Copy link
Hydralazine
Last updated: 10/14/2025
Key Points
- Hydralazine is a direct-acting vasodilator used to treat essential hypertension and, in conjunction with nitrates, heart failure.
- Due to hydralazine’s rapid arterial vasodilatory effects, it is considered a first-line antihypertensive in pregnancy or during a hypertensive emergency.1,2
Introduction
- Due to hydralazine’s rapid arterial vasodilatory effects, it is considered a first-line antihypertensive in pregnancy or during a hypertensive emergency.1,2
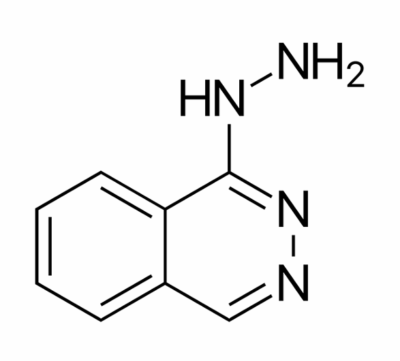
Figure 1. Chemical structure of hydralazine. Made with ChemDraw.
Pharmacokinetics and Mechanism of Action
- The exact mechanism of hydralazine is not fully understood, but it involves the inhibition of inositol triphosphate. This action prevents the release of calcium from the sarcoplasmic reticulum and inhibits myosin phosphorylation, thus preventing arterial smooth muscle cells from contracting.2
- Hydralazine’s actions lead to a decrease in peripheral vascular resistance, enabling the baroreceptor-mediated release of epinephrine and norepinephrine, which in turn leads to an increase in cardiac output and heart rate.
- Hydralazine undergoes hepatic metabolism, primarily undergoing acetylation via enzyme N-acyltransferase 2. Genetic acetylator status affects hydralazine levels, as slow acetylators exhibit a greater risk of adverse effects, especially the development of drug-induced lupus erythematosus (DILE) or acute liver injury.3,4
Dosage
- Hydralazine is available in oral and intravenous (IV) formulations.
- The half-life of oral hydralazine is 2 to 7 hours. In IV formulation, the half-life can be significantly decreased, less than 1 hour.2
- For hypertensive emergencies, 10mg of IV hydralazine is given with a maximum initial dose of 20mg and can be repeated every 4-6 hours as needed.2
- For essential hypertension, it is recommended to gradually increase from 10mg orally four times daily, to then 25mg four times daily for a few days until a week of treatment is complete. For maintenance therapy, the same dosage schedule can be used as long as the overall intake of hydralazine does not exceed more than 300mg per day.1,2
- For heart failure with reduced ejection fraction (HFrEF), it is recommended to give a fixed initial dose of 37.5mg hydralazine/20 mg isosorbide dinitrate (ISDN) 3 times daily.2,5
Clinical Uses
- Hypertension: Considered an option if hypertension is refractory to other first-line therapeutics. Hydralazine is often used in combination with beta-blockers or diuretics to mitigate the tachycardic baroreceptor response to a fall in blood pressure.1,2
- Hydralazine is considered a safe first-line agent as it has a rapid onset of action and can mitigate the development of a hypertensive emergency. During pregnancy and post-partum, IV hydralazine and labetalol are first-line therapy for acute onset, severe hypertension.2
- The reflex tachycardia associated with hydralazine administration contraindicates its usage in patients with coronary artery disease (CAD) (concern for type 2 myocardial infarction) and aortic dissection (counteracts impulse control, increases shear stress).2 This effect can be mitigated by coadministration or pre-treatment with beta-blocking agents.1
- HFrEF: In combination with ISDN, a potent venous vasodilator, a formulation of H-ISDN has been shown to improve left ventricular ejection fraction and decrease mortality rates.5 This combination attempts to mimic the increase in cardiac output seen with nitroprusside with orally available agents.6
Contraindications
- CAD: Hydralazine’s ability to trigger reflex sympathetic activation leads to an increase in myocardial contractility, heart rate, and oxygen demand. These effects can precipitate myocardial ischemia or worsen angina in patients with CAD.1,2
- Aortic dissection: Hydralazine causes a rapid drop in afterload and can worsen an aortic dissection as shear stress and force increase on the vessel wall.
- Systemic lupus erythematosus (SLE): Hydralazine at high doses, over long durations, or in individuals classified as “slow acetylators” are at risk of developing drug-induced lupus, where symptoms resemble SLE but typically spare the kidneys and central nervous system.4
Side Effects and Toxicity
- The most common side effects include flushing, headaches, palpitations, and tachycardia. These are due to reflex sympathetic activation.1,2
- DILE usually occurs with over 6 months of continuous use and is a dose-dependent effect. These symptoms typically regress with discontinuation of the drug.4
Special Considerations
- Beta-blocking agents or diuretics can be used as an adjunct to hydralazine therapy to mitigate the physiological effects of reflex sympathetic activation.1
- A complete blood count and an antinuclear antibody titer should be obtained prior to starting hydralazine and periodically throughout treatment to prevent lupus-like effects.4
References
- Herman LL, Bruss ZS, Tivakaran VS. Hydralazine. In: StatPearls. Treasure Island (FL). StatPearls Publishing; 2023. Accessed July 20, 2025. PubMed
- McComb MN, Chao JY, Ng TMH. Direct vasodilators and sympatholytic agents. J Cardiovasc Pharmacol Ther. 2015;21(1):3-19. PubMed
- LiverTox: Clinical and research information on drug-induced liver injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Hydralazine. Link
- He Y, Sawalha AH. Drug-induced lupus erythematosus: an update on drugs and mechanisms. Curr Opin Rheumatol. 2018;30(5):490-497. PubMed
- Ziaeian B, Fonarow GC, Heidenreich PA. Clinical effectiveness of hydralazine-isosorbide dinitrate in African-American patients with heart failure. JACC Heart Fail. 2017;5(9):632-639. PubMed
- Cole RT, Kalogeropoulos AP, Georgiopoulou VV, et al. Hydralazine and isosorbide dinitrate in heart failure: Historical perspective, mechanisms, and future directions. Circulation. 2011;123(21):2414-22. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.