Copy link
Life Cycle Analysis in Anesthesiology
Last updated: 08/01/2023
Key Points
- Life cycle analyses (LCA) are a critical tool for evaluating the environmental impact of various medical products, processes, and medications.
- Utilization of a LCA allows health care workers and other stakeholders to understand and modify anesthetic plans based on these assessments to minimize long-term effects to the environment.
Rationale for LCAs
- The medical ethics principle nonmaleficence (primum non nocere, first do no harm) broadly includes the need to reduce health care-associated emissions, promote population health, and provide high quality care without unnecessary waste.
- Health care as it is currently practiced contributes significantly to greenhouse gas emissions and pollution, worsening the climate crisis and harming patients. Health care sector pollution and emissions are responsible for almost 5% of global emissions and contribute to excess morbidity and mortality.1,2
- Provision of health care is highly resource-intensive, and many have chosen to shift towards single-use disposable products for convenience and the notion that they may reduce infection (i.e., disposable plastic gowns, disposable laryngoscopes/blades, etc.) without full consideration of downstream effects such as environmental impact, and often without evidence of superiority.
- Many organizations have dedicated time and energy to minimizing the environmental impacts of medical treatments; however, significant challenges remain. Generation of waste is one of these challenges, as health care-generated waste is complex and expensive to manage, with over 6 million tons of waste generated annually.3
Methodology
- LCA assess the environmental impacts of a product or service throughout its entire life cycle (Figures 1 and 2). In the health care industry, LCAs are utilized to evaluate the environmental impacts of medical devices, pharmaceuticals, other health care products, and the delivery of health care services.4
- More broadly, LCA methodology can be applied to evaluate the environmental impacts of health care facilities, including the energy and water use associated with lighting, heating, and cooling, as well as the impacts of waste generation and disposal.
- Most LCAs have found that single use items contribute to higher emissions than reusable alternatives, though variables such as limited natural resources (i.e., water) and use of electricity from nonrenewable polluting sources can make reusable options less desirable.
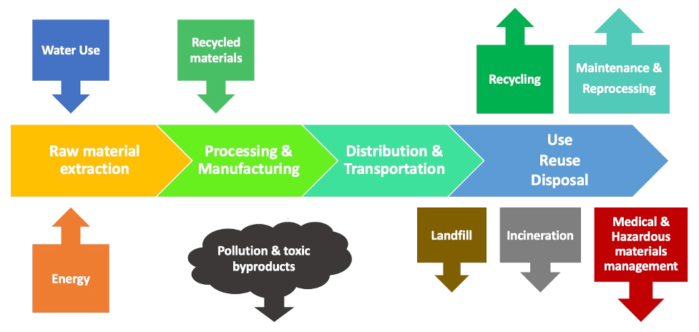
Figure 1. Schematic of a life cycle
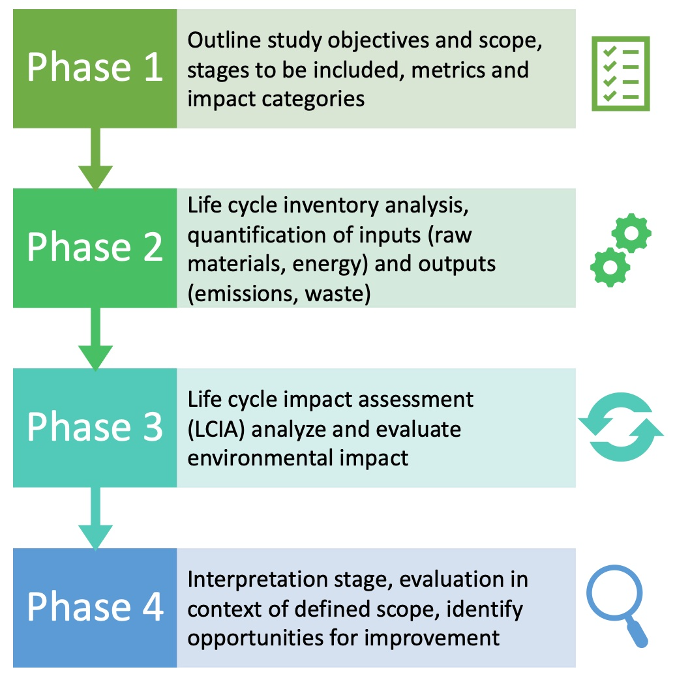
Figure 2. Four phases of standard LCA methodology
Selection of LCA Related to Anesthesia Care
Anesthetic Drugs5
- Desflurane has largest greenhouse gas (GHG) impact (15 times more than isoflurane, 20 times more than sevoflurane).
- Nitrous oxide (N2O) has large impact due to high global warming potential (GWP) and high concentration for clinical effect.
- Propofol infusion has a much smaller impact (1000 times less than desflurane or N2O).
Laryngoscope Handles and Blades6
- A single use disposable (SUD) plastic handle generates an estimated 16-18 times more carbon dioxide equivalents (CO2e) than reusable steel (low-level disinfection).
- A SUD plastic tongue blade generates an estimated 5-6 times more CO2e than reusable steel (high level disinfection).
- SUD metal components generated much higher emissions than all alternatives.
- Reusable handles are more economical than SUDs if they last through 4-5 uses, and reusable blades 5-7 uses, before loss.
Laryngeal Mask Airways (LMAs)7
- Reusable silicone LMAs were found to have a more favorable environmental profile than the disposable polyvinyl chloride LMAs. Reusable LMAs have a 7.4kg CO2e over their life cycle, compared to 11.3kg CO2e for 40 disposable LMAs.
- There is an impact from reusable LMA from washing and sterilization.
- There is an impact from disposable LMA from production (polymers), packaging, waste, etc.
- Discarding reusable LMAs prior to end of life should be avoided. There are about 40 uses or higher with proper handling).
- If using disposable LMAs, they should be purchased in bulk and high impact plastics (PVC) should be avoided.
Anesthesia Equipment (Airway Supplies, Breathing Circuits)8
- Reusable supplies have lower costs.
- Energy source determines much of the CO2 emissions from reusable equipment. This varies by country/region.
Limitations
- These analyses are specific to the location in which they are performed and use calculations that are derived from the availability of local resources, energy sources and waste streams. Therefore, the results may not be applicable to other facilities or geographic regions.
- In addition, regulations vary by country and region, and hospitals may have their own internal policies that must be considered. Readers should carefully analyze any LCA to determine how applicable it is to their region and institution and for any methodological assumptions or choices that may impact interpretation.
- It may be challenging to fully account for the downstream pollution associated with products or devices, for example, the impact of microplastics.
Gaps in Knowledge
- LCAs have been completed on a small subset of health care processes and products. There is a great need for expanded LCAs in health care, perioperative care, and anesthesia delivery.
- A database of health care LCAs9 has been created, but users must exercise caution as methodology can vary, and conclusions may not be broadly applicable.
References
- Health Care Without Harm: Josh Karliner and Scott Slotterback Arup: Richard Boyd, Ben Ashby, and Kristian Steele. Health Care’s Climate Footprint: How the Health Sector Contributes to the Global Climate Crisis and Opportunities for Action. Published September 2019. Accessed January 2023. Link
- Eckleman MJ, Sherman JD. Estimated global disease burden from US Health Care Sector greenhouse gas emisssions. Am J Public Health. 2018;108(S2): S120-22. PubMed
- Jenkins N. How to reduce waste by increasing use of reusable medical textiles. Supply Chain Strategies & Solutions. 6(2):6-8. Link
- Drew J, Christie SD, Tyedmers P, et al. Operating in a climate crisis: A state-of-the-science review of life cycle assessment withing surgical and anesthetic care. Environ Health Perspect. 2021; 129(7): 76001. PubMed
- Sherman J, Le C, Lamers V, et al. Life cycle greenhouse gas emissions of anesthetic drugs. Anesth Analg. 2012;114(5):1086-90. PubMed
- Sherman JD, Raibley LA 4th, Eckelman MJ. Life cycle assessment and costing methods for device procurement: Comparing reusable and single-use disposable laryngoscopes. Anesth Analg. 2018;127(2):434-43. PubMed
- Eckelman M, Mosher M, Gonzalez A, et al. Comparative life cycle assessment of disposable and reusable laryngeal mask airways. Anesth Analg. 2012;114(5):1067-72. PubMed
- McGain F, Story D, Lim T, et al. Financial and environmental costs of reusable and single-use anaesthetic equipment. Br J Anaesth. 2017;118(6):862-9. PubMed
- Drew J, Rizan C. Healthcare LCA (Online Database). Healthcare LCA. Published online 2022. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.