Copy link
Hypercalcemia
Last updated: 04/30/2025
Key Points
- Hypercalcemia may result from increased bone resorption, increased gastrointestinal absorption, or reduced kidney clearance.
- Symptoms range from fatigue to arrhythmias, with a shortened QT interval being the hallmark electrocardiogram (ECG) finding.
- Treatment should include intravenous (IV) hydration, calcium-lowering agents, and targeted treatment of the underlying cause of hypercalcemia.
- Careful monitoring is needed during anesthesia due to the altered response to vasopressors, muscle relaxants, and fluid shifts.
Basics of Calcium Regulation & Hypercalcemia
- Calcium participates in various biochemical processes and is critical for heart function, bone strength, muscle contraction, and as a signaling molecule.1
- Calcium is regulated by three key hormones including1
- Parathyroid hormone (PTH)
- 1,25-dihydroxy Vitamin D3 (Vitamin D3)
- Calcitonin
- When serum calcium levels decrease, the parathyroid glands secrete PTH, which restores calcium levels by stimulating osteoclast-mediated bone resorption, enhancing renal calcium absorption, and stimulating the kidneys to produce Vitamin D3 to promote absorption in the intestines (Figure 1).1,2
- When serum calcium levels increase, calcitonin is released by the thyroid C cells to reduce calcium levels by inhibiting osteoclast activity, promoting calcium deposition into bone, and increasing excretion in urine (Figure 1).1,2
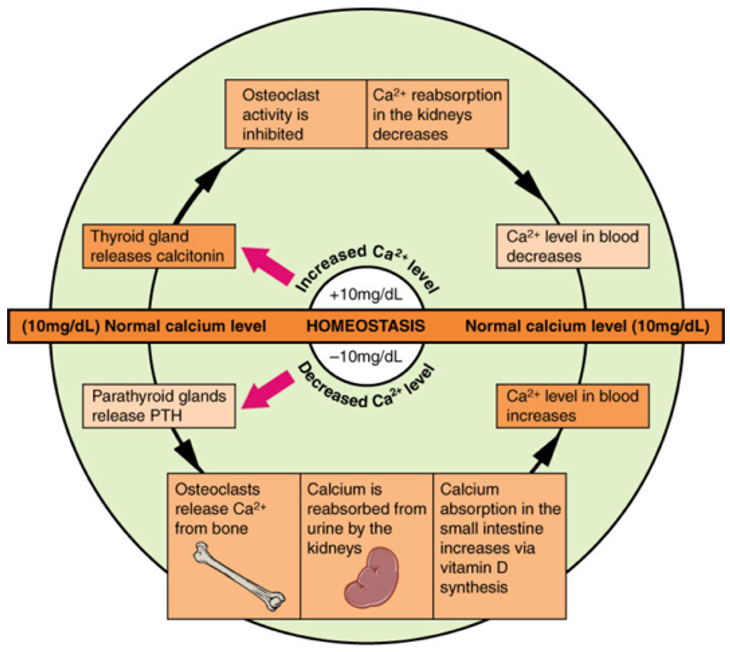
Figure 1. Hormonal regulation of calcium homeostasis. Source: Wikimedia Commons. Originally by Anatomy & Physiology, Connexions Website. CC BY 3.0.
Hypercalcemia
- The normal reference range for total serum calcium is 8.5 to 10.5 mg/dL.1
- Calcium also exists in its ionized (biologically active) form, which ranges from 4.8 to 5.6 mg/dL.1
- Values above these thresholds indicate hypercalcemia.
- Hypercalcemia can be classified by severity based on total serum calcium levels (Table 1).1
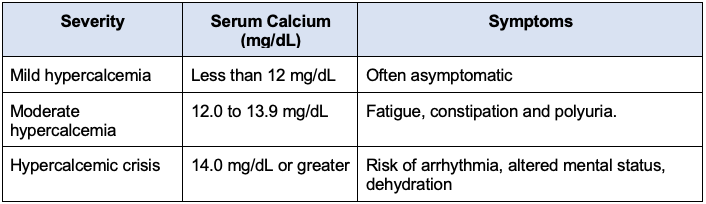
Table 1. Hypercalcemia: severity classification by serum calcium
Causes of Hypercalcemia
Diagnostic Laboratory Tests for Hypercalcemia
1. Serum Calcium
- Ionized calcium is the most accurate reflection of active calcium status.3
- Total calcium may require correction for albumin levels.3
2. Parathyroid Hormone
- Elevated PTH with high calcium suggests primary hyperparathyroidism.1,3,4
- Suppressed PTH suggests non-PTH mediated hypercalcemia (e.g., malignancy, Vitamin D excess).1,3
3. 24-hour Urinary Calcium and Calcium/Creatinine Clearance Ratio (UCCR)
- UCCR <0.01 → Suggests familial hypocalciuric hypercalcemia3
- UCCR >0.02 → Suggests primary hyperparathyroidism.3
4. Vitamin D (25(OH)D and 1,25(OH)2D)
- High 1,25(OH)2D with low PTH may point to sarcoidosis or lymphoma.3
- Vitamin D intoxication can also cause hypercalcemia.1,3
5. PTH-related Peptide
- Elevated in humoral hypercalcemia of malignancy.3,5
Common causes of hypercalcemia secondary to increased bone resorption, increased gastrointestinal absorption, and decreased renal clearance are listed in Tables 1-3.
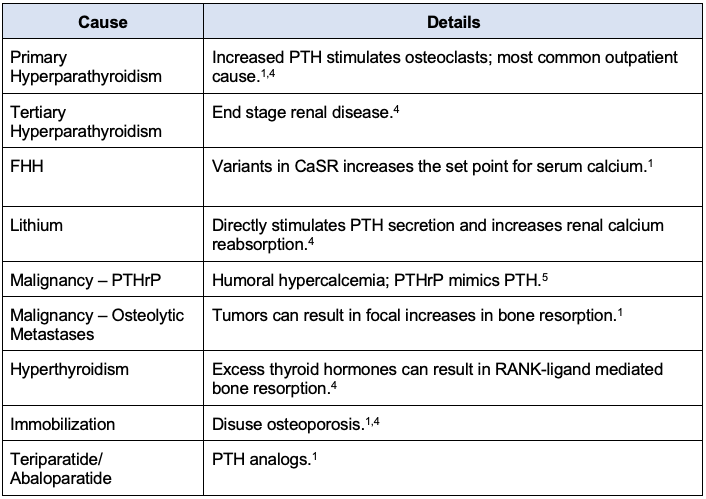
Table 2. Causes of hypercalcemia: increased bone resorption; Abbreviations: PTH, parathyroid hormone; CaSR, calcium-sensing receptor; PTHrP, parathyroid hormone-related peptide; RANK, receptor activator of nuclear factor-kappa B
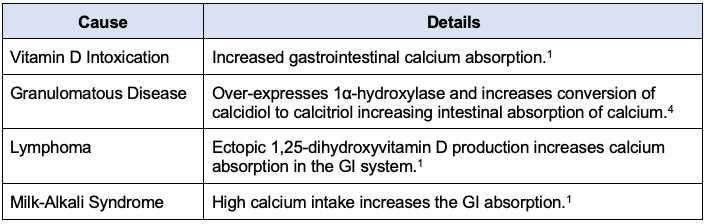
Table 3. Causes of hypercalcemia: increased gastrointestinal calcium absorption; Abbreviation: GI, gastrointestinal
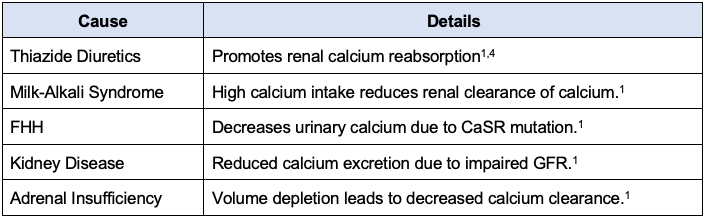
Table 4. Causes of hypercalcemia: reduced renal calcium clearance; Abbreviations: FHH, familial hypocalciuric hypercalcemia; CaSR, calcium-sensing receptor; GFR, glomerular filtration rate.
Clinical Presentation of Hypercalcemia
- Clinical manifestations can range from asymptomatic to serious complications depending on the acuity and severity.
- Early symptoms are often nonspecific, including fatigue, muscle weakness, and common gastrointestinal complaints such as nausea, constipation, and abdominal pain.1,4
- Altered mental status or lethargy may occur in severe cases.1
- Bone pain/fractures may be present due to increased bone resorption.1,4
- Renal calculi may develop.4
- On ECG, a shortened QT interval is the most characteristic finding.1
- Other changes, such as PR prolongation, widened QRS, or arrhythmias (bradycardia), can also be seen.1,4
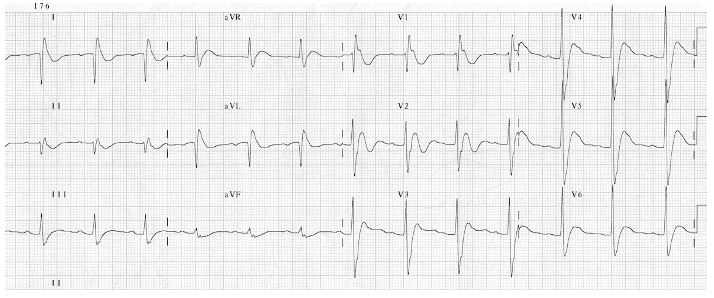
Figure 2. Electrocardiogram demonstrating shortened QT interval. Source: Life in the Fast Lane ECG Library. Link
Treatment of Hypercalcemia
Initial Management
- IV hydration (0.9% saline):
- First-line treatment is to correct volume depletion and promote urinary calcium excretion.6
- Initiation of calcium-lowering agents (Table 5):
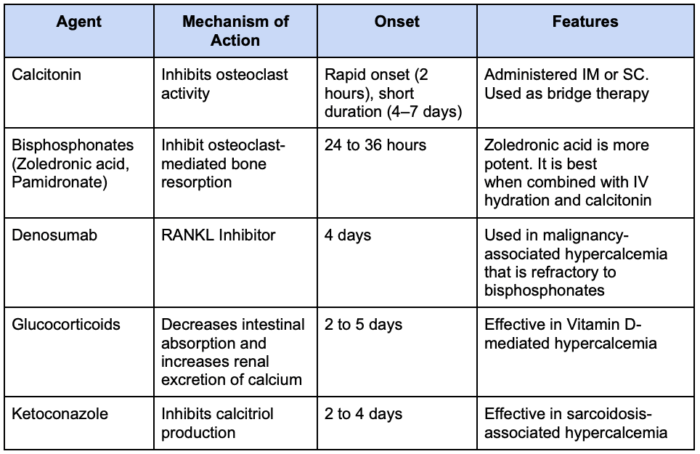
Table 5. Calcium-lowering agents1,4,7 Abbreviations: IV = intravascular, IM = intramuscular, SC = subcutaneous; RANKL, receptor activator of nuclear factor-kappa B ligand.
Targeted Therapies
1. Parathyroidectomy
- Indicated for primary hyperparathyroidism in patients who meet surgical criteria, such as:
- Serum calcium >1.0 mg/dL above normal1,6
- Osteoporosis or fragility fractures1,6
- Nephrolithiasis or hypercalciuria1,6
- Age <501,6
2. Cinacalcet
- Increases sensitivity of calcium-sensing receptors1,4
- Used in primary hyperparathyroidism in patients who are not surgical candidates1
3. Dialysis
- Considered in severe hypercalcemia with renal failure1,4,6
- Typically performed using a low or calcium-free dialysis solution1
Anesthetic Considerations of Hypercalcemia
- Hypercalcemia can cause arrhythmias, hypertension, and bradycardia.1,4
- Hypercalcemia causes volume depletion due to polyuria; therefore, perioperative rehydration with IV saline solution is an important initial step to restore volume imbalances.1,8
- High calcium levels may blunt the effect of β-adrenergic inotropes like epinephrine and dobutamine by interfering with adenylate cyclase, which can reduce the inotropic response.8
- Vasopressors that act independently of β-receptors, such as phenylephrine and amrinone, are usually unaffected.8
- In the setting of hypercalcemia, nondepolarizing muscle relaxants should be used with caution.8
- Their duration of action is often prolonged, especially in the presence of muscle weakness, although shortened duration has been reported with atracurium.8
- Starting with a lower initial dose, with subsequent titration, is recommended.8
- Volatile anesthetics may have less myocardial depressant effect in hypercalcemia, but caution is needed when used with calcium channel blockers.8
- Acidosis increases ionized calcium, and alkalosis reduces it by increasing protein-binding.
- Therefore, careful pH management is required during surgery to avoid calcium fluctuations that may affect cardiac and neuromuscular function.8
References
- Walker MD, Shane E. Hypercalcemia: A review. JAMA. 2022;328(16):1624–36. PubMed
- Babić Leko M, Pleić N, Gunjača I, Zemunik T. Environmental factors that affect parathyroid hormone and calcitonin levels. Int J Mol Sci. 2022;23(1):44. PubMed
- Meng QH, Wagar EA. Laboratory approaches for the diagnosis and assessment of hypercalcemia. Crit Rev Clin Lab Sci. 2015;52(3):107-19. PubMed
- Minisola S, Pepe J, Piemonte S, Cipriani C. The diagnosis and management of hypercalcaemia. BMJ. 2015;350:h2723. PubMed
- Mune T, Katakami H, Kato Y, Yasuda K, Matsukura S, Miura K. Production and secretion of parathyroid hormone-related protein in pheochromocytoma: participation of an alpha-adrenergic mechanism. J Clin Endocrinol Metab. 1993;76(3):757–62. PubMed
- Turner JJO. Hypercalcaemia - presentation and management. Clin Med (Lond). 2017;17(3):270-3. PubMed
- Adams JS, Sharma OP, Diz MM, Endres DB. Ketoconazole decreases the serum 1,25-dihydroxyvitamin D and calcium concentration in sarcoidosis-associated hypercalcemia. J Clin Endocrinol Metab. 1990;70(4):1090-5. PubMed
- Aguilera IM, Vaughan RS. Calcium and the anaesthetist. Anaesthesia. 2000;55(8):779-90. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.