Copy link
Initial Evaluation of Trauma Patients
Last updated: 01/12/2023
Key Points
- The initial management of the trauma patient requires a coordinated approach by a multidisciplinary team of specialists.
- The primary and secondary surveys are universal methods to provide efficient and effective care and evaluation in the trauma setting.
- The Glasgow Coma Scale (GCS) is a tool used to assess impairment of conscious level in response to defined stimuli.
Introduction
- Trauma is the leading cause of death of individuals younger than 45 years in the U.S and other developed nations. In the United States, trauma is the third leading cause of death in people of all ages.1
- Patients can present with a wide range of conditions resulting from a variety of traumatic mechanisms. Multiple organ systems may be involved, and the patient’s condition can be very labile and unpredictable. Thus, a systematic approach is required for the initial evaluation and management.
- The advanced trauma life support (ATLS)® course provides an algorithmic approach to evaluate trauma patients. These guidelines include a primary survey, secondary survey, and damage-control resuscitation. The 10th edition of ATLS® was published in 2018.2
Primary Survey
• The primary survey is designed as a quick diagnostic tool to rapidly assess and treat the most common life-threatening conditions in a trauma patient.2-4 (Figure 1)
• Conditions include massive internal or external hemorrhage, airway obstruction, tension pneumothorax, flail chest, cardiac tamponade, and increased intracranial pressure.
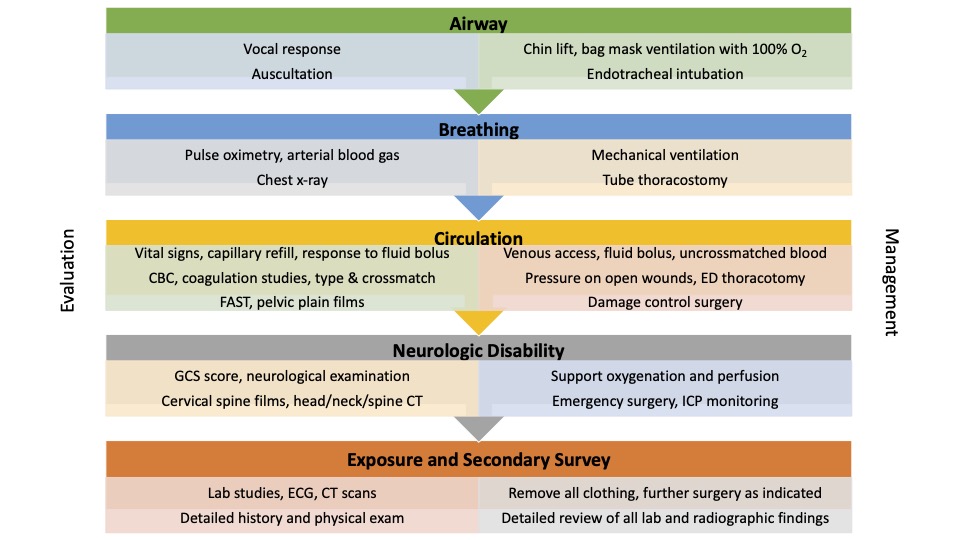
Figure 1. ATLS Primary Survey. Adapted from Galvagno SM, Steurer MP, Grissom TE. Anesthesia for Trauma. In: Gropper MA, et al (Eds). Miller’s Anesthesia. 8th edition. Elsevier, Philadelphia, PA: 2115-55.
Glasgow Coma Scale
- The Glasgow coma scale (GCS) allows the rapid evaluation of the trauma patient’s mental status and motor function (Table 1).5
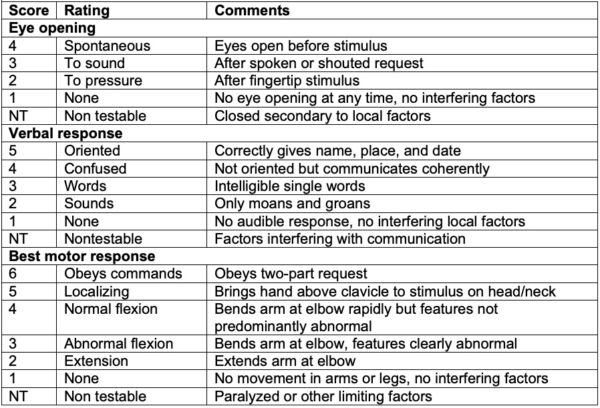
Table 1. Glasgow coma scale. Adapted from Institute of Neurological Sciences NHS Greater Glasgow and Clyde. Glasgow Coma Scale: do it this way.6
- Score from the three parameters are added to get a total GCS score that is often expressed as GCS (total #) = E(#)V(#)M(#). For example, GCS13 = E4V4M5.
- A GCS of less than 8 is an indication for endotracheal intubation; hence, the phrase “less than 8, intubate.” The highest GCS score (full consciousness) is 15, and the lowest GCS score (lack of consciousness) is 3.
- The updated version of GCS includes the following changes:6
- Pressure, rather than pain, should be used (if necessary) to evaluate eye opening. The three recommended sites for physical stimulation are fingertip pressure, trapezius pinch, and supraorbital notch pressure.
- In the verbal component, the terms “inappropriate words” and “incomprehensible sounds” have been simplified to “words” and “sounds.”
- In the motor component, the term withdrawal has been replaced with normal and abnormal flexion response. Abnormal flexion response includes slow stereotyped movements, movement of the arm across the chest (instead of away from the body), rotation of the forearm, clenching of the thumb, or leg extension.
- When an assessment cannot be completed (e.g., verbal response in intubated patient), the untestable component is designated as nontestable.
Secondary Survey
- The secondary survey is performed after the initial stabilization of the trauma patient, and is focused on obtaining a detailed history, performing a thorough head to toe examination, reassessing all the vital signs, and obtaining pertinent laboratory and imaging studies.3
- Step 1: Obtain a detailed history using the mnemonic AMPLE.
- Allergies
- Medications
- Past medical history, illnesses, pregnancy
- Last meal
- Environment and exposure to toxins
- Step 2: Obtain history of the event that caused injury and identify the mechanism of injury
- Step 3: Assess the head and maxillofacial region
- Step 4: Assess the cervical spine and neck
- Signs of blunt or penetrating injury, tracheal deviation, accessory respiratory muscle use
- Palpate for tenderness, deformity, swelling, subcutaneous emphysema, symmetric pulses
- Auscultate carotid arteries for bruits
- Restrict cervical spinal motion if injury is suspected
- Step 5: Assess the chest
- Signs of blunt or penetrating injury
- Auscultate lung fields, assess quality of respiratory excursions or accessory muscle use
- Percuss for hyperresonance or dullness
- Step 6: Assess the abdomen
- Inspect, auscultate, percuss, and palpate for signs of blunt or penetrating injuries or signs of internal bleeding
- Step 7: Assess the perineum, rectum, and vagina
- Only perform a rectal examination in selected patients (i.e., assessing sphincter tone or bowel wall integrity, looking for blood or bony fragments)
- Only perform a vaginal exam in selected patients
- Look for contusions, hematomas, lacerations to the perineum
- Assess for urethral bleeding
- Step 8: Perform a musculoskeletal assessment
- Inspect and palpate upper and lower extremities for signs of blunt or penetrating injury
- Assess pelvis for evidence of fracture and associated hemorrhage
- Palpate all peripheral pulses
- Inspect and palpate the thoracic and lumbar spine, while restricting spinal motion in patients with possible spinal injury
- Step 9: Perform a neurological assessment
- Reevaluate pupils
- Determine GCS
- Evaluate the upper and lower extremities for motor and sensory function
- Observe for lateralizing signs (i.e., paresis, plegia, hyperreflexia)
References
- World Health Organization. Global burden of disease. Accessed October 15th, 2022. Link
- American College of Surgeons Committee on Trauma. Advanced Trauma Life Support (ATLS) Student Course Manual, 10th ed, American College of Surgeons, Chicago. 2018.
- Galvagno Jr SM, Nahmias JT, Young DA. Advanced trauma life support Update 2019. Management and applications for adults and special populations. Anesthesiology Clin. 2019. 37(1):13-32. PubMed
- Fort AC, Zack-Guasp RA. Anesthesia for patients with extensive trauma. Anesthesiol Clin. 2020;38(1):135-48. PubMed
- Teasdale G, Maas A, Lecky F, et al. The Glasgow coma scale at 40 years: Standing the test of time. Lancet Neurol. 2014; 13(8): 844-54. PubMed
- Institute of Neurological Sciences NHS Greater Glasgow and Clyde. Glasgow Coma Scale: do it this way. Accessed October 17th, 2022. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.