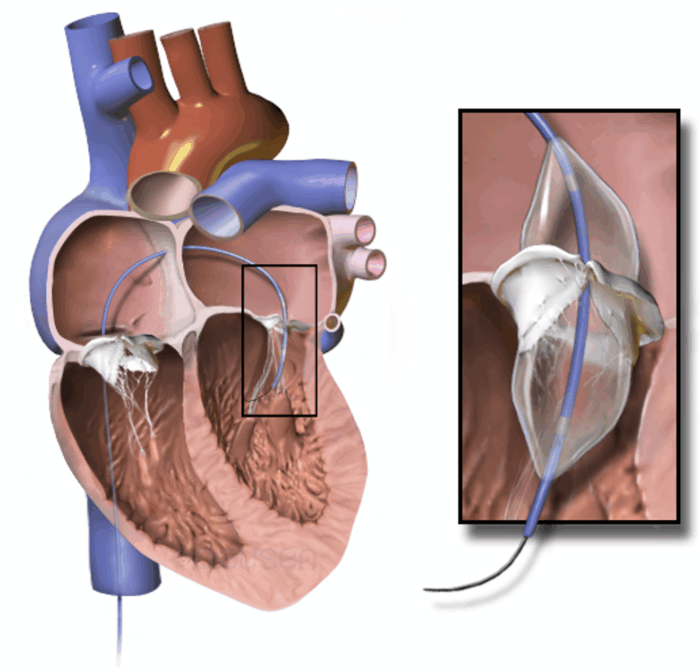
Figure 1. Percutaneous mitral balloon commissurotomy. Guidewire is inserted through the femoral vein to the inferior vena cava and right atrium, across the interatrial septum, and to the left atrium. The balloon is subsequently placed across the mitral valve. Source: Wikimedia Commons. Blausen Medical Communications, Inc. CC by SA. Link
- Surgical commissurotomy can be performed either closed (where the valve is opened blindly through the LA or LV), or open (which allows more extensive surgery under direct visualization), depending on the patient’s anatomy. However, in the presence of severe valvular thickening and sub-valvular fibrosis with leaflet tethering, MVR may be the best option.
- MVR is indicated in patients with calcified MS, where the calcification involves the annulus and base of the leaflets without commissural fusion; in these cases, there is no role for PMBC or surgical commissurotomy. Patients with rheumatic MS with severe valvular thickening and sub-valvular fibrosis with leaflet tethering are appropriate candidates.
- MVR for patients with severe mitral annular calcification (MAC) can be technically complex due to difficulties in sizing and securing the prosthetic valve. Patients with MAC are often elderly and frail and thus require medical optimization and other therapies prior to undergoing surgical management.
References
- Herrera A. Valvular heart disease. Stoelting's Anesthesia and Co-Existing Disease. 2008:27-42.
- Holmes K, Gibbison B, Vohra HA. Mitral valve and mitral valve disease. BJA Education. 2017;17(1):1-9. Link
- Carabello BA. Modern management of mitral stenosis. Circulation. 2005; 112(3):432-7. PubMed
- Joglar JA, Chung MK, Armbruster AL, Benjamin EJ, et al. 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2024;149(1):e1-e156. PubMed
- Connolly SJ, Karthikeyan G, Ntsekhe M, Haileamlak A, et al. Rivaroxaban in rheumatic heart disease-associated atrial fibrillation. N Engl J Med. 2022;387(11):978-988. PubMed
- Nishimura RA, Otto CM, Bonow RO, Carabello BA, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(22):e57-185. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.