Copy link
Laryngeal Anatomy: Muscles and Innervation
Last updated: 05/24/2024
Key Points
- The larynx connects the oropharynx to the trachea, allowing for phonation and prevention of aspiration.
- All innervation to the larynx is from branches of the vagus nerve (cranial nerve X).
- The superior laryngeal nerve has an internal branch that provides sensory innervation to the glottis and vestibule and an external branch that provides motor innervation to the cricothyroid muscle. Innervation is for vocal cords and above the posterior pharynx area.
- The recurrent laryngeal nerve is the major motor nerve of the larynx, innervating all the intrinsic muscles of the larynx except for the cricothyroid muscle. It provides sensory innervation to all structures of the larynx below the glottis, including the subglottic mucosa. Innervation is below the vocal cords to the carina.
Introduction
- The larynx connects the oropharynx to the trachea and is bordered by the epiglottis superiorly and the cricoid cartilage inferiorly. The larynx is suspended from the hyoid bone.
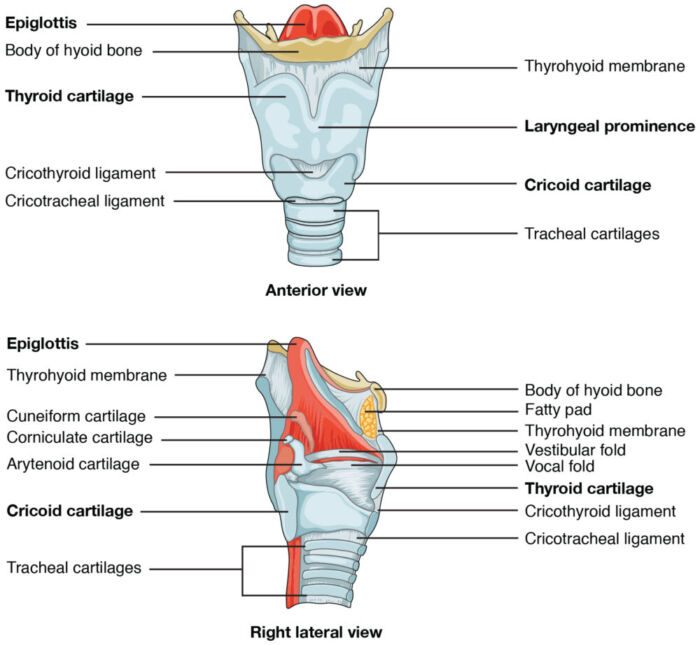
- The larynx comprises nine cartilage structures: three unpaired (epiglottis, thyroid, and cricoid cartilage) and three paired (arytenoid, corniculate, and cuneiform) cartilages. The cricoid cartilage is the only circumferential cartilage in the airway1 (Figure 1).
- The larynx’s functions are phonation (vocal cords) and prevention of aspiration (epiglottis and vocal folds).
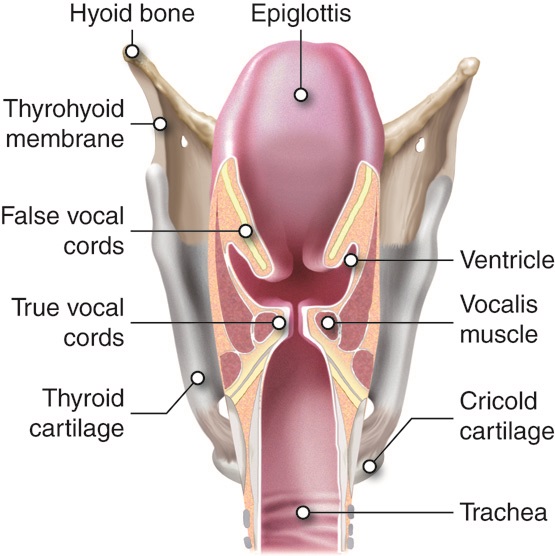
- The vocal cords meet at the anterior commissure anteriorly, attaching to the thyroid cartilage. They attach to the arytenoids posteriorly. The opening between the vocal cords is referred to as the rima glottidis. The part of the larynx above this is the vestibule, and below the glottis is the subglottis. The vestibular folds, also known as the false cords, are superolateral to the true vocal cords2 (Figure 2).
Laryngeal Innervation
- All the structures of the larynx are innervated by two branches of the vagus nerve (cranial nerve X), the superior laryngeal nerve and the recurrent laryngeal nerve (Figure 3).3
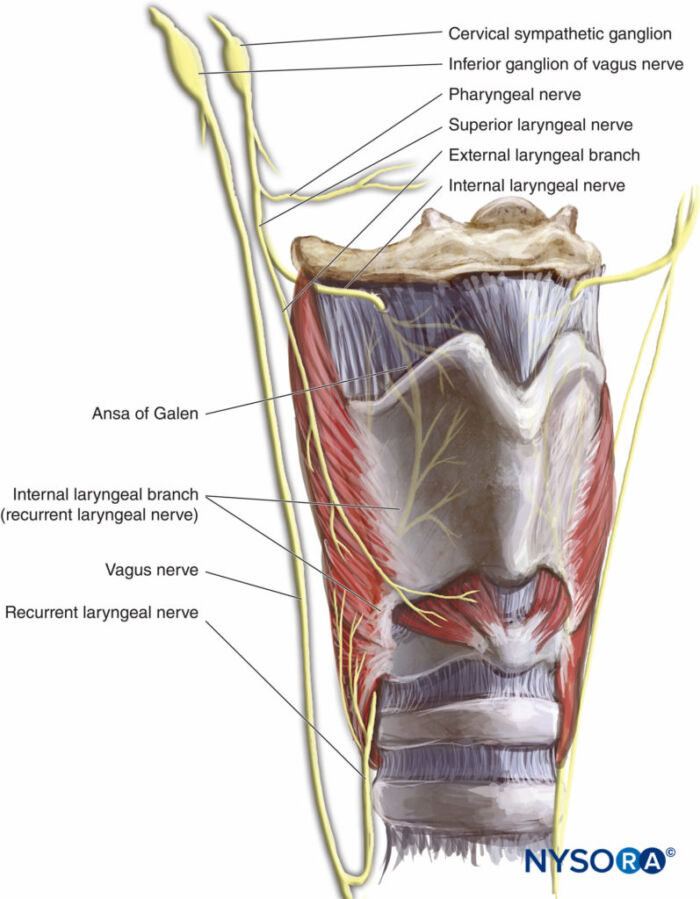
Figure 3. Innervation of the larynx. Source: NYSORA.com.4
- The superior laryngeal nerve is a branch of the vagus nerve that divides into internal and external branches (Figure 3).
- The internal branch of the superior laryngeal nerve provides sensory innervation to the epiglottis, laryngeal vestibule, and the superior surface of the vocal folds.
- This is the afferent limb of the laryngospasm reflex.
- The external branch of the superior laryngeal nerve provides motor innervation to the cricothyroid muscle.
- The internal branch of the superior laryngeal nerve provides sensory innervation to the epiglottis, laryngeal vestibule, and the superior surface of the vocal folds.
- The recurrent laryngeal nerve is another branch of the vagus nerve.
- It innervates all structures of the larynx that are not innervated by the superior laryngeal nerve.
- It is the primary motor nerve of the larynx, providing innervation to all the intrinsic laryngeal muscles except the cricothyroid muscle.
- It provides sensory innervation to the mucosa of the larynx below the vocal cords..
Laryngeal Muscles
- The intrinsic laryngeal muscles move the vocal folds and change their size, shape, and tension.3
- Tenses vocal ligaments (forceful speech): cricothyroid
- Adductor muscles: lateral cricoarytenoid, transverse and oblique arytenoid, thyroarytenoid muscles (Figure 4)
- Abductor muscles: posterior cricoarytenoid muscles (Figure 5)
- Extrinsic laryngeal muscles move the entire larynx. The suprahyoid muscles elevate the hyoid bone and the larynx during swallowing and vocalization. The infrahyoid muscles depress the hyoid bone and the larynx.
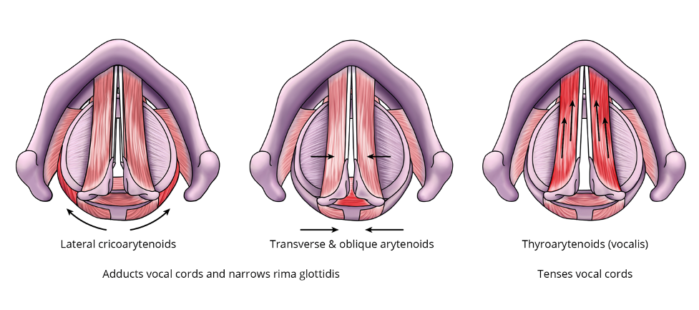
Figure 4. Adductors of the vocal cords
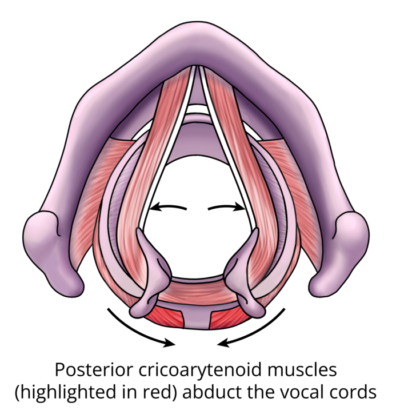
Figure 5. Posterior cricoarytenoid muscles (abductor of the vocal cords)
Clinical Correlates
Notable Landmarks4
- The larynx is located at the C3-C6 level.
- The cricoid cartilage is located at the C6 level.
- Laryngeal prominence, or “Adam’s apple,” is the anterior aspect of thyroid cartilage.
- The cricothyroid membrane is located between the thyroid and the cricoid cartilage. A needle cricothyroidotomy is often used for emergency front-of-neck access.
Recurrent Laryngeal Nerve Damage
- Recurrent laryngeal nerve damage can cause vocal cord paralysis, resulting in the affected vocal cord resting in the paramedian position.
- Unilateral vocal cord injury may cause a breathy voice and aspiration, though breathing is usually adequate.
- Bilateral vocal cord injury is usually iatrogenic and may compromise ventilation because both vocal cords are positioned near the midline. It may present as inspiratory stridor or respiratory distress.
Nerve Blocks5
- The superior laryngeal nerve (internal and external branches) can be anesthetized by injecting local anesthetic at the horn of the hyoid (Figure 6) or by placing lidocaine-soaked pledgets in the pyriform sinus.

Figure 6. Superior laryngeal nerve block. Source: NYSORA.com4

Figure 7. Translaryngeal nerve block. Source: NYSORA.com4
- Four percent lidocaine nebulizer can also be used to numb up the laryngeal area but is less effective.
- One can also spray lidocaine through the fiberoptic scope as it is being advanced.
- While performing an awake fiberoptic intubation, in addition to blocking the superior and recurrent laryngeal nerves, it will be helpful to minimize the gag reflex by blocking the glossopharyngeal nerve (cranial nerve IX). This can be done by injecting local anesthetic at the caudal aspect of the posterior tonsillar pillar bilaterally (Figure 8), having the patient gargle with viscous lidocaine, or placing a lidocaine lollipop far back in the patient’s mouth.
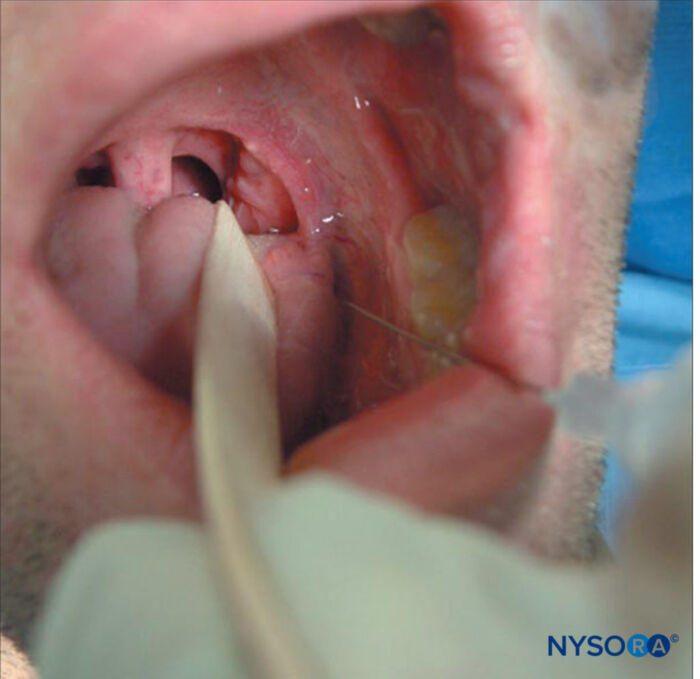
Figure 8. Glossopharyngeal nerve block. Source: NYSORA.com4
References
- Artime CA, Hagberg CA. Airway management in the adult. In: Gropper, MA et. al. Miller’s Anesthesia. Volume 1. Ninth edition. Philadelphia, PA; Elsevier; 2020: 1377-1387.
- Netter FH. Atlas of Human Anatomy. Fifth edition. Philadelphia, PA; Saunders Elsevier; 2011: 76-80.
- Moore, KL et al. Neck. In: Moore Clinically Oriented Anatomy. Seventh edition. Baltimore, MD. Lippincott Williams & Wilkins; 2014: 1022-1030.
- Burch, JM, Kamani, DV. Hoarseness in adults. UpToDate; 2024. Accessed 3/31/24. Link
- Ahmad, I. Regional and topical anesthesia for awake endotracheal intubation. NYSORA; 2024. Accessed 3/30/2024. Link
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.