Copy link
Hypokalemic Periodic Paralysis
Last updated: 06/10/2025
Key Points
- Hypokalemic periodic paralysis (hypoPP) manifests as the sudden onset of generalized paralysis in association with low serum potassium levels, precipitated by factors including cold, stress, trauma, infection, and surgery.
- Perioperative management includes assessment of disease severity, maintenance of normothermia, adequate pain control, avoidance of glucose-containing solutions, and monitoring of potassium levels.
- Potential association with malignant hyperthermia (MH) exists, and the use of triggering agents should be avoided if possible.
Introduction
- hypoPP is a rare channelopathy affecting sodium or calcium channels, typically with autosomal dominant inheritance, although sporadic mutations also occur.1-2 The disease has a prevalence of 1 in 100,000 and appears in the first or second decade of life. Attacks can occur once or several times throughout life.2
- The manifestation of the disease is a sudden onset of paralysis, either generalized or focal, that is associated with low serum potassium levels. The duration of paralysis can be short-lived or last several hours. Paralysis begins early in the morning or upon awakening in the middle of the night.3,4
- Attacks can be triggered under several circumstances, including prolonged rest after strenuous exercise, a carbohydrate-rich meal the day prior, viral illness, and inadequate sleep. Offending medications known to trigger an attack include beta agonists, corticosteroids, and insulin.1
Etiology and Pathophysiology
- Mutations in type I hypoPP are due to mutations in CACNA1S, a dihydropyridine-sensitive skeletal muscle calcium channel gene.3 This gene encodes for a protein involved in the interaction between dihydropyridine receptors (DHPR) and ryanodine receptors.4
- Mutations in type 2 hypoPP are related to mutations in SCN4A, a voltage-sensitive skeletal muscle sodium channel gene. The gene encodes a protein, NaV1.4, which is structurally similar to DHPR.4
- Regardless of the genotypical origin of the disease, paralysis occurs with hypokalemia. The defective sodium or calcium gene allows for an accessory flow of ions across skeletal muscle cell membranes.
- Potassium levels that fall below 3.0 mEq/L will paradoxically cause skeletal muscle fibers to undergo sustained depolarization, failure of excitation-contraction coupling and ultimately weakness due to inexcitable muscle.5–7
- Affected muscles include the proximal muscles. The diaphragm and muscles innervated by cranial nerves are usually spared.5 With severe attacks, respiration, ocular movements, and swallowing function can be affected.
- An association with MH has been reported; however, several cases of succinylcholine or halogenated agents being used without issue have been documented. It is recommended to avoid triggering agents until further evidence is available that suggests there is no possible association between hypoPP and MH.5
- The use of neuromuscular blocker agents should be done with caution. Depolarizing agents can potentially lead to weakness. Judicious use of nondepolarizing agents is advised.8
Anesthetic Considerations
Perioperative Considerations
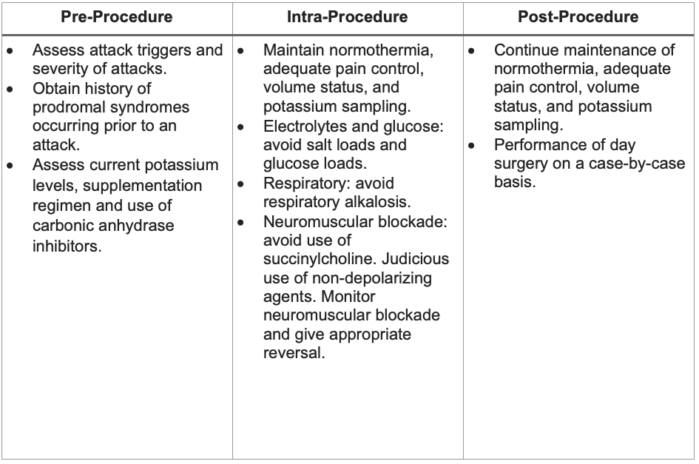
Table 1. Perioperative considerations in the care of patients with hypokalemic periodic paralysis3-5
Other Considerations
- Performance of a regional anesthetic is preferred. If general anesthesia is performed, avoidance of MH triggering agents is encouraged. Regional anesthesia allows for continued reporting of any changes in symptoms prior to the occurrence of an attack. Although there are reports of hypokalemia associated with spinal anesthesia, it has been safely performed.9
- Epinephrine and other beta-adrenergic agonists can result in hypokalemia, especially if added to local anesthetic mixtures during regional anesthetics.
- Insulin also lowers serum potassium levels, and it should be used with caution in patients with hypoPP.
- Minimizing severe acute pain is also critical, as stress hormones such as cortisol can lead to hypokalemia and trigger a paralytic attack.3
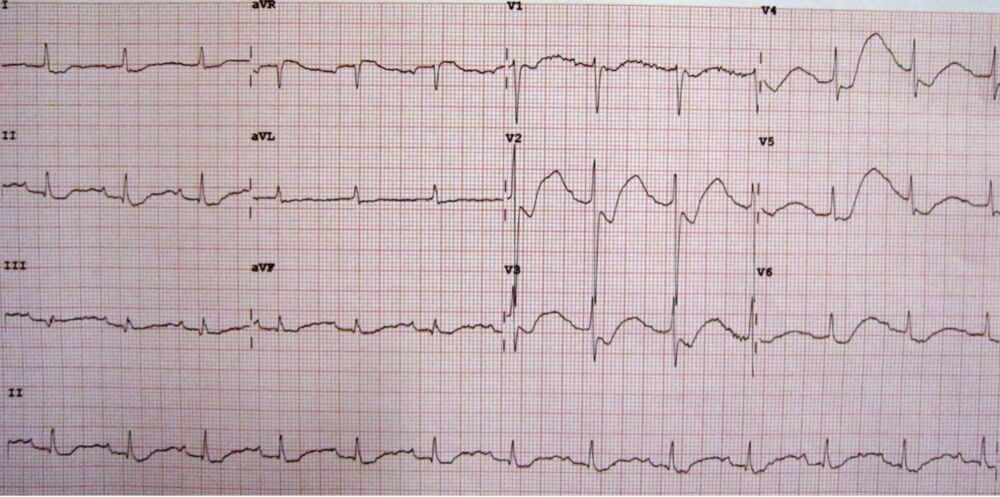
Figure 1. An electrocardiogram (ECG) of a patient with a potassium level of 1.1, showing the classical ECG changes of ST-segment depression, inverted T waves, large U waves, and a slightly prolonged PR interval. Source: Wikimedia Commons. James Heilman, MD, CC BY-SA 3.0 Link
Treatment of an Acute Attack
- Administration of oral or intravenous potassium until normalization of serum potassium1
- Supportive care in the case of respiratory muscle weakness4
Prevention of an Attack
- The ongoing prevention of attacks has been achieved through the use of carbonic anhydrase inhibitors. These diuretics induce potassium loss, but somewhat counterintuitively, they help reduce the frequency of paralytic attacks by poorly understood mechanisms.3
- Some patients also benefit from the use of a potassium-sparing diuretic such as spironolactone, either as monotherapy or in combination with a carbonic anhydrase inhibitor.3
References
- Lambert C, Blanloeil Y, Horber RK, et al. Malignant hyperthermia in a patient with hypokalemic periodic paralysis. Anesth Analg. 1994;79(5):1012-4. PubMed
- Venance SL, Cannon SC, Fialho D, et al. The primary periodic paralyses: diagnosis, pathogenesis and treatment. Brain. 2006;129(Pt 1):8-17. PubMed
- Fontaine B. Chapter 1 Periodic Paralysis. In: Advances in Genetics. Volume 63. Elsevier; 2008:3-23. PubMed
- Phuyal P, Bhutta BS, Nagalli S. Hypokalemic periodic paralysis. In: StatPearls (Internet). Treasure Island, FL. StatPearls Publishing; 2025. Accessed 5/14/2025. Link
- Bandschapp O, Iaizzo PA. Pathophysiologic and anesthetic considerations for patients with myotonia congenita or periodic paralyses. Paediatr Anaesth. 2013;23(9):824-33. PubMed
- Jurkat-Rott K, Weber MA, Fauler M, et al. K+-dependent paradoxical membrane depolarization and Na+ overload, major and reversible contributors to weakness by ion channel leaks. Proc Natl Acad Sci U S A. 2009;106(10):4036-41. PubMed
- Wang X, Nawaz M, DuPont C, et al. The role of action potential changes in depolarization-induced failure of excitation-contraction coupling in mouse skeletal muscle. Elife. 2022;11:e71588. PubMed
- Parness J, Bandschapp O, Girard T. The myotonias and susceptibility to malignant hyperthermia. Anesthesia and Analgesia. 2009;109(4):1054-64. PubMed
- Hecht ML, Valtysson B, Hogan K. Spinal anesthesia for a patient with a calcium channel mutation causing hypokalemic periodic paralysis. Anesth Analg. 1997;84(2):461-4. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.