Copy link
Intubation in the Critically Ill: Airway Management in Patients with a Physiologically Difficult Airway
Last updated: 07/18/2025
Key Points
- Intubation in critically ill patients is a high-risk procedure, with 45% of patients experiencing a major adverse event.
- The physiologically difficult airway is characterized by physiologic alterations that put the patient at an increased risk for cardiovascular collapse and other peri-intubation adverse events during tracheal intubation and transition to positive pressure ventilation.
- Hypoxic patients should be preoxygenated in the upright position with noninvasive positive pressure ventilation (NIPPV).
- To prevent hypotension, the dose of the induction agent should be decreased, administer a bolus dose of a vasopressor should be administered, or the patient should be intubated while awake.
Physiologically Difficult Airway
- Physiologically difficult airway describes patients with physiologic derangements that put them at high risk of adverse peri-intubation events. These airways can be considered difficult even though they pose no anatomic difficulty, and when tracheal intubation is successful on the first attempt.1
- Major adverse events occur frequently in this patient population. A recent prospective international study of nearly 3,000 intubations in critically ill patients identified an alarming rate of peri-intubation complications of 45%.2 These major adverse events include:
- hypoxia, which occurred in 9% of patients;
- hemodynamic instability, which occurred in 42.6% of patients; and
- cardiac arrest, which occurred in 3% of patients.
- Peri-intubation complications were associated with increased intensive care unit (ICU) admissions and 28-day mortality.3
- Patients with physiologically difficult airways are at risk of complications both during tracheal intubation and with transition to positive pressure ventilation due to limited tolerance of increased intrathoracic pressure.4
- Minimizing the risk of adverse events in patients with a physiologically difficult airway requires optimization of environmental and human factors. It is critical to minimize the number of attempts at tracheal intubation and maximize the chances of first-pass success.
- A timeout to ensure all necessary equipment is available and to clarify roles and backup plans can be helpful to minimize the risk of adverse events. Checklists have also been utilized to optimize the intubation procedure in these patients.
- Some groups have developed scoring systems to identify those with difficult airways and ensure the correct personnel and equipment are available for airway management.5
- Patients with physiologically difficult airways can be categorized into groups based on their physiologic derangements, with distinct strategies employed to minimize the risk of adverse events in each group. These categories include those with:
- Hypoxemia
- Cardiovascular instability
- Cardiac arrest
- Right ventricular dysfunction
- Obesity
- One technique that can be applied to patients presenting with a physiologically difficult airway is an awake intubation. Awake intubations can be performed using video laryngoscopy or flexible bronchoscopy. Benefits of awake intubation include:
- Maintenance of spontaneous respirations
- Avoidance of side effects of induction agents
- Maintenance of sympathetic tone and respiratory efforts
- An awake technique is unlikely to be effective in patients with severe agitation or those who require emergent airway management and cannot wait for airway topicalization.
Intubating the Hypoxic Patient
- Patients with a physiologically difficult airway due to hypoxia are at risk of desaturation during intubation, resulting in cardiac arrest.
- The optimal method of preoxygenation is NIPPV with positive end-expiratory pressure (PEEP), which delivers a high fraction of inspired oxygen, assists those with weak respiratory effort, and may open atelectatic alveoli.
- Preoxygenation in the upright position should be performed whenever possible. Preoxygenation is especially critical in patients with significant shunt or reduced functional residual capacity, such as those who are pregnant, obese, or have acute respiratory distress syndrome.
- Patients who are receiving a high fraction of inspired oxygen and high PEEP during preoxygenation are likely to have significant alveolar collapse upon removal of the bilevel positive airway pressure mask to facilitate intubation. Clinicians should be prepared to perform recruitment maneuvers to reopen atelectatic alveoli upon placement of the endotracheal tube.
- Preoxygenation should be performed for at least 3 minutes or 8 vital-capacity breaths.
- Patients who are obese and patients who are pregnant have significantly reduced functional residual capacity and are at high risk of hypoxia during the intubation procedure. Managing these two patient groups similarly to those presenting with hypoxia to minimize the risk of severe hypoxia and cardiac arrest should be considered.
- Some patients with hypoxia also present with agitation or delirium, which limits their ability to tolerate adequate preoxygenation. In these patients, a delayed sequence intubation can be helpful.
- To perform a delayed sequence intubation, a low dose of a sedating medication that does not depress respiratory efforts should be administered, such as ketamine or dexmedetomidine. Clinicians should be prepared to transition to an emergent intubation in case the patient becomes overly sedated or apneic.
- Apneic oxygenation may be beneficial to increase the safe apneic interval. Apneic oxygenation can be achieved using a nasal cannula at maximum flow rates or a high-flow nasal cannula. Apneic oxygenation will not replace adequate preoxygenation.6
- Critically ill patients who present with obesity have a higher incidence of severe hypoxemia in the peri-intubation period. Additionally, obesity has been associated with a higher rate of first-pass intubation failure, which elevates the risk of hypoxemia as the apneic time is prolonged.7 Therefore, in obese patients, clinicians should prioritize adequate preoxygenation and ensure the availability of backup equipment and experienced personnel prior to attempting intubation.
Intubating the Hypotensive Patient
- Patients who present with hypotension are at high risk of peri-intubation cardiac collapse. The etiology of cardiovascular collapse in the hypotensive patient requiring tracheal intubation is a combination of:
- underlying shock
- hypoxia
- acidosis
- transition to positive pressure ventilation and an increase in intrathoracic pressure
- vasodilatory or negative inotropic effects of induction agents; and
- adrenergic response blunting as a result of induction medications.
- In a large international observational study, 43% of critically ill patients had peri-intubation cardiac instability or collapse. Additionally, patients with peri-intubation cardiovascular instability or collapse had an increased risk of ICU and 28-day mortality.4
- Patients at a particularly high risk of hemodynamic collapse during intubation are those with right ventricular (RV) failure. Transthoracic echocardiography has been utilized to identify cardiac abnormalities, including RV dysfunction, and may provide critical information prior to an intubation.8
- Several strategies, including different induction agents, have been studied to minimize the risk of worsening hypotension and hemodynamic instability in the peri-intubation period.
- Administering a fluid bolus before intubation has not been found to be effective in preventing hemodynamic instability or cardiac arrest.
- Propofol has been associated with a higher risk of cardiovascular instability.3
- Etomidate is a hemodynamically stable agent; however, it has been associated with higher odds of hospital mortality, which is suspected to be due to the side effect of adrenal suppression.9
- Ketamine, as a sympathomimetic agent, has a favorable hemodynamic profile; however, it may have a direct myocardial depressant effect in patients whose catecholamine reserves have been depleted and may cause hypotension in the critically ill.
- Midazolam is a helpful sedative and amnestic that can be used to maintain hemodynamic stability.
- Most critically ill patients require much lower doses of induction agents than typically used in the operating room.
- An awake technique avoids the use of induction medications and allows for the maintenance of sympathetic tone during the intubation period. An awake technique may be the safest way to intubate a patient with RV failure.
Intubating the Neurologically Impaired Patient
- Patients presenting with altered mental status may have elevated intracranial pressure. In these patients, hypoxemia or hypercapnia could result in acute elevations in intracranial pressure and decreases to cerebral blood flow.
- Patients with elevated intracranial pressure should be positioned with the head elevated at 30 degrees.
- Induction agents that will preserve stable hemodynamics are preferable to minimize changes in cerebral perfusion.
- Ketamine was initially avoided due to concerns for side effects of increasing intracranial pressure; however, recent studies suggest it can be safely used in the neurologically injured patient.
- Agents such as opiates, lidocaine, or esmolol, which blunt the stimulation of intubation without significant hypotension, may be helpful.8
Intubating the Patient with Metabolic Acidosis
- Patients with severe metabolic acidosis will have higher ventilatory needs to clear carbon dioxide.
- Patients may already be maximally compensating for metabolic acidosis with increased ventilation. Any reduction in ventilation could therefore lead to worsening acidosis and cardiac arrest.
- Periods of reduced ventilation or apnea during intubation are poorly tolerated by patients with metabolic acidosis.
- Preoxygenation with NIPPV reduces the patient’s work of breathing and supports high ventilatory requirements.
- An awake intubation allows such patients to maintain spontaneous ventilation and avoids the apneic interval.
- There is no evidence to suggest the benefit of the administration of bicarbonate preintubation.6
Intubating the Patient in Cardiac Arrest
- In the patient who has suffered an in-hospital cardiac arrest, the etiology of the cardiac arrest should be considered before attempting to intubate.
- If a patient has a shockable rhythm or a cardiac etiology of arrest, minimizing interruptions to chest compressions and allowing defibrillation attempts should be the priority.
- If a patient presents with a hypoxic arrest or an aspiration, intubating and restoring oxygenation should be the priority.
- Airway management is more difficult in cardiac arrest, and first-pass success is lower.
- A high index of suspicion should be maintained for failed intubation.
- Continuous waveform capnography should be used to confirm endotracheal intubation and monitor cardiopulmonary resuscitation quality.8
Tips and Tricks
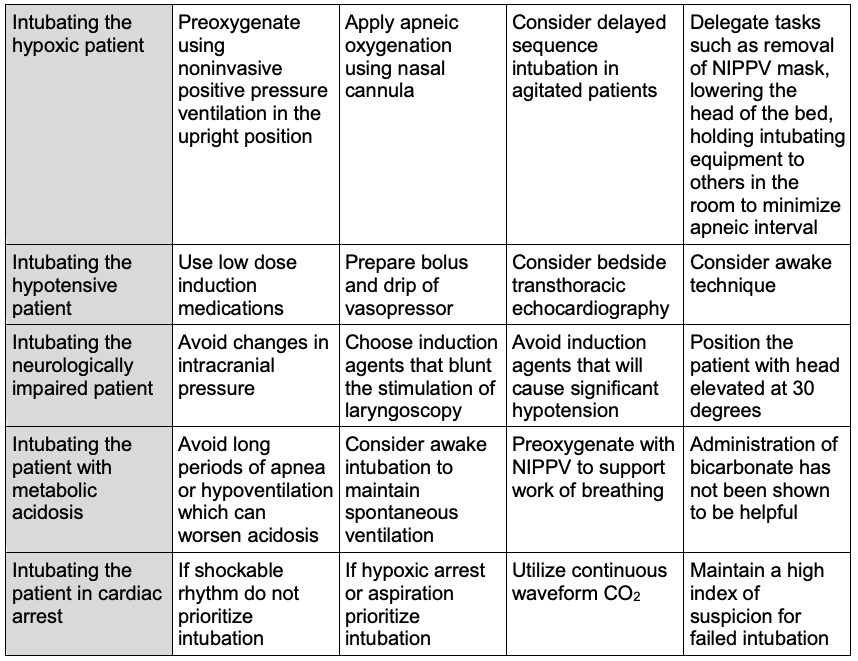
Table 1. Tips and tricks for intubating a patient with a physiologically airway
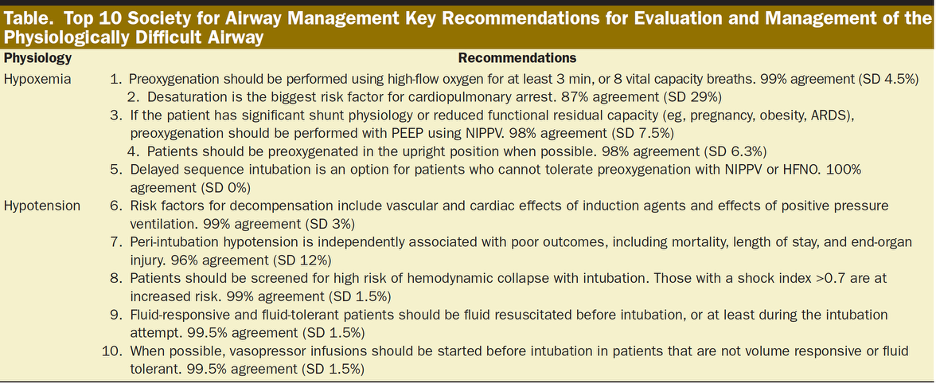
Table 2. Society for Airway Management key recommendations for evaluation and management of the physiologically difficult airway. Used with permission from Kornas RL, et al. Anesth Analg. 2021.6
References
- Myatra SN, Divatia JV, Brewster DJ. The physiologically difficult airway: an emerging concept. Curr Opin Anaesthesiol. 2022;35(2):115-21. PubMed
- Russotto V, Myatra SN, Laffey JG, et al. Intubation practices and adverse peri-intubation events in critically ill patients from 29 countries. JAMA. 2021;325(12):1164-72. PubMed
- Russotto V, Tassistro E, Myatra SN, et al. Peri-intubation cardiovascular collapse in patients who are critically ill: insights from the INTUBE study. Am J Respir Crit Care Med. 2022;206(4):449-58. PubMed
- Karamchandani K, Nasa P, Jarzebowski M, et al. Tracheal intubation in critically ill adults with a physiologically difficult airway. An international Delphi study. Intensive Care Med. 2024 ;50(10):1563-79. PubMed
- Karamchandani K, Wheelwright J, Yang AL, et al. Emergency airway management outside the operating room: current evidence and management strategies. Anesth Analg. 2021;133(3):648-62. PubMed
- Kornas RL, Owyang CG, Sakles JC, et al. Evaluation and management of the physiologically difficult airway: consensus recommendations from Society for Airway Management. Anesth Analg. 2021;132(2):395-405. PubMed
- Russotto V, Laffey JG, Tassistro E, et al. Peri-intubation complications in critically ill obese patients: a secondary analysis of the international INTUBE cohort. Crit Care. 2025 ;29(1):1-2. PubMed
- Budde AM, Tung A. Airway management during resuscitation. Int Anesthesiol Clin. 2023;61(4):9-14. PubMed
- Wunsch H, Bosch NA, Law AC, et al. Evaluation of etomidate use and association with mortality compared with ketamine among critically ill patients. Am J Respir Crit Care Med. 2024;210(10):1243-51. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.