Copy link
Magnetic Resonance Imaging Safety: Advanced
Last updated: 04/09/2024
Key Points
- Magnetic resonance imaging (MRI) requires the use of a strong magnetic field. Therefore, objects with ferromagnetic properties are dangerous. Patients undergoing MRI require comprehensive screening examinations to ensure implants and devices are MR-safe.
- Technological advancement has led to the incorporation of MRI scanners in the operating room (OR), which necessitates specific measures, including OR design and anesthesia considerations that must be taken to ensure patient and personnel safety.
- Reducing the amount of sedation during MRI promotes patient safety while obtaining high-quality, diagnostic studies. Some strategies include supportive programs, joint staff efforts, tools to enhance patient cooperation, prescanning familiarity, ambient optimization, and parallel imaging.
MRI Technology (or Principles)
- MRI produces detailed images by utilizing the body’s natural magnetic properties. The hydrogen nucleus, which is a single proton, has a north-south pole and spins on its axis. The hydrogen proton is utilized for MRI because of its abundance in water and fat.1
- Under normal conditions, the hydrogen protons spin on their axes within the body at random. However, when the body is placed in the strong magnetic field of the MRI scanner, the protons’ axes align, creating a magnetic vector oriented along the axis of the scanner.1
- When radio waves are added to the magnetic field, a magnetic vector is deflected. The strength of the magnetic field is altered using electric coils, and the different frequencies applied allow different slices of the body to resonate.
- When the radiofrequency source is turned off, the magnetic vector returns to its resting state, and a signal is emitted, which is used to create magnetic resonance (MR) images. Receiver coils around the target body part detect the emitted signals, which are subsequently plotted on a greyscale, and cross-sectional images are produced.1
Radiofrequency Pulses
- Multiple radiofrequency pulses can be utilized in sequence to highlight tissue types due to the properties by which the protons of different tissues relax at different rates.1
- T1 relaxation images: Generated based on the time required for the magnetic vector to return to its resting state.
- T2 relaxation images: Generated based on the time required for the axial spin to return to its resting state.
- MR images, therefore, comprise a series of pulse sequences that have different focuses because different tissues, such as fat and water, have different relaxation times that can be identified individually.
- MR imaging utilizes radiation in the radiofrequency range that is found all around us and does not damage tissues. Therefore, unlike X-ray or computed tomography scans, there are no biological hazards of MRI.1
Intraoperative MRI Safety
- MRI scanners have traditionally been used outside the OR for diagnostic imaging. However, technological advancement has led to the incorporation of MRI scanners in the OR, which have benefits in numerous surgical settings.
- Common surgical procedures that utilize intraoperative MRI (iMRI) include neurosurgical procedures such as the removal of spinal cord tumors, as well as surgeries involving abdominal organs such as the liver or kidneys.2
- During invasive neurologic procedures, brain shift occurs following the opening of the dura due to cerebrospinal fluid fluctuation and surgical manipulation.3 iMRI scans can be performed to determine progressive changes in lesions or surrounding tissues to detect complications.3
Operating Room Design
- An OR that is used for iMRI must be larger than a conventional OR to accommodate the MRI scanner, portable shield, and extra personnel.3
- To ensure the safety of all personnel and patients, the magnetic field and MRI scanner must be appropriately distanced from other OR equipment. An area outlined by a 5 Gauss (5-G) line demonstrates the perimeter within which the static magnetic field is higher than 5G.3 Outside of this perimeter, magnetic field exposure is less than 5G and is considered minimal risk to bystanders.3
- Only MR-safe devices should be used during iMRI to ensure patient and personnel safety. Ferromagnetic objects should remain at a specific distance from the scanner to avoid being attracted to the scanner, which can turn these objects into projectiles.
Patient Safety
- During iMRI, patients require the same standard American Society of Anesthesiology monitors, including electrocardiogram (ECG), blood pressure, heart rate, and pulse oximetry.
- MRI technology can create restrictions with the monitoring equipment, anesthesia machine, and medication delivery devices. Any object with ferromagnetic properties can become a projectile and poses injury risks to patients or staff in the OR.3
- Monitors and equipment utilized should be designed and labeled as MR-safe or MR-conditional to ensure patient and personnel safety.
- Please see the OA summary on MRI safety for more details. Link
- Metal objects and electronic monitors introduced into the MRI scanner, even if designated as MR-safe, can reflect or generate radiofrequency waves, which can result in distorted MR images.
- Both patients and OR personnel may benefit from foam earplugs to prevent hearing damage due to acoustic noise generated from the MRI machine, which can exceed 100 dB.3
- Patient temperature should be monitored during MRI procedures. MR imaging may lead to increased patient body temperatures, particularly in longer scans. However, sedation during MR imaging can lead to decreased body temperatures. In a study of 74 children undergoing MRI with anesthesia, only 5 had clinically relevant increases in body temperature greater than 0.5 degrees Celcius.4
Anesthesia Considerations
- During iMRI, there are additional safety challenges, and it is the role of the anesthesiologist to help promote patient safety, which may be compromised due to acoustic noise, a darkened environment, obstructed line of sight, and other distractions.3
- The anesthesiologist should perform a preoperative MRI compatibility examination and ensure that any acquired or implanted metallic devices within the patient are MR-safe.
- Standard ECG lead placement should be utilized, and the anesthesiologist must be trained to adjust electronic filters on the monitor to achieve noise-free signals as best as can be obtained. If a cardiac event is suspected during an iMRI, the patient should be removed from the MR scanner zone for accurate monitoring.3
- Anesthesia providers must also check on devices such as pulse oximeters and temperature probes, which may heat in the presence of the MR scanner and cause local burn injuries.
- Anesthesiologists must monitor pulse oximetry measurements and end-tidal CO2 monitors while the patient is in the MRI scanner. Clinical signs of ventilation, such as chest rise and breath sounds, are difficult to assess due to the lack of patient visualization and access.2
- MRI may interfere with standard monitoring and produce artifacts due to interference from magnetic fields, producing aberrant data. These may include ECG abnormalities, inaccurate pulse oximetry measurements, interruption of signal transmission, or falsely elevated temperature readings due to heating of a probe.
- Due to the possibility of artifacts, baseline measurements should be obtained in anesthetized or sedated patients.
- An extended circuit for ventilation and an extended tubing for drug administration is often necessary because the patient is moved further from the anesthesia machine while in the MRI scanner.
- Isoflurane, enflurane, halothane, and sevoflurane are MRI safe in both low and high-field MR environments. However, desflurane is not MRI safe.3 Sevoflurane is used most commonly because there are no MRI-safe or MRI-conditional desflurane vaporizers.
Other Safety Considerations
- Anesthesiologists often provide sedation or general anesthesia for patients undergoing MRI.
- Patient claustrophobia, anxiety, or inability to remain still within the MRI scanner for an extended period of time may necessitate the use of sedation or general anesthesia, as these conditions can compromise image quality and limit the diagnostic ability of the scan.
- MRI examinations in pediatric patients more commonly require sedation and general anesthesia due to its limitation of long acquisition times, enclosed environment, and loud noises. The ability to follow commands regarding limiting motion and breath-hold acquisitions are often more challenging in these patients.5
- Although sedation and general anesthesia are considered relatively safe, their use during MRI still poses potential risks, such as apnea from oversedation or allergic reactions to anesthetics.
- Inhalational anesthetics or infusion medications should be MR-safe and be administered through MRI safe/conditional anesthesia machines, vaporizers, and devices.
Strategies for Reducing Sedation During MRI
- Strategies to reduce the amount of sedation and general anesthesia during MR imaging can help promote patient safety while still obtaining high quality, diagnostic studies. Some of these strategies are presented in Table 1.5
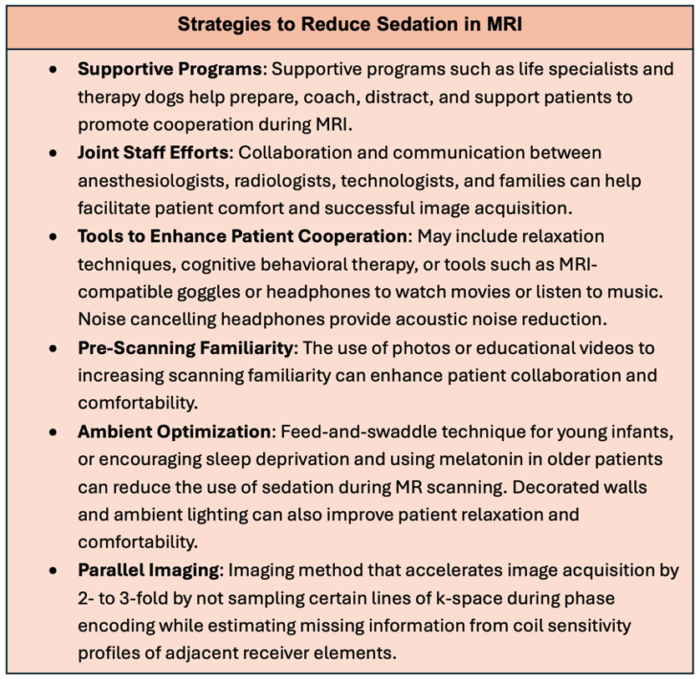
Table 1. Strategies to reduce sedation and mitigate anesthesia risks during MRI
References
- Berger A. Magnetic resonance imaging. BMJ. 2002; 324(7328):35. PubMed
- Henrichs B, Walsh RP. Intraoperative MRI for neurosurgical and general surgical interventions. Curr Opin Anaesthesiol. 2014; 27(4):448-52. PubMed
- Bergese SD, Puente EG. Anesthesia in the intraoperative MRI environment. Neurosurg Clin N Am. 2009; 20(2):155-62. PubMed
- Madsen TW, Sørensen MK, Cromhout PF, et al. Temperature change in children undergoing magnetic resonance imaging-An observational cohort study. Paediatr Anaesth. 2022; 32(7): 870-879. PubMed
- Artunduaga M, Liu CA, Morin CE, et al. Safety challenges related to the use of sedation and general anesthesia in pediatric patients undergoing magnetic resonance imaging examinations. Pediatr Radiol. 2021; 51(5):724-735. PubMed
Other References
- APSF Podcast. Episode #30 Airway Emergency Preparedness in MRI Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.