Copy link
Management of Patients with Acute Respiratory Distress Syndrome
Last updated: 10/22/2025
Key Points
- The central tenets of ventilator management in patients with acute respiratory distress syndrome (ARDS) include low tidal volume ventilation with no more than 4-6cc/kg of the patient’s ideal body weight, permissive hypercapnia, and avoiding high driving pressures.
- Prone positioning has a mortality benefit in ARDS patients with a PaO2/FiO2 ratio (the ratio of partial pressure of oxygen in arterial blood to the fraction of inspired oxygen) lower than 150 mmHg, requiring positive end-expiratory pressure (PEEP) greater than 5 mmHg, and an FiO2 greater than 0.6.
- Other therapies, including inhaled nitric oxide (iNO), corticosteroids, neuromuscular blocking agents, and extracorporeal membrane oxygenation (ECMO), should be considered on a case-by-case basis.
- Many treatments that improve oxygenation in patients with ARDS do not lead to improved mortality and should therefore be used cautiously.
Introduction
- Although the primary treatment approach for ARDS is supportive therapy, numerous clinical studies have been conducted to identify the most effective treatment strategies and achieve successful outcomes. Therefore, it is worth highlighting certain clinical studies that have shown positive results, as well as pointing out those that require further study, along with those that have demonstrated a negative impact on patients with ARDS.
Treatment of ARDS Patients: Recommended Therapies
Low Tidal Volume Ventilation
- In patients with ARDS, mechanical ventilation with a tidal volume of 6 cc/kg of ideal body weight resulted in a significant decrease in mortality compared with 12cc/kg of ideal body weight.1
- Low tidal volume ventilation with permissive hypercapnia reduces the risk of barotrauma and ventilator-associated lung injury.
Reduce Driving Pressure
- Driving pressure (ΔP) is considered a key factor in predicting outcomes in mechanically ventilated patients, especially those who are not actively breathing. This is because respiratory system compliance, which reflects how easily the lungs can expand, is closely related to the amount of functional, aerated lung tissue remaining during the disease.
- Unlike tidal volume or PEEP alone, driving pressure takes into account lung compliance, making it a more accurate indicator of the stress placed on the lungs. It essentially normalizes tidal volume to lung size, providing a clearer picture of the pressure required to inflate the lungs.
- Driving pressure can be calculated in two ways:
- i. ΔP = Tidal Volume ÷ Compliance, or
- ii. ΔP = Plateau Pressure − PEEP (in passively ventilated patients).
- Research has shown that lower driving pressures are strongly associated with better survival.2
Prone Positioning
- In ARDS patients with a PaO2/FiO2 ratio lower than 150 mmHg, and with PEEP greater than 5 cmH2O and FiO2 greater than 0.6, prone positioning for 16 hours per day significantly decreased 28-day and 90-day mortality.3
- Prone positioning can improve oxygen levels in the lungs by allowing better ventilation-perfusion matching and reducing pressure on the lungs from other organs. The prone sessions should be continued until the patient’s oxygenation improves (PaO2/FiO2 greater than 150 mmHg with PEEP lower than 10cm of water and FiO2 lower than 0.6).
Conservative Fluid Management
- In a study comparing liberal with conservative fluid management in ARDS, patients randomized to conservative fluid therapy with a net even fluid balance were compared with patients randomized to a liberal fluid strategy with a net positive 7 liters fluid balance.
- Conservative fluid management resulted in improved oxygenation, more ventilator-free days, and reduced intensive care unit (ICU) length of stay.
- Patients randomized to conservative fluid management did not have an increase in non-pulmonary organ failure.
- There was no difference in mortality between groups.4
Treatment of ARDS Patients: Therapies to Consider
Use of Neuromuscular Blocking Agents
- A systematic review and meta-analysis found that neuromuscular blocking agents provide benefit in patients with ARDS by increasing recruitment, improving oxygen delivery, and reducing oxygen consumption. By paralyzing patients, ventilator asynchrony is minimized which reduces ventilator-induced lung injury (VILI) and decreases circulating inflammatory mediators.5
- Neuromuscular blocking agents have not been consistently found to have a mortality benefit. In patients with moderate to severe ARDS, the early use of neuromuscular blocking agents decreases 22-28-day mortality but does not improve 90-day mortality.
- Risks of neuromuscular blocking agents include ICU myopathy, which can significantly prolong recovery. It is therefore recommended to utilize these agents for 48 hours or less.
Corticosteroids
- Corticosteroids may reduce mortality and increase ventilator-free days in some populations with ARDS; however, due to the heterogeneity of the disease, corticosteroids have not been found to be universally beneficial. The underlying cause of ARDS influences the likelihood of the patient responding to corticosteroids.
- Steroids are recommended in patients with ARDS due to COVID-19. Patients with ARDS resulting from septic shock, bacterial pneumonia, or direct lung injury involving Pneumocystis jiroveci are more likely to benefit from corticosteroid therapy.
- A recent randomized controlled trial found that patients with moderate to severe ARDS defined as PaO2/FiO2<200 mmHg requiring at least PEEP of 10 and FiO2 0.5 had reduced duration of mechanical ventilation and a trend towards lower mortality when treated with intravenous dexamethasone for 10 days 6
- Patients with ARDS caused by H1N1 influenza may experience increased mortality when treated with corticosteroids.
- Consider risks associated with steroids including venous thromboembolism, hyperglycemia, gastrointestinal bleeding, bone fractures, ICU-acquired weakness, delirium, and an increased risk of sepsis.7
iNO
- A systematic review and meta-analysis concluded that iNO does not reduce hospital mortality in patients with ARDS, regardless of the severity of hypoxemia.
- In life-threatening situations where patients are at imminent risk of death from hypoxemia and have failed all other treatment options, a trial of iNO may be considered as a last resort.8
- There is some evidence that iNO may cause renal impairment; however, this is not definitive.
Extracorporeal Membrane Oxygenation (ECMO) for Severe ARDS
- Two major randomized controlled trials have evaluated the use of ECMO for treating patients with severe ARDS. Neither trial found a mortality benefit to ECMO compared with standard of care; however, there was an increased crossover from the control group to the ECMO group.
- ECMO should be considered in patients who have failed standard of care ARDS management.9,10
Mechanical Ventilation Guided by Esophageal Pressure
- Determining the optimal level of PEEP in patients with acute lung injury or ARDS has long been a challenge. One proposed strategy involves the use of an esophageal balloon catheter to estimate transpulmonary pressure, which is the difference between alveolar and pleural pressures.
- A randomized controlled study evaluating this approach showed that mechanical ventilation guided by esophageal pressure measurements significantly improved oxygenation and respiratory system compliance compared to standard care.11
- Utilizing esophageal pressure to determine optimal PEEP has not been associated with a mortality benefit.
Airway Pressure Release Ventilation (APRV)
- APRV is a mode of mechanical ventilation characterized by the application of continuous positive airway pressure with brief, intermittent pressure releases that allow partial exhalation. Unlike conventional modes, APRV permits spontaneous breathing throughout the high-pressure phase, and gives clinicians control over both inspiratory and expiratory times. This method is based on the “open lung” concept, aiming to maintain alveolar recruitment.
- While APRV has been associated with improved oxygenation, studies are limited and have heterogeneous results12
- This mode should be used with caution to avoid high tidal volumes and driving pressures, which have both been repeatedly associated with increased mortality in ARDS1,2
Treatment of ARDS Patients: Therapies to Avoid
High-Frequency Oscillatory Ventilation (HFOV)
- HFOV is a mechanical ventilation strategy that delivers very small tidal volumes at very high frequencies (up to several hundred breaths per minute) while maintaining a constant mean airway pressure to keep the lungs open. It was initially considered promising for severe ARDS, based on its potential to minimize VILI by preventing overdistension and atelectrauma.
- In a randomized controlled trial, HFOV was compared with conventional lung protective ventilation in adults with moderate to severe ARDS. The investigators found a trend toward higher mortality in the HVOF group, and the trial was terminated due to concerns for harm.
- Patients in the HFOV group additionally had more hemodynamic compromise than the conventional ventilation group, requiring more vasopressors.13
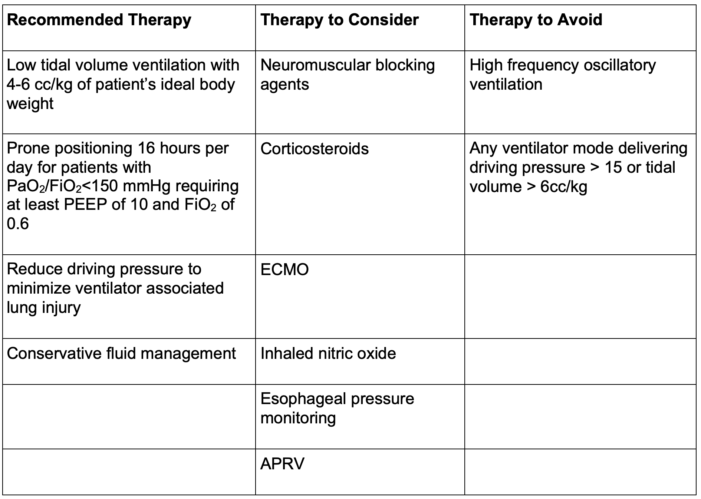
Table 1. Summary of ARDS treatment
References
- The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000; 342(18), 1301–8. PubMed
- Amato MBP, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372(8), 747–55. PubMed
- Guerin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23), 2159–68. PubMed
- National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wiedemann HP, Wheeler AP, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354(24):2564-75. PubMed
- Papazian L, Forel JM, Gacouin A, et al. (2010). Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med.2010;363(12), 1107-16. PubMed
- Villar J, Ferrando C, Martínez D, et al. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med. 2020;8(3):267-276. PubMed
- Hensley MK, Sjoding MW, Prescott HC. COUNTERPOINT: Should Corticosteroids Be Routine Treatment in Early ARDS? No. Chest. 2021;159(1):29-33. PubMed
- Gebistorf F, Karam O, Wetterslev J, Afshari A. Inhaled nitric oxide for acute respiratory distress syndrome (ARDS) in children and adults. Cochrane Database Syst Rev. 2016;2016(6):CD002787. PubMed
- Combes A, Hajage D, Capellier G, et al. Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Distress Syndrome. N Engl J Med. 2018;378(21):1965-1975. PubMed
- Peek GJ, Mugford M, Tiruvoipati R, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374(9698):1351-1363. PubMed
- Talmor D, Sarge T, Malhotra A, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med. 2008;359(20):2095-2104. PubMed
- Carsetti A, Damiani E, Domizi R, et al. Airway pressure release ventilation during acute hypoxemic respiratory failure: a systematic review and meta-analysis of randomized controlled trials. Ann Intensive Care. 2019;9(1):44. PubMed
- Ferguson ND, Cook DJ, Guyatt GH, et al. High-frequency oscillation in early acute respiratory distress syndrome. N Engl J Med. 2013;368(9):795-805. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.