Copy link
Hepatorenal Syndrome
Last updated: 04/09/2024
Key Points
- Hepatorenal syndrome (HRS) is observed as progressive renal impairment in the setting of advanced liver disease.
- Approximately 25% of patients admitted to the hospital with cirrhosis exhibit impaired renal function.
- Diagnosis requires the exclusion of other causes of intrinsic kidney disease.
- Treatment options include the use of vasoconstrictors, renal replacement therapy, and liver transplantation.
Introduction
- A diagnosis of HRS is associated with a high incidence of morbidity and mortality.
- HRS manifests as a functional failure of compensatory mechanisms in maintaining renal perfusion in the setting of systemic vascular dilatation and hypotension.
- Approximately 25-30% of patients with cirrhosis develop some form of acute kidney injury (AKI) during an acute decompensation event.1
- HRS has been described in two primary forms: a faster onset, acute kidney injury type (Type I-AKI) and a slower onset, chronic kidney disease type (Type II-CKD). Type I carries a worse prognosis.1
- Treatment focuses on establishing an appropriate circulating volume while minimizing further damage from nephrotoxic medications. Medical therapies include the use of vasopressors, while surgical interventions, including transjugular intrahepatic portosystemic shunt (TIPS) placement and liver transplantation, are also options.
- Morbidity and mortality remain high despite these efforts.2
Pathogenesis
- Portal hypertension associated with advanced cirrhosis triggers splanchnic and systemic vasodilation due to the circulation of multiple vasodilatory factors, including nitric oxide (NO), carbon monoxide (CO), prostacyclin, and endocanabinoids.3
- The reduction in systemic vascular resistance (SVR) and decrease in renal perfusion activates the body’s compensatory mechanism to maintain normotension and organ perfusion through the renin-angiotensin-aldosterone system (RAAS) (Figure 1).
- Aldosterone increases sodium and water retention in the nephron, while angiotensin aids in the compensatory systemic vasoconstrictive response.
- Unfortunately, RAAS activation also results in renal vasoconstriction, further reducing renal blood flow. In the early stages of cirrhosis, this renal vasoconstriction is counterbalanced by local renal vasodilators, leading to the maintenance of adequate renal perfusion.2
However, with further progression of portal hypertension, the action of circulating vasoconstrictors may overcome these compensatory mechanisms leading to the development of HRS.
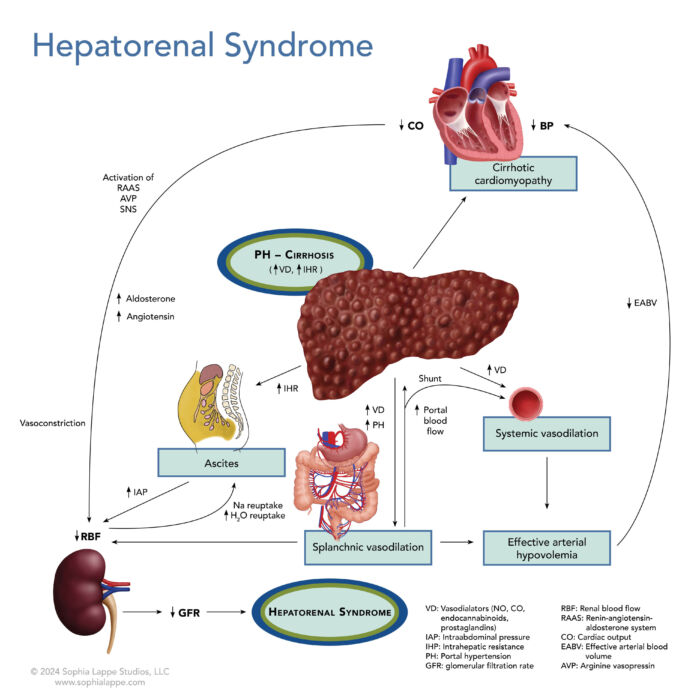
Figure 1. The interaction of factors leading to the development of HRS
Diagnosis2
- HRS is a diagnosis of exclusion and requires several criteria to be met. There must be ongoing deterioration of renal function in the presence of advanced liver disease. Other identifiable causes of kidney disease or dysfunction must also be ruled out or absent (Table 1).
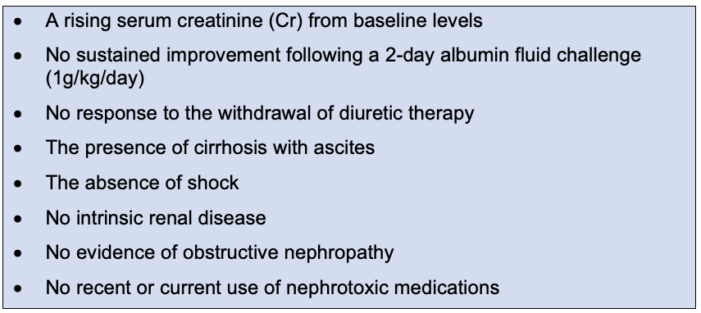
Table 1. Diagnostic criteria required for a diagnosis of HRS
Types of HRS
- The classification of HRS has undergone several changes over the last two decades. However, for this summary, there are two main presentations: a rapidly progressive version (Type I-AKI) and a slower, more insidious one (Type II-nonAKI/CKD).3
- Type I HRS-AKI3
- Rapid and life-threatening impairment of renal function with serum creatinine (Cr) rising 0.3 mg/dL within 48 hours OR an increase from baseline serum Cr levels by 1.5 mg/dL in the last three months
- It is often initiated by spontaneous bacterial peritonitis (SBP), large-volume paracentesis without adequate volume expansion, or gastrointestinal bleeding.
- Carries a poor prognosis without treatment, with a median survival of 2 weeks
- Type II HRS-nonAKI/CKD3
- Gradual deterioration in renal function leads to a slow rise in serum Cr to <1.5x baseline.
- Glomerular filtration rate assessed as <60mL/min/1.73m2 over three months
- It is often associated with diuretic-resistant ascites.
- Carries a better prognosis with a median survival of 5-6 months
Management
- Patients with HRS should be cared for in an intensive care unit (ICU) with consideration for special monitoring techniques, such as intra-arterial and central venous pressure measurements, to guide volume expansion with albumin. The aim is the return of an effective arterial blood volume (EABV).
- The mainstay of pharmacologic treatment is the use of vasoconstrictors. Medications commonly used worldwide are vasopressin analogs (e.g., terlipressin), norepinephrine, midodrine, and somatostatin analogs (e.g., octreotide). Terlipressin has more specific actions at the splanchnic bed and is the better option, but there are currently limitations regarding its availability and use.
- TIPS has also been shown to be successful in some patients with HRS by reducing portal hypertension and decompressing the splanchnic bed. Splanchnic venous pooling is then redirected to the systemic circulation, thereby reducing activation of the RAAS.2,3
- Long-term prophylactic antibiotic use can help prevent spontaneous peritoneal peritonitis (SBP) and reduce the chance of decompensation.
- Renal replacement therapy is helpful in the short-term management of the unresponsive HRS patient and as a bridge to liver transplantation.2,3
- Liver transplantation is the definitive treatment, and patients should be assessed early in the progression of their disease. However, the presence of HRS at the time of transplantation is associated with increased morbidity and mortality.2,3
Prognosis
- The onset of renal failure in patients with advanced liver disease is very serious, with delays in diagnosis and treatment leading to rapid, early death. Without effective treatment, most patients usually die within a few weeks or months, so close monitoring of at-risk patients while on the transplant list is paramount.
- Liver transplantation may often be curative for this type of renal failure.
References
- Amin AA, Alabsawy EI, Jalan R, Davenport A. Epidemiology, pathophysiology, and management of hepatorenal syndrome. Semin Nephrol. 2019;39(1):17-30. PubMed
- Cárdenas A, Arroyo V. Hepatorenal syndrome. Ann Hepatol. 2003;2(1):23-9. PubMed
- Simonetto DA, Gines P, Kamath PS. Hepatorenal syndrome: pathophysiology, diagnosis, and management. BMJ. 2020;370:m2687. PubMed
Other References
- UpToDate: Hepatorenal syndrome: Pathogenesis and clinical presentation. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.